
Am Fam Physician. 1999;59(7):1843-1850
See related patient information handout on adhesive capsulitis, written by the authors of this article.
The shoulder is a very complex joint that is crucial to many activities of daily living. Decreased shoulder mobility is a serious clinical finding. A global decrease in shoulder range of motion is called adhesive capsulitis, referring to the actual adherence of the shoulder capsule to the humeral head. Adhesive capsulitis is a syndrome defined as idiopathic restriction of shoulder movement that is usually painful at onset. Secondary causes include alteration of the supporting structures of and around the shoulder, and autoimmune, endocrine or other systemic diseases. The three defined stages of this condition are the painful stage, the adhesive stage and the recovery stage. Although recovery is usually spontaneous, treatment with intra-articular corticosteroids and gentle but persistent physical therapy may provide a better outcome, resulting in little functional compromise.
The shoulder is a complex anatomic structure that allows movement in many planes. Physicians and patients alike don't often think about the importance of the shoulder joint until its function becomes compromised. It then becomes obvious how crucial it is for many essential activities. The expression “If you don't use it, you lose it” applies perfectly to diseases of the shoulder because any voluntary or involuntary guarding of the shoulder may result in loss of mobility. The term “frozen shoulder” has been loosely applied to conditions when the shoulder is working at less than its optimal range. Because the shoulder joint is so complex, it is important to determine the precise cause for loss of shoulder mobility. It is paramount that physicians use proper terminology so that they can communicate effectively and treat patients appropriately.
Definition of Terms
Many terms are used to describe limitation of shoulder movement, and all of them imply a stiff shoulder with decreased range of motion (Table 1). These terms are attempts to describe the probable underlying pathophysiologic process (i.e., bursal or capsular origins of inflammation). They were used to describe conditions that are difficult to understand and explain and, although of historic interest, they are confusing and are best discarded. The term “frozen shoulder” encompasses many of the concepts of the terms in Table 1, but it too is confusing and not always accurate. The correct term for true global decrease in shoulder range of motion is adhesive capsulitis, related to the surgical findings of actual adherence of the capsule to the humeral head.1,2
| Frozen shoulder |
| Adhesive capsulitis |
| Pericapsulitis |
| Periarthritis |
| Adherent bursitis |
| Obliterative bursitis |
Adhesive capsulitis is a syndrome defined in its purest sense as idiopathic painful restriction of shoulder movement that results in global restriction of the glenohumeral joint. It is not associated with a specific underlying condition. It has also been described as a condition of “unknown etiology characterized by gradually progressive, painful restriction of all joint motion . . . with spontaneous restoration of partial or complete motion over months to years.”3 To avoid confusion, the term “adhesive capsulitis” should be used to refer to the primary idiopathic condition and the term “secondary adhesive capsulitis” should be applied to the condition that is associated with, or results from, other pathologic states. Each case must be evaluated to determine if the restriction is idiopathic (primary) or the result of an underlying systemic illness or anatomic process (secondary). Either condition causes pain and decreased shoulder mobility.
Differential Diagnosis
Complaints of shoulder pain or movement problems are difficult to evaluate. Many shoulder conditions have similar symptoms, causes, precipitating factors and treatments. Multiple pathologic lesions may be present in a single joint.4 In assessing a patient's shoulder pain, the physician must distinguish between true glenohumeral joint problems and extra-articular derangements. Active range of motion will most likely be limited and painful in both cases, but decreased passive range of motion, which is often painful as well, most likely indicates true joint pathology.
If the patient is able to relax and the examiner can elicit full passive range of motion, the etiology of the pain is most likely to be extra-articular. Prolonged soft tissue problems, however, may eventually lead to decreased shoulder range of motion because of the patient's constant guarding of the shoulder. It is imperative to determine the precise source of shoulder pain (Figure 1) so that a program of physical therapy can be initiated to prevent compromise of shoulder movement (Figure 2). Extra-articular pain may result from strain or inflammation of muscles, tendons or bursae.
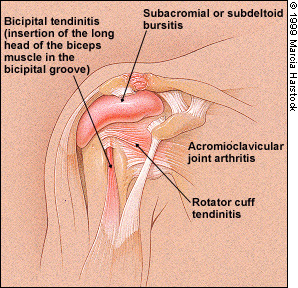
The differential diagnosis of shoulder problems is protean, but physicians should be able to readily recall some of the more common causes of shoulder pain and decreased range of motion. Bicipital tendinitis may affect active shoulder movement and is diagnosed by eliciting tenderness while pressing on the long head bicipital tendon in the bicipital groove. The bicipital tendon passes through the glenohumeral joint.
Tendinitis of the rotator cuff is the most common cause of shoulder pain and secondary decreased shoulder mobility that manifests with pain on passive and active abduction.5,6 Pain is usually greater with internal rotation of the shoulder than with external rotation. The key finding is pain in the rotator cuff on active abduction, especially at 60 to 100 degrees of abduction. Ultimately, there may be impingement and a loss of mobility. Tenderness may be elicited anteriorly over the humeral head when the arm is extended. Calcific tendinitis may also lead to impingement.
The subacromial and subdeltoid bursae are contiguous in most persons. Subacromial bursitis manifests with pain when the patient lies on his or her shoulder, or with tenderness on palpation of the space on the lateral aspect of the shoulder just inferior to the acromion along the deltoid. Subacromial bursitis may also be a reactive phenomenon in a patient with a rotator cuff injury. Acromioclavicular joint problems, commonly including osteoarthritis, may also result in decreased passive joint range of motion and local tenderness.
True shoulder pain presents with tenderness on anterior or posterior palpation. Decreased joint motion is compensated for by an increase in scapulothoracic motion during flexion and abduction. Increased scapulothoracic motion stresses other structures around the shoulder and may result in more global pain syndromes, guarding and decreased range of motion.
The evaluation of shoulder instability is important in patients with shoulder pain. Symptomatic subluxation may clinically mimic an acute rotator cuff injury or bicipital tendinitis. A high index of suspicion and a detailed physical examination combining the assessment of laxity in all directions with stress tests can help the physician determine the underlying cause of pain. Correction of any muscle imbalance is paramount to preservation of mobility and function. Muscles around the neck and shoulder girdle should be palpated for tenderness or trigger points to assess for fibromyalgia, myofascial pain syndromes and cervical osteoarthritis.
The correct diagnosis in a patient with restricted shoulder movement on physical examination and any of the previously mentioned findings, such as bursitis or tendinitis, is secondary adhesive capsulitis. The underlying condition is documented as the primary problem leading to secondary adhesive capsulitis.
Adhesive Capsulitis
FEATURES, PRESENTATION AND NATURAL HISTORY
Primary idiopathic adhesive capsulitis is difficult to define, diagnose and manage. This condition affects 2 to 3 percent of the population. It tends to occur in patients older than 40 years of age and most commonly in patients in their 50s and in women. Fifteen percent of patients develop bilateral disease. Adhesive capsulitis has been reported in children.7
The natural history of adhesive capsulitis and its clinical course is divided into three stages: the painful stage, the adhesive stage and the recovery stage (Table 2). The painful stage involves gradually increasing pain and stiffness and lasts between three and eight months. Muscle spasms in the trapezius also commonly occur during this phase. A history of a minor strain or injury before onset may be noted; however, it is unclear whether the initial strain is an independent phenomenon or an early awareness of the pain associated with the onset of adhesive capsulitis.
| Painful stage |
| Pain with movement |
| Generalized ache that is difficult to pinpoint |
| Muscle spasm |
| Increasing pain at night and at rest |
| Adhesive stage |
| Less pain |
| Increasing stiffness and restriction of movement |
| Decreasing pain at night and at rest |
| Discomfort felt at extreme ranges of movement |
| Recovery stage |
| Decreased pain |
| Marked restriction with slow, gradual increase in range of motion |
| Recovery is spontaneous but frequently incomplete |
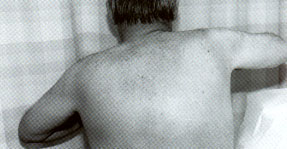
Commonly, patients note a decreased ability to reach behind the back when fastening a garment or removing a wallet from a back trouser pocket. The initial discomfort is described by many patients as a generalized shoulder ache with difficulty pinpointing the exact location of the discomfort. The pain may radiate both proximally and distally, is aggravated by movement and alleviated with rest. Sleep may be interrupted if the patient rolls on the involved shoulder.
This condition progresses to one of severe pain accompanied by stiffness and decreased range of motion. The stiffening increases to the point where the natural arm swing that accompanies normal gait is lost.8 The patient tries to compensate for this loss by using other muscles and increasing scapular rotation to accomplish various activities. This places additional strain on the other muscle groups, leaving them overworked and tender.
The physical examination during the painful stage of adhesive capsulitis may reveal muscle spasm and diffuse tenderness about the glenohumeral joint and the deltoid muscle. An area of pinpoint tenderness is seldom found. With disease progression and in longstanding cases, disuse atrophy of the shoulder girdle may result. Passive and active range of motion in all planes of shoulder movement are lost (Figure 5). This global loss of motion is the primary factor distinguishing adhesive capsulitis from many of the conditions associated with secondary adhesive capsulitis.

The second stage, the adhesive stage, involves increasing stiffness with diminishing pain. Pain decreases at night, and discomfort occurs only at the extremes of motion, although movement is dramatically decreased. This stage lasts four to six months.
The final stage, called the recovery stage, lasts from one to three months and is characterized by minimal pain but severe restriction of movement. This latter stage is self-limiting, with a gradual and spontaneous increase in range of motion. Complete recovery, however, is infrequent. The external rotation range of motion improves first, followed by abduction and internal rotation. Short recovery periods may have associated bouts of pain before each phase of improvement. Although approximately 7 to 15 percent of patients permanently lose their full range of motion, only a few have a true functional disability.9,10
PATHOLOGY
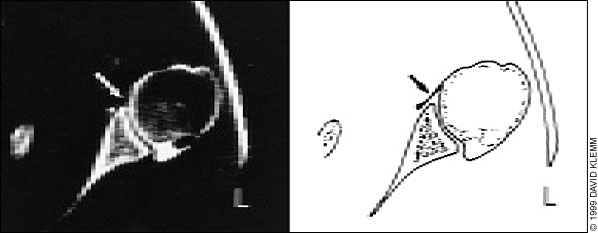
The pathophysiology of primary and secondary adhesive capsulitis remains elusive. It is believed that in patients with diabetes, associated microvascular disease causes abnormal collagen repair, which predisposes them to adhesive capsulitis. Occasionally, fibrous strands are seen traversing the joint space (Figure 6). Patients with diabetes often present with fibrosis elsewhere (i.e., Dupuytren's contracture). Trauma, the associated transient inflammatory state with granulation tissue, and eventual fibrous adhesions and thickening of the capsule may cause adhesive capsulitis.1,8
Immobilization is an intriguing possible etiologic factor for adhesive capulitis in patients with stroke or postmyocardial infarction; however, prolonged casting studies have not supported this theory.8 Neuropathic mechanisms, including suprascapular nerve compression, have been considered, but none accounts for most cases of adhesive capsulitis. Although strong evidence suggests an association among these neuropathic and vascular conditions and adhesive capsulitis, no pathophysiologic mechanisms are convincing.
Theories regarding autoimmune reaction to tendon degeneration have led to immunologic investigations. Although random and inconsistent, the inflammatory indexes measured (e.g., erythrocyte sedimentation rate) were partially supported because they were slightly elevated and improved as the disease improved.11 Synovial fluid offers no clues to the etiology of adhesive capsulitis. Biopsies of the synovial lining have revealed increased fibroblasts and vascular dilatation, but few or no perivascular inflammatory cells.
EVALUATION
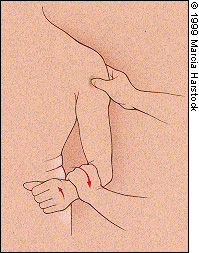
The diagnosis of adhesive capsulitis is primarily clinical. In general, the scapular rotation occurs at 60 degrees with active abduction of the shoulder. In an unaffected person, the shoulder can be passively abducted to 90 degrees even when the physician holds the scapula. Inability to achieve the 90-degree arc with scapular stabilization is the clue to the diagnosis in both primary and secondary adhesive capsulitis. It is important to assure that the scapula is secured when assessing passive range of motion (Figure 7).

Radiographs are important in assessing restricted range of motion in the diagnosis of secondary adhesive capsulitis. Osteoarthritis, fracture, avascular necrosis, crystalline arthropathy, calcific tendinitis and neoplasm may be detected on plain radiographs. Radiographs of patients with early adhesive capsulitis are normal. Later changes sometimes show osteopenia, cyst-like changes in the humeral head and joint-space narrowing. A chest radiograph may be useful in establishing the diagnosis of tuberculosis or malignancy-associated adhesive capsulitis.
Arthrography, although invasive, is useful to document decreased joint volume. The unaffected shoulder will accommodate 20 to 30 mL of contrast material, whereas the shoulder with adhesive capsulitis will only be able to hold 5 to 10 mL. Arthrograms may reveal an irregularity of the capsular insertion at the anatomic humeral neck and a decreased axillary fold. From 10 to 30 percent of patients are found to have a demonstrable rotator cuff tear at arthrography, yet a significant number also have normal findings. Arthrography should be reserved for use in patients whose diagnosis remains uncertain following physical examination and radiography.
Arthroscopy may have a limited role in the diagnosis of other diseases that mimic adhesive capsulitis, but it does not aid in the diagnosis of adhesive capsulitis itself and is not used frequently.12 The usefulness of magnetic resonance imaging (MRI) in the diagnosis of adhesive capsulitis has also been evaluated.13 Studies revealed that some changes seen on MRI are specific and sensitive for adhesive capsulitis; however, the decrease in joint fluid is not appreciated. MRI may become a useful, noninvasive way to document capsular thickening, but further studies are needed. In most cases, the diagnosis of adhesive capsulitis is clinical; however, if any imaging is necessary, arthrography remains the procedure of choice. If there are no underlying illnesses, laboratory investigations will be unremarkable.
Other Causes of Secondary Adhesive Capsulitis
Some systemic diseases are known to be associated with adhesive capsulitis (Table 3) and should be considered in patients with restricted shoulder movement. Trauma, avascular necrosis and osteoarthritis may predispose a patient to secondary adhesive capsulitis. Systemic diseases such as diabetes, hyperthyroidism and rheumatoid arthritis are also associated with secondary adhesive capsulitis and must be considered in a patient with limited range of motion of the shoulder.14,15 Patients often have referred shoulder pain from the heart, neck, diaphragm, liver or spleen. It is unclear why patients with a history of myocardial infarctions, cerebrovascular accidents and chronic pulmonary diseases, such as tuberculosis and pulmonary cancer, are also predisposed to adhesive capsulitis. Patients with reflex sympathetic dystrophy (related to some of these events) may have restricted range of motion of the shoulder that becomes permanent in the later stages of disease. Some patients may also develop reflex sympathetic dystrophy as a result of primary or secondary adhesive capsulitis.
| Diabetes mellitus |
| Thyroid illness |
| Trauma |
| Rheumatoid arthritis |
| Lung cancer |
| Pulmonary tuberculosis |
| Chronic lung disease |
| Myocardial infarction |
| Cerebrovascular accidents/hemiplegia |
| Scleroderma |
| Postmastectomy |
| Cervical radiculitis |
Management
Although studies comparing various treatment modalities for adhesive capsulitis reveal that no specific treatment method has any long-term advantage, early and accurate diagnosis is imperative.16 In patients with adhesive capsulitis, the goal of treatment is pain reduction and preservation of shoulder mobility. The first step is preventing secondary adhesive capsulitis by definitively addressing underlying causes. Avoiding prolonged immobilization in patients who may be predisposed to adhesive capsulitis is crucial.
Treatment of a shoulder injury of any etiology requires early range of motion therapy to reduce muscle spasm while maintaining full range of motion. Heat, cold and other modalities that relax the muscles may help preserve range of motion. Adequate analgesia is necessary for successful treatment in this phase. Vigorous and forceful exercises are contraindicated because of the pain associated with the rupture of adhesions. Also, the more painful treatment regimens have been found to be associated with a higher level of non-compliance. Constant encouragement is necessary for patients with adhesive capsulitis, since resolution may be slow. Gradually increasing the range of motion of the shoulder will decrease the pain associated with the disease. Physical therapy done at home, including Codman exercises, “climbing the wall” or placing things up higher to encourage reaching, is cost effective but requires a long rehabilitative process.17
Nonsteroidal anti-inflammatory drugs (NSAIDs) help to relieve pain and inflammation. Analgesics are indicated when NSAIDs are contraindicated. Muscle relaxants are helpful in the early stages of the disease when spasm is predominant. Low-dose antidepressant medications (e.g., 10 mg of amitriptyline [Elavil] taken at night) may help to avoid a cycle of sleep disturbance leading to a chronic pain syndrome and fibromyalgia.8
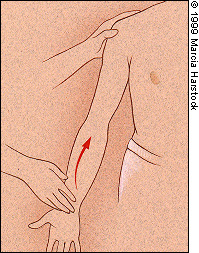
Intra-articular corticosteroid injections are used in affected patients to relieve pain and permit a more vigorous physical therapy routine. The injection site is located 1 cm distal and 1 cm lateral to the coracoid process18 (Figure 8). Full external rotation of the humerus with the elbow held in a relaxed position at the patient's side helps open up the space, which is difficult to enter if contracted by adhesive capsulitis.19 The usual dosage is 15 to 40 mg of triamcinolone acetonide (Kenalog) or another depot steroid with 1 mL of 1 percent lidocaine. Although intra-articular corticosteroids are frequently used, no long-term benefits from this therapy (i.e., shorter time to full recovery) have been proved. Some clinicians advocate simultaneous intra-articular and bursal injections for pain relief before beginning physical therapy. Oral corticosteroids are not helpful.

Severe adhesive capsulitis diagnosed in the later stages is more difficult to manage. The above treatments, useful on occasion, are not always successful. Surgical intervention should be considered when physical therapy and injections fail (no improvement after three months of therapy). Manipulation under anesthesia to break up the adhesions is reserved for use in the adhesive stage. During this procedure, the joint capsule and sub-scapular muscles are ruptured, and aggressive rehabilitation is employed to restore and maintain range of motion of the shoulder. Patients undergoing manipulation may receive an intra-articular corticosteroid injection after the procedure and begin physical therapy the day of the procedure. Icing is often helpful.
Another option is the administration of an interscalene block before the manipulation; this renders the patient pain free and allows for the immediate start of physical therapy. Risks associated with manipulation under anesthesia include humeral fracture, dislocation and rotator cuff rupture. Contraindications to manipulation include severe osteopenia, a history of fracture or dislocation, or recurrence following adequate manipulation.12 For patients with loss of motion refractory to closed manipulation, arthroscopic capsular release has been shown to improve motion with minimal operative morbidity.20 In this study, most patients had a marked decrease in pain, and functional improvement. Some investigators21 demonstrated that arthroscopic release was helpful in patients with diabetes-associated adhesive capsulitis who were refractory to conservative measures. Thirteen of the patients studied had no pain, full range of motion and full function after surgical release.
Interestingly, a marked discrepancy exists between the patient's subjective awareness of residual range deficit and the measurable (objective) restrictions. Many patients with range deficits regard their recovery as complete. This difference in subjective and objective assessment of recovery, plus the variation and confusion in the definitions of adhesive capsulitis, may account for the conflicting reports of prognosis and therapy.12