Am Fam Physician. 1998;57(5):995-1002
This is Part I of a two-part article on pitfalls in the radiologic evaluation of extremity trauma. Part II, “The Lower Extremity,” will appear in the next issue.
Family physicians often are required to evaluate patients who present with acute skeletal trauma. The first of this two-part series discusses the features and evaluation of some commonly missed fractures and dislocations of the upper limb, excluding the hand. Dislocations of the sternoclavicular joint are infrequent and often missed. Clavicular fractures in adults usually are not hard to diagnose. Acromioclavicular joint dislocations represent about 10 percent of all dislocation injuries to the shoulder girdle. Forty percent of all dislocations occur at the glenohumeral joint. Scapular fractures are often a result of significant force. Multiple views should be obtained in adults with a suspected fracture of the elbow. Complications in fractures of the wrist are strongly related to the location of the fracture.
Regardless of the experience of the treating physician, accurate detection and evaluation of musculoskeletal trauma is a challenge. This two-part series, divided into separate discussions of the upper limb and the lower limb, reviews key diagnostic features of some commonly missed fractures and dislocations. The mechanism of injury, appearance of radiographic projections, plain film signs and advanced imaging techniques that are useful for further evaluation are discussed.
Plain radiographs remain pivotal in the initial assessment of patients with a suspected fracture or dislocation. The radiographic approach should be tailored to the patient's history and physical examination. The possibility that an unusual or unexpected finding may represent a normal physical variant should always be considered.1 Routine use of comparison films of the contralateral, asymptomatic side is not appropriate, although this technique may be useful in the evaluation of skeletally immature patients with a suspected physeal injury or when a normal variant is being considered.
Sternoclavicular Joint
Dislocations of the sternoclavicular joint are infrequent, occurring most often in patients under 25 years of age. These dislocations often are associated with other significant injuries and are difficult to visualize and, consequently, are often missed. This injury commonly constitutes an epiphyseal separation with a fracture through the unfused physis of the proximal clavicle, rather than a true dislocation.
Direct trauma to the shoulder transmits forces through the clavicle to the sternoclavicular joint. Anterior dislocations occur more commonly, but the posterior (retrosternal) type of dislocation is most important to recognize because of its potential for concomitant injuries to the structures of the superior mediastinum, including the great vessels, esophagus, trachea and nerves.
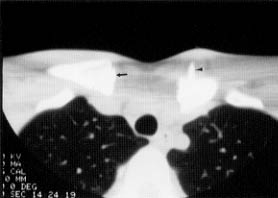
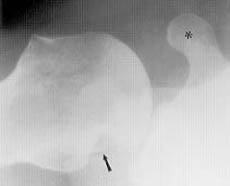
Although conventional anteroposterior radiographs may demonstrate elevation of the medial end of the clavicle in anterior dislocations and depression below that of the normal side with posterior dislocations, computed tomographic (CT) scanning is now considered the imaging modality of choice. Both the joint and mediastinum may be evaluated by CT scanning (Figure 1).
Clavicle
Clavicular fracture is one of the most frequent childhood fractures. This injury may be a greenstick, plastic bowing or nondisplaced complete fracture. Nondisplaced complete fractures may be missed unless an image is obtained with 15 degrees of cephalic angulation.
Fracture of the clavicle in a skeletally mature patient does not typically present a diagnostic dilemma. This fracture occurs most commonly following a fall onto an outstretched hand. Eighty percent of these injuries involve the middle one third of the clavicle. The fractures are usually transverse and complete, although some may be comminuted, with overriding of fragments. Fifteen percent of all clavicular fractures involve the outer one third of the clavicle. These fractures may be associated with coracoclavicular ligament disruption.
Acromioclavicular Joint
Acromioclavicular joint dislocations usually result from a fall on an outstretched arm in patients who are 15 to 40 years of age. These injuries represent approximately 10 percent of all dislocations involving the shoulder girdle. Although initial radiographs may be normal, further imaging should be performed when clinical suspicion is high. A single radiographic view that includes both joints permits the assessment of symmetry. Stress views taken with weights suspended from each wrist will provide the diagnosis. The normal acromioclavicular joint space of 3 to 8 mm varies no more than 2 to 3 mm between the two joints in an individual. In uninjured patients, the inferior cortical margins of the acromion and clavicle are smoothly contiguous, and the coracoclavicular distance measures 11 to 13 mm. A difference of more than 3 to 4 mm between the two sides is abnormal.
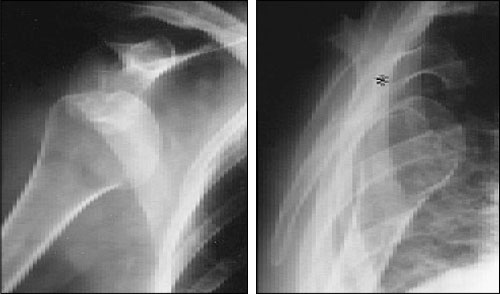
Three types of acromioclavicular ligamentous disruption occur. Type I is a clinical diagnosis. Despite normal radiographs, the acromioclavicular ligaments are stretched or torn. Type II manifests as widening of the acromioclavicular joint (Figure 2) and/or minor elevation or posterior subluxation of the distal portion of the clavicle. These findings indicate isolated disruption of the acromioclavicular ligament. Type III represents disruption of both the acromioclavicular and the coracoclavicular ligaments, with dislocation of the acromioclavicular joint and elevation of the distal clavicle.
Glenohumeral Joint
The bony anatomy of the glenohumeral joint allows a wide range of motion at the expense of stability. The glenohumeral joint is the most frequently dislocated major joint, accounting for 40 percent of all dislocations.
Glenohumeral dislocations are classified as anterior (95 percent), posterior (4 percent) and, rarely, inferior or superior.
Anterior dislocations and the commonly associated posterolateral humeral head compression fracture (Hill-Sachs deformity) occasionally present a diagnostic problem (Figures 3 and 4). The less frequently associated fracture of the anterior glenoid (Bankart lesion) is not easily recognized (Figure 5). CT scanning or magnetic resonance imaging (MRI) may be necessary to demonstrate the purely cartilaginous lesion of the labrum, as originally described by Bankart, and to further evaluate the bony glenoid rim, which may also be involved (Figure 6).


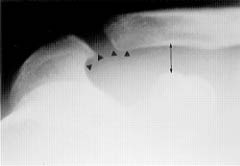
Unlike an anterior dislocation of the gleno-humeral joint, the rare posterior dislocation goes unrecognized on initial evaluation in over 50 percent of cases (Figure 7). The injury typically is associated with violent muscular contractions, such as those that occur during generalized motor seizures, electrocution and electroconvulsive therapy, and its infrequency and subtle plain film findings contribute to this abnormality being overlooked.

Radiographically, the “light-bulb” sign (where the humeral head appears circular) is seen as the humeral head is held fixed in internal rotation. Other features include the “vacant” glenoid cavity (the radiographic appearance is due to an increase in the gleno-humeral distance), loss of the normal parallelism of the articular surfaces, and the “trough line” (a line parallel and lateral to the subchondral articular surface of the humeral head, representing an impaction fracture of the head as a consequence of direct compression by the posterior glenoid rim during dislocation). Associated injuries include posterior glenoid rim fractures, lesser tuberosity avulsions and subscapularis tendon detachment.
Scapula
Scapular fractures constitute only 5 to 7 percent of all shoulder-girdle fractures. These injuries often are a result of significant force. The association between scapular fractures and other severe and potentially life-threatening injuries is high. Most involve the scapular body.
Fractures of the acromion usually follow a direct blow. These fractures require differentiation from the normal variant, the os acromiale (Figure 8). The coracoid process is usually fractured by either a direct injury from the dislocating humeral head, a direct force on the tip of the coracoid itself or an avulsion that is due to traction on the coracoclavicular ligament associated with acromioclavicular joint dislocation. Isolated fractures of the coracoid tend to occur in athletes as a result of an avulsion injury and in trapshooters as a result of repetitive stress from the impact of the recoiling rifle. These fractures are best visualized on an axillary view.

Elbow
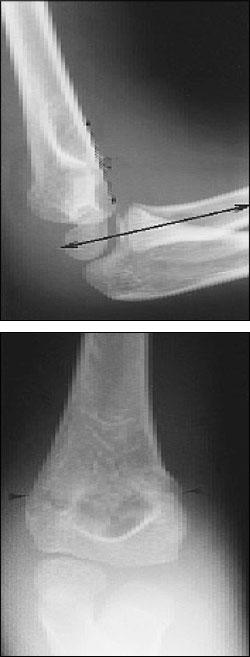
The anterior humeral line is drawn along the anterior aspect of the humeral shaft on the lateral radiograph (Figure 9). This line passes through the middle one third of the capitellum in bones that are not injured. Only true lateral views should be used to assess this line. A supracondylar fracture changes the anterior humeral line as it passes through the anterior one third or entirely anterior to the capitellum (Figure 10).
The radiocapitellar line (Figure 10, top) is obtained by bisecting the proximal radial shaft and extending the line proximally. In uninjured patients, this line passes through the capitellum on every view. If it does not, dislocation of the radial head or displacement of the capitellum should be suspected.
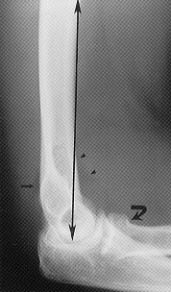
The fat pads also must be evaluated. On lateral radiographs, the normal anterior fat pad lies against the anterior surface of the distal humerus. A joint effusion displaces this fat pad anteriorly and produces the “sail sign.” The posterior fat pad is not visible in radiographs of the normal elbow. In patients who have undergone trauma, demonstration of the posterior fat pad mandates a thorough search for a fracture (Figure 9). The fat pads, however, may be elevated if fluid that is due to other conditions, such as joint infection or inflammation, is present.
A high index of suspicion should be maintained, and multiple views of the elbow should be obtained in adult patients with an apparently isolated proximal fracture of the ulna or an isolated radial head dislocation, since these are uncommon injuries. However, the Monteggia fracture, a combination of these two injuries, is relatively common (Figure 11). Similarly, although isolated dislocations of the distal radioulnar joint are infrequent, Galeazzi fractures occur more commonly. A fracture of the radius, which usually occurs at the junction of the middle and the distal one third and often with ulnar displacement of the distal fragment, is associated with ulnar dislocation (Figure 12).

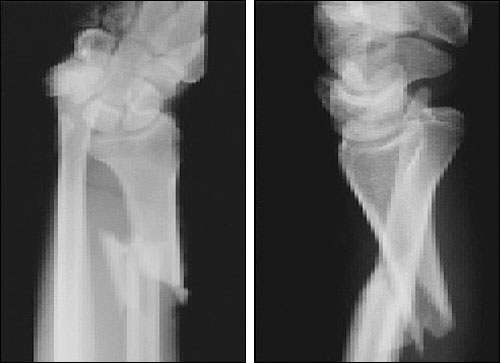
Torus and plastic bowing fractures are unique to children and often are subtle on plain films. Torus fractures are typically seen as cortical buckling, usually involving the metaphysis of long bones. Plastic bowing fractures manifest as a gentle curving of the involved shaft of the long bones (Figure 13).

Wrist
The most common fracture in the wrist involves the scaphoid (also known as the navicular bone). Although common, this fracture is easily missed. A patient with anatomic snuff-box tenderness requires thorough radiographic assessment. The assessment should include a lateral radiographic view and antero-posterior views of the wrist in radial and ulnar deviation and with 20-degree beam angulation toward the elbow. This fracture, however, may not be apparent on initial images, and a normal radiograph does not exclude the diagnosis. Repeated examination in 10 to 14 days is advised and during this time, the wrist should be placed in a thumb spica cast.
Although bone scans are highly sensitive,2–4 MRI may supersede scintigraphy in the future because of its far greater spatial and contrast resolution, high sensitivity and specificity, and ability to delineate adjacent soft tissues and bones. The role of MRI in the evaluation of scaphoid fracture, however, is still being evaluated.
Complications are largely determined by the location of the fracture. Five percent of scaphoid fractures result in nonunion, and many patients ultimately develop osteoarthritis and avascular necrosis. Displaced scaphoid fractures are more likely to show nonunion and malunion. Fractures occurring in the proximal one half of the scaphoid predispose the proximal pole to avascular necrosis. CT scanning is useful to evaluate these processes.
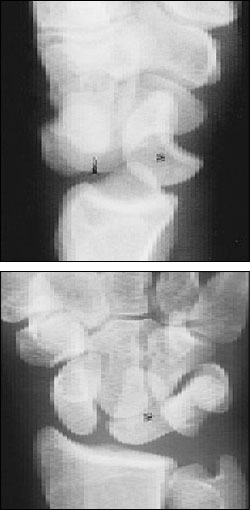
Scapholunate dissociation, perilunate dislocation and lunate dislocation represent a continuum of injury with increasing hyperextension associated with a fall on an outstretched hand. Scapholunate dissociation, the most common form of wrist instability, is suggested by the Terry Thomas, or David Letterman, sign, in which the scapholunate distance is wider than 2 mm (Figure 14). Disruption of the scapholunate ligament is indicated by palmar tilting of the scaphoid, which appears foreshortened.
The protection imparted by the radial articular surface causes perilunate dislocations to occur three times more often than lunate dislocations. Radiographs demonstrate normal radiolunate alignment with dorsal dislocation of the other carpal bones. Commonly associated with a scaphoid fracture, the injury is then called a trans-scaphoid perilunate fracture–dislocation (Figure 15).

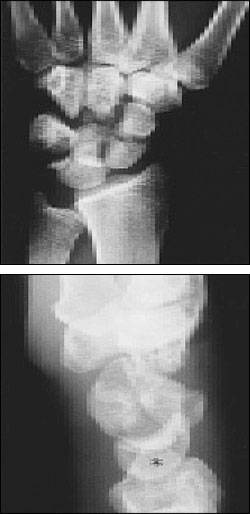
Lunate dislocation occurs least commonly. The carpus typically dislocates volarly and remains in the normal position, so that the capitate appears to be aligned with the distal portion of the radius (Figure 16).