
Am Fam Physician. 2021;103(3):186-188
Author disclosure: No relevant financial affiliations.
Key Points for Practice
• Chronic pelvic pain is most often associated with endometriosis, bladder pain syndrome, or both but also shares the multifactorial aspects of other chronic pain syndromes.
• Neuromuscular pain conditions are common in chronic pelvic pain and can be diagnosed with palpation for pelvic floor muscle tenderness and with the FABER and Carnett tests for sources outside the pelvic floor.
• Pelvic floor physical therapy and trigger point injections can both improve vaginal pain and dyspareunia from neuromuscular chronic pelvic pain.
• Surgical interventions appear to offer no benefit in chronic pelvic pain.
From the AFP Editors
Chronic pelvic pain is associated with cognitive, behavioral, sexual, and emotional consequences. It is most often defined as noncyclic pain that lasts more than six months, and up to 26% of women meet these criteria. The American College of Obstetricians and Gynecologists (ACOG) has new recommendations for managing this condition.
Common Associated Conditions
The most common associated conditions are endometriosis and bladder pain syndrome, which affect between 60% and 70% of patients with chronic pelvic pain. Nearly one-half of patients with chronic pelvic pain have both conditions. Other common conditions that affect at least one in five patients with chronic pelvic pain are irritable bowel syndrome, interstitial cystitis, pelvic floor muscle tenderness, and depression.
Evaluation
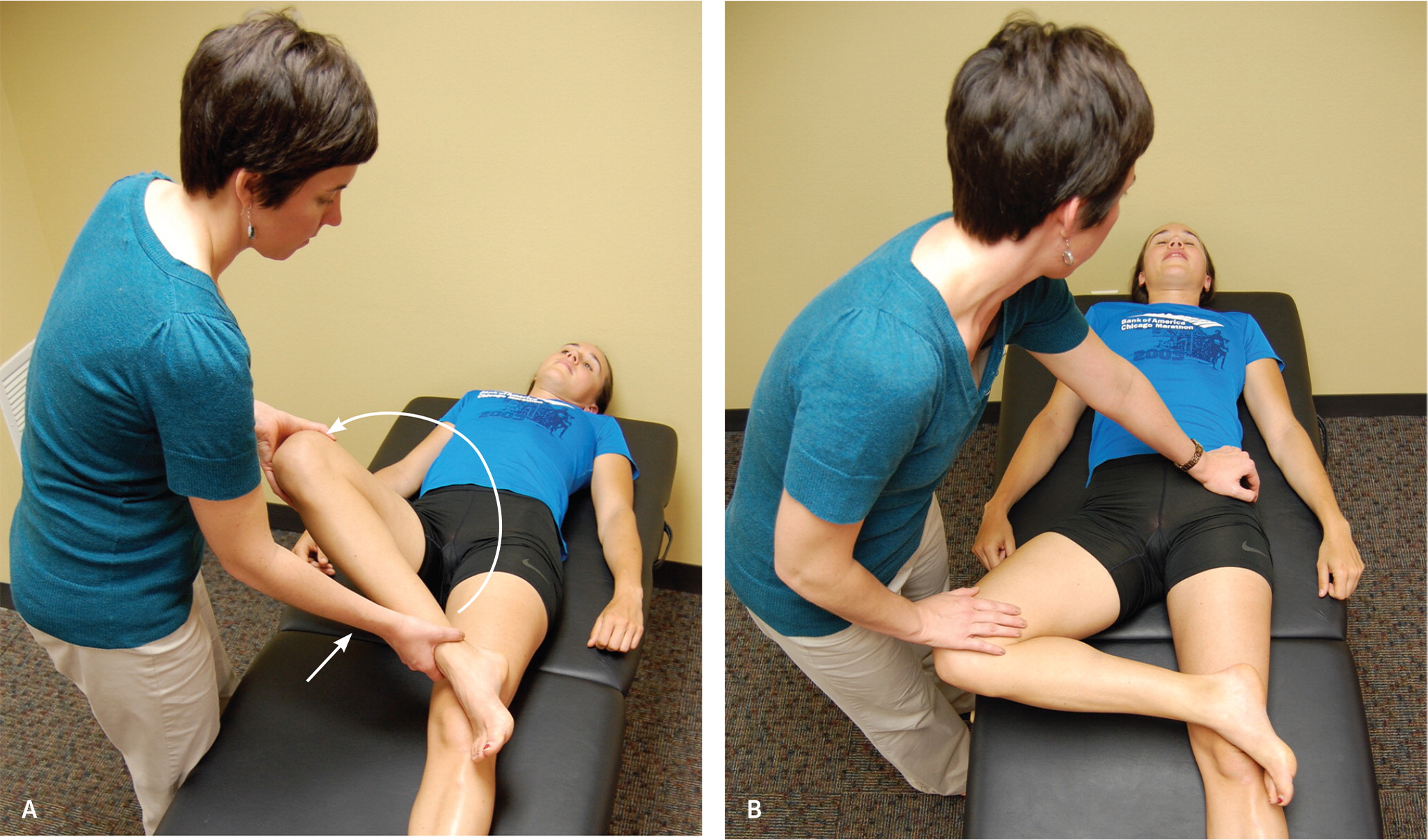
Because chronic pelvic pain is often multifactorial, most patients will have multiple pain generators and comorbid conditions. Although many conditions are associated with chronic pelvic pain, determining how pain changes with sexual activity, menstruation, urination, and defecation is a good starting point. Patients often focus on visceral etiologies, yet neuromuscular issues such as myofascial trigger points may be more common and are often overlooked. Single-digit or swab palpation for tenderness of pelvic floor muscles, or palpation of the abdomen and the lower back, including the sacroiliac joints, that reproduces pain can identify possible neuromuscular conditions. In one small study, pelvic floor muscle tenderness or a positive flexion, abduction, and external rotation (FABER; Figure 1) test identified 85% of patients with chronic neuromuscular pelvic pain. A positive Carnett test, where abdominal tenderness increases with abdominal wall muscle contraction, also demonstrates neuromuscular pain. The Carnett test is described in a previous issue of American Family Physician (https://www.aafp.org/afp/2016/0301/p380.html).
In addition to neuromuscular and gynecologic conditions, many patients with chronic pelvic pain also have comorbid mood disorders, gastrointestinal conditions such as irritable bowel syndrome or diverticulitis, and urinary conditions such as interstitial cystitis. Laboratory and imaging tests for chronic pelvic pain are useful only if suggested by the presentation.
Multidisciplinary Care
Multidisciplinary care is essential for chronic pelvic pain because the central nervous system sensitization of the chronic pain process makes it unlikely that pain will resolve through a single intervention. In addition to treating identified physical pain generators, treating psychological comorbidities is an essential element of care.
Consider pelvic floor physical therapy, cognitive behavior therapy, or sex therapy, alone or in combination. Pelvic floor muscle tenderness is common in patients with chronic pelvic pain. In one randomized trial, pelvic floor physical therapy with trigger point injections markedly improved vaginal pain and dyspareunia. For those who do not improve with pelvic floor physical therapy, a focused evaluation for musculoskeletal disorders should be considered.
Chronic pain syndromes predispose patients to mood disorders and social isolation. Cognitive behavior therapy has a small to moderate benefit in patients with chronic pain syndromes. Sex therapy has been shown to improve symptoms of female orgasmic disorder and genito-pelvic pain, allowing couples to achieve pain-free intercourse.
Surgical interventions, including laparoscopic uterosacral nerve ablation and presacral neurectomy, do not appear to improve chronic pelvic pain. Laparoscopic adhesiolysis offers no benefit and leads to poorer patient outcomes, including increased pain and bowel injury.
Pain management specialists can be a part of multidisciplinary care for interventional procedures or pharmacotherapy.
Medications
Evidence of medication effectiveness in chronic pelvic pain is lacking, so recommendations are based on evidence for other neuropathic pain syndromes. Serotonin-norepinephrine reuptake inhibitors (SNRIs) and gabapentin (Neurontin) or pregabalin (Lyrica) are recommended if underlying visceral etiologies have been addressed and a neuropathic pain component has been identified. These medications show benefit in small retrospective studies that are not specific to pelvic pain. SNRIs also treat depressive symptoms and improve quality of life with neuropathic pain.
Opioids are not recommended in chronic pelvic pain because they neglect the underlying etiology while increasing risks of adverse effects, tolerance, overdose, and dependence.
Nonpharmacologic Interventions
In myofascial chronic pelvic pain, trigger point injections of saline, anesthetic, steroids, or opioids can improve pain and function. Injections often provide immediate relief of cutaneous nerve entrapment or trigger points, although repeated procedures may be required. Needle insertion itself may be effective without injection. Botulinum toxin injection benefit is unclear and should be reserved for treatment of myofascial pelvic pain that does not respond to physical therapy.
Acupuncture can be used for chronic pelvic pain caused by a musculoskeletal etiology. It reduces pain and opioid use in chronic musculoskeletal pain. Yoga is recommended based on a noncontrolled trial in chronic pelvic pain that showed improvements in pain, emotional well-being, and sexual function at six weeks. Relaxation, tai chi, massage, and manipulation have weaker evidence of benefit.
The views expressed are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of the Air Force, Uniformed Services University of the Health Sciences, Department of Defense, or the U.S. government.
Guideline source: American College of Obstetricians and Gynecologists
Evidence rating system used? Yes
Systematic literature search described? Yes
Guideline developed by participants without relevant financial ties to industry? Not reported
Recommendations based on patient-oriented outcomes? Yes
Published source: Obstet Gynecol. March 2020;135(3):e98–e109
Editor's Note: Chronic pelvic pain is a common and difficult to treat multifactorial syndrome. ACOG has updated its previous practice bulletin covering chronic pelvic pain to highlight the neuromusculoskeletal and psychosocial factors that contribute to chronic pain syndromes. Although many of the recommendations are similar to a previous American Family Physician article (https://www.aafp.org/afp/2016/0301/p380.html), the new guideline emphasizes multidisciplinary care, including physical therapy, behavioral health, and pain management, while arguing against surgical therapy. A recent large randomized controlled trial of gabapentin in chronic pelvic pain would have likely taken away this recommendation if it had been available.1 Despite a four-week titration of gabapentin or placebo to maximal tolerated dosages before the study, there was no improvement in average or worse pain levels after 16 weeks with gabapentin.—Michael J. Arnold, MD, Contributing Editor
1. Horne AW, Vincent K, Hewitt CA, et al.; GaPP2 collaborative. Gabapentin for chronic pelvic pain in women (GaPP2): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2020;396(10255):909–917
