
Your performance this year will affect your Medicare payment in 2019.
Fam Pract Manag. 2017;24(1):12-15
Author disclosure: no relevant financial affiliations disclosed.
The world of physician payment was turned upside-down with passage of the Medicare Access and CHIP Reauthorization Act (MACRA) in April 2015. Since then we have been learning the ins and outs of the law and emerging regulations that will transform Medicare physician payment. Additional details were released in October 2016, when the final rule was published in the Federal Register,1 so this article continues our previously published article on “Making Sense of MACRA.”2
First, a brief recap: The passage of MACRA repealed the “unsustainable” sustainable growth rate formula, which was set to cut physician Medicare payments by 21 percent in 2015. The legislation established two new tracks for payment, the Merit-Based Incentive Payment System (MIPS) and the Alternative Payment Model (APM). It created strict criteria for entry into APMs and outlined a scoring system for MIPS. The proposed rule released by the Centers for Medicare & Medicaid Services (CMS) in April 2016 gave names and definitions to the programs described in the legislation, proposed further criteria for participation in the newly named Advanced Alternative Payment Model (AAPM) track and scoring criteria for MIPS categories, and named the two tracks the Quality Payment Program (QPP).
The final rule solidified what was proposed and provided a better understanding of exactly what to expect in the future, which is coming sooner than you might think. Although you won't be paid under MIPS or the AAPM track until 2019, your performance for that payment year begins in 2017. You can choose the extent of your participation in MIPS for the first performance period through the CMS “Pick Your Pace” program, which provides the options described and depicted below:
“Test” the program. Ensure that your system is working and you are ready for further participation by submitting at least one measure of quality or one improvement activity or the required advancing care information (ACI) measures to CMS. With this option there is no negative payment adjustment.
“Partially” participate. Report more than one quality measure or more than one improvement activity or more than the required ACI measures for at least 90 days. This could earn you a small positive adjustment, and you would be exempt from a negative adjustment.
“Fully” participate. Report all required quality measures and improvement activities and ACI measures for at least 90 days. This could earn you a positive adjustment based on your MIPS final score, and you would be exempt from a negative adjustment.
Don't participate. You will receive the maximum negative payment adjustment.
Participate in the AAPM track if you qualify. This option will be described later in the article.
PICK YOUR PACE
The Merit-Based Incentive Payment System (MIPS) path of the Quality Payment Program offers three participation options for 2017. The size of your payment in 2019 will depend both on how much data you submit and on your performance results.
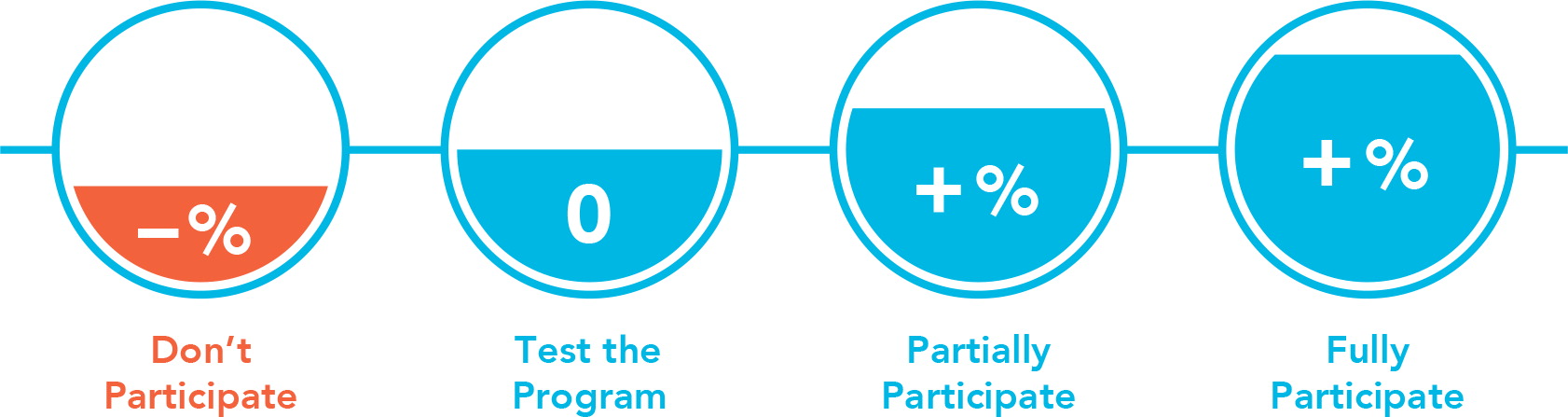
| Don't Participate | Test the Program | Partially Participate | Fully Participate |
| If you don't submit any 2017 data, you will receive a negative payment adjustment of -4 percent. | If you submit a minimum amount of 2017 data (e.g., one quality measure), you will be exempt from a negative payment adjustment. | If you submit more than the minimum amount of 2017 data for 90 days (e.g., more than one quality measure), you could earn a small positive payment adjustment and you will be exempt from a negative adjustment. | If you submit all required 2017 data for 90 days, you could earn a larger positive payment adjustment and you will be exempt from a negative adjustment. |
Again, your performance in 2017 will determine your payments in 2019, so it is imperative to identify the best approach for you and your practice (see the CMS resource for more details). To partially or fully participate, you must start collecting data by Oct. 2, 2017. Reporting on that data will begin in 2018 and must be completed by March 31, 2018. Participating now will also prepare your practice for 2018, when full-year reporting for cost and quality will be required.
MIPS track
Most physicians initially will participate in MIPS, which is based on existing activities with few entry requirements or exceptions, making it easy to become a participant. MIPS-eligible clinicians (ECs) will be scored on quality, cost (referred to as “resource use” in previous versions of the regulations), ACI (based on meaningful use requirements), and improvement activities (previously referred to as clinical practice improvement activities). Primary care physicians have been doing at least some, if not much, of what is required in each of these categories.
Scores in each category will be added together in a weighted fashion to make a final score, from 0 to 100, which will be compared to a “performance threshold.” If you score above the threshold, you will receive a sliding scale positive adjustment; if you score below, you will receive a sliding scale negative adjustment. Only those at the threshold get no adjustment. If you score in the lowest quartile, you will receive the maximum penalty for that payment year. All adjustments are budget neutral; the negative adjustments and positive adjustments for all participating physicians must balance each other. All adjustments will be made only to Medicare Part B claims.
Quality. You are required to report six quality measures, one of which must be an outcomes measure (see the complete list). You may report more than the six required measures, and in that case CMS will only use the six highest scoring measures. In addition to the six self-reported measures, CMS will calculate one population-based measure from claims data. The All Cause Hospital Readmission measure has been selected as the population measure, and it will be calculated only for those in groups of 16 or more clinicians with a minimum measure case size of 200.
Scoring. Each measure submitted will score points. Your performance on the measure is then compared to peers submitting the same measure and compared to a benchmark. Benchmarks are taken from data two years prior to the performance period (i.e., 2015 benchmarks for performance period 2017). Each benchmark is then broken down into performance deciles, and the decile where you fall will determine how many points are awarded for the measure. Scores in the top decile are automatically awarded the full points. You can earn bonus points for reporting extra measures for outcomes and patient experience and other high priority measures defined by CMS. Bonus points are also available for measures that are submitted using end-to-end electronic reporting. For a measure to receive a score, it must meet a minimum case size of 20 patients. Submitted measures that do not meet the minimum case size will not be scored on performance but will receive a baseline score of three points.
Data submission. You can submit quality data as an individual or as a group through qualified clinical data registries (QCDRs), qualified registries, electronic health record systems (EHRs), claims, and the CMS web interface. With submission through QCDR, qualified registries, and EHRs, you must report on 50 percent of your patients, regardless of payer. Submission via claims requires reporting on 50 percent of the Medicare Part B patients seen in the performance period. Submission through the CMS web interface requires reporting on all measures in the measure set using the first 248 consecutively ranked and assigned Medicare beneficiaries in the order they appear on the CMS web interface. If there are not 248 beneficiaries, groups must report 100 percent of the beneficiaries assigned to them.
Cost. In 2017, the cost category will not receive a score. However, beginning in 2018, cost measures will be automatically calculated by CMS. No data submission is required. Most of these measures are triggered by an inpatient evaluation and management code or specific procedure code; however, the measures of Medicare spending per beneficiary and total cost of care will apply to anyone who meets the minimum case size of 35 patients and 20 patients, respectively. Each measure that meets the minimum case size requirement will be awarded points and compared to a benchmark. The benchmarks are broken into deciles, and the points awarded for each measure will depend on where in the decile the performance falls.
Unlike the quality category, where the benchmark is based on a two-year look-back period, the cost performance category bases the benchmark on the actual performance period. This is because CMS realizes changes in payment policy make it challenging to compare cost across performance periods.
The cost score will be the average of the scores of eligible measures. The cost category will make up 10 percent of the final score in performance year 2018 and 30 percent in 2019 and subsequent years. In those years, if no score is obtained (i.e., because you did not meet the minimum case size in any measure), the cost category points will be redistributed to quality.
ACI. The ACI category is much like meaningful use. To get full credit for this category, you must first attest to several statements:
That you are using 2014 or 2015 edition certified EHR technology (CEHRT),
That you will participate in good faith with CEHRT surveillance when requested,
That you support information exchange,
That you will avoid information blocking.
The ACI score is broken down into a base and a performance score, each accounting for half of the total score. To earn full credit for the base score (and to receive any credit for ACI), you must either attest “yes” or submit a numerator and denominator for four or five measures, depending on the edition of your CEHRT. (See the complete list.) Failure to meet requirements for even one of the base score measures results in a score of zero for the base score and ultimately a zero for the entire ACI category. If a base score is achieved, a performance score is calculated based on how well you perform on the ACI performance measures and whether any bonus points are achieved. Bonus points are available for specified public health and syndromic surveillance reporting or for using CEHRT to perform a handful of MIPS improvement activities.
You can submit ACI data as an individual or as a group through a qualified registry, EHR, QCDR, attestation, or the CMS web interface. Hardship exclusions are available for those with insufficient Internet connectivity, extreme and uncontrollable circumstances, “lack of control” over the availability of certified EHR technology (as defined by CMS), and lack of face-to-face patient interaction. These exclusions must be filed annually.
Improvement activities. Improvement activities are exactly what they sound like – activities you can do within your clinic to improve your practice and the care to your patients. This is the “new” category for MIPS, but the activities are not new to family medicine and primary care in general. In fact, if your clinic is a medical home recognized by the National Committee for Quality Assurance, the Accreditation Association for Ambulatory Health Care, the Joint Commission on Accreditation of Healthcare, URAC, a regional or state program, a private payer, or another body that administers patient-centered medical home recognition to 500 or more clinicians, you will automatically be awarded full credit for this performance category. Practices participating in the CMS Comprehensive Primary Care Plus (CPC+) initiative but do not qualify for the AAPM bonus also get full credit for this category.
There are 92 improvement activities to choose from and no official measurement, just a requirement to carry out the chosen activity for a minimum of 90 days and submit attestation through a qualified registry, EHR, QCDR, attestation, or the CMS web interface.
Each activity carries a specified number of points, which are compiled to achieve the total score. Participation in an AAPM (excluding CPC+) that does not qualify for the bonus payment means receiving half the credit for this performance category. If you are in a small practice (15 or fewer professionals), a rural practice, or a practice in a health professional shortage area, or if you are not in a patient-facing role (i.e., you bill fewer than 100 patient-facing encounters during a performance period), you have fewer requirements: You need to report two medium-weighted or one high-weighted improvement activity. For others, the full credit threshold is 40 points, which can be reached by attesting to four medium-weighted activities or two high-weighted activities (or a combination to reach 40 points).
As you consider MIPS participation, it is important to note a few overarching rules related to reporting:
If you submit data as a group in one category, you must submit as a group in all categories,
If you submit as an individual, you must submit as an individual in all categories,
You must use only one method for data submission per category (e.g., you may submit quality data through claims, but not through claims and through a registry). However, you can use different methods between categories (e.g., you may submit quality data through claims and ACI measures through a registry).
AAPM track
To participate in the AAPM track and qualify for the 5 percent annual bonus payment, you must be a qualifying participant, which means practicing in a “qualifying” payment model that meets further eligibility criteria. The law is very specific about which models qualify and meet these requirements. They are the Medicare Shared Savings Program (MSSP) Tracks 2 and 3, Next Generation Accountable Care Organization, Comprehensive End-Stage Renal Disease Care (with two-sided risk), CPC+, and the Oncology Care Model (with two-sided risk). Participants within these models must become qualifying participants by having a certain percentage of payments or patients coming through the AAPM. In 2019 and 2020, the payment threshold is that 25 percent of payments made by CMS for Medicare Part B services for care of attributed beneficiaries must be paid through the AAPM. The patient threshold is that 20 percent of Medicare attributed beneficiaries must be seen through the AAPM.
Qualifying AAPM participants are excluded from MIPS and will receive a 5 percent bonus payment from 2019 through 2024. They will also receive a higher Medicare physician fee schedule update (of 0.75 percent) starting in 2026. If you participate in an alternative payment model that is not an AAPM, you are not considered a “qualifying participant” and will be subject to MIPS. However, you may receive favorable scoring in MIPS due to your participation.
Moving forward
Change can seem overwhelming, but taken in small steps it is manageable. Evaluate your practice and catalog what you are likely already doing that fulfills the requirements. The most important next step for most physicians is to “Pick Your Pace.” This will allow physicians to begin participating in the QPP at a level that works for their practice. By reporting with no possibility for penalty, you can test the system and make sure things are working as anticipated prior to 2018, when full-year reporting for cost, quality, improvement activities, and ACI will be required. Look to https://www.aafp.org/MACRAready for further resources as they become available.
