Decoding G2211: Myths Versus Facts
Primary care visits are thoughtful, complex, and all about ensuring patients’ health care needs are met. Here's the catch, though: All that work physicians do isn’t appropriately paid for.
One physician billing code is specifically designed to pay more accurately for the complex, high-value visits that primary care physicians provide as part of a continuous relationship with a patient. The equation is simple. Better payment equals better patient access and better outcomes. G2211 can make this a reality.
Unfortunately, this important policy advance, poised to improve health care nationwide, has attracted opposition. But the misperceptions driving criticism of G2211 do not stand up to scrutiny.
What is G2211?
Code G2211 describes “visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious condition or a complex condition.” In short, G2211 is for evaluation and management (E/M) visits that are part of an ongoing, longitudinal care relationship. It is an add-on code that can be listed separately in addition to office/outpatient E/M visits for new or established patients (i.e. codes 99202-99215).
The AAFP's Meredith Yinger (senior manager, federal policy) explains G2211 and how it affects family physicians.
The AAFP's Natalie Williams (senior manager, legislative affairs) explains why the Academy is advocating for G2211.
The AAFP's Dave Tully (vice president, government relations) shares how family physicians can advocate for G2211.
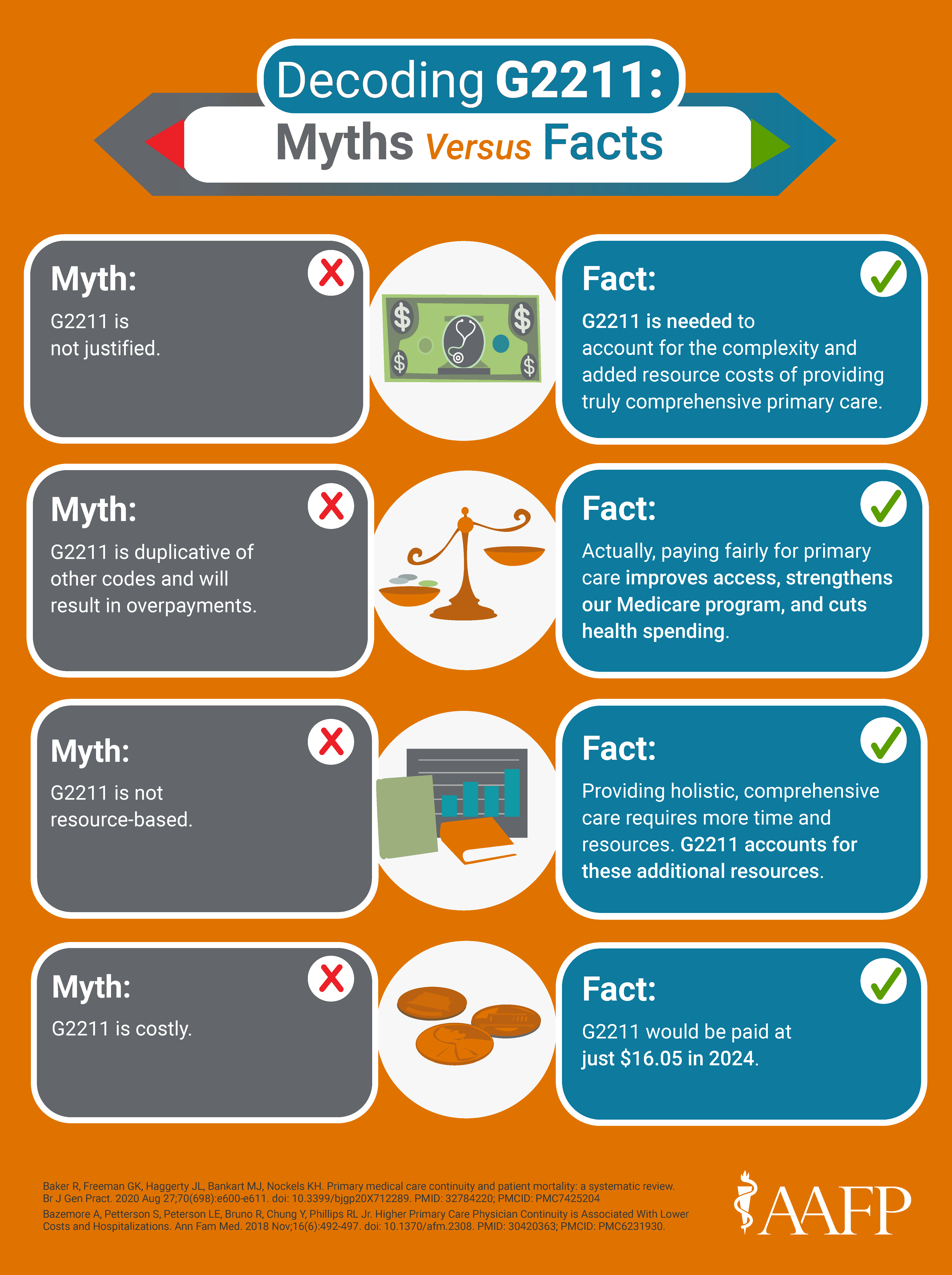
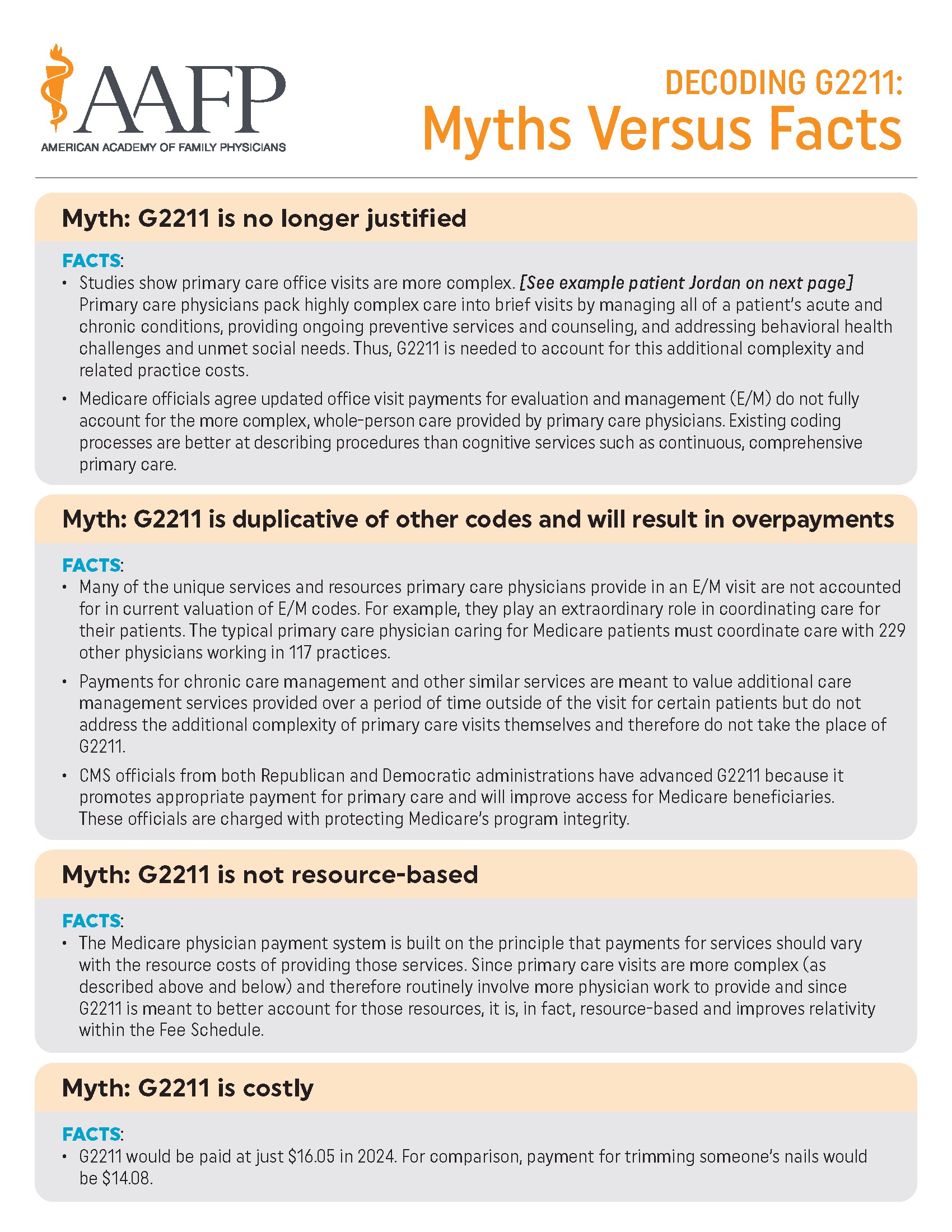
Myths Versus Facts
❌ Myth: G2211 is not justified.
✔️ Fact: G2211 is needed to account for primary care's complexities and related practice costs.
Studies show that primary care office visits are more complex than those conducted by other specialties. Primary care physicians pack highly complex care into brief visits by managing all of a patient’s acute and chronic conditions, providing ongoing preventive services and counseling, and addressing behavioral health challenges and unmet social needs. To fully account for this additional complexity and related practice costs, G2211 is needed.
Medicare officials agree that updated office visit payments for evaluation and management (E/M) do not fully account for the more complex, whole-person care provided by primary care physicians. Existing coding processes are better at denoting procedures than at describing cognitive services such as continuous, comprehensive primary care.
❌ Myth: G2211 is not resource-based.
✔️ Fact: G2211 is resource-based and improves relativity within the Medicare physician fee schedule.
The Medicare physician payment system is built on the principle that payments for services should vary with the resource costs of providing those services.
Because primary care visits are more complex (as described above and below) and therefore routinely involve more physician work to provide, G2211 is meant to better account for those resources.
❌ Myth: G2211 is costly.
✔️ Fact: G2211 would be paid at just $16.04 in 2024.
For comparison, payment for trimming someone's nails would be $14.08.
❌ Myth: G2211 is duplicative of other codes and will result in overpayments.
✔️ Fact: CMS officials from both Republican and Democratic administrations are charged with protecting Medicare’s program integrity.
Current E/M coding fails to account for many of the unique services and resources that primary care physicians provide or reflect their extraordinary role in coordinating care for their patients. The typical primary care physician caring for Medicare patients must coordinate care with 229 other physicians working in 117 practices.
Payments for chronic care management and similar services are meant to value additional care management provided over time and beyond the exam room. However, they do not by themselves address the additional complexity of primary care visits and therefore cannot take the place of G2211.
Example patient, Jordan
A 75-year-old established male patient with a history of hypertension, diabetes, and coronary artery disease complains of increased urinary frequency and a change in urinary stream.
NOTE: The lists in this example are not meant to suggest that these services are not paid for via E/M or other codes, but rather illustrate the inherent complexity of visits that are part of longitudinal care.
A one-time visit with a specialist includes:
an order for prostate-specific antigen (PSA) test,
a prescription for Flomax (for which the side effects would be reviewed),
evaluation of sleep habits,
a rectal exam,
review of options for treatment with patient to include shared decision-making discussion about starting medications,
counsel on limiting fluids before sleep and other factors that could contribute to poor sleep and nocturia, and
a request to return as needed.
A visit with a primary care physician includes:
a review of the patient’s hemoglobin A1c to ensure his diabetes was not contributing to urinary frequency;
a review of blood pressure history;
a review of current medications (to rule out the patient’s diuretic is causing urinary frequency);
a check to the patient’s last PSA before ordering a new one;
a prescription of Flomax after a discussion with the patient on possible side effects as related to the patient’s current medication list;
counseling on limiting fluids before sleep and other factors that could contribute to poor sleep and nocturia;
checking on symptoms and management of other chronic conditions;
determining if the patient is up to date on all recommended preventive vaccinations and providing or refering the patient to receive any outstanding vaccines;
a screening for unmet social needs and other determinants of health;
a mental health and substance use screening, counseling, brief intervention and referral as needed;
nutrition, exercise, and behavioral health counseling as needed; and
updating and coordinating with the rest of the care team, including specialists and family caregivers.
What is the AAFP doing to support the G2211 add-on code?
The AAFP strongly supported the creation of G2211 and urged CMS to ensure its full implementation in 2024. Learn about recent advocacy and keep track of our activity.