
This is a corrected version of the article that appeared in print.
Am Fam Physician. 1999;59(2):313-324
See related patient information handout on flexible sigmoidoscopy, written by the authors of this article.
Flexible sigmoidoscopy is an important screening procedure because of its ability to detect early changes in the distal colon. The 60-cm flexible sigmoidoscope provides excellent visualization with minimal discomfort to patients. Successful sigmoidoscopy requires adequate patient preparation, proper equipment and an experienced examiner who can recognize both normal and abnormal findings. Complications arising from sigmoidoscopy are rare, but patients may experience some cramping, gas or watery stools. Screening and primary preventive measures, including regular exercise and increased dietary fiber intake, can lower the morbidity and mortality associated with colorectal cancer.
Colorectal malignancy accounted for about 10 percent of cancer-related deaths last year in the United States. By the end of 1998, an estimated 131,600 new cases of colorectal cancer were diagnosed, and 56,500 persons died from the disease.1
When localized to the bowel, colorectal cancer is highly treatable and often curable. With early detection, the five-year survival rate for patients with this malignancy is 92 percent.2 Although the incidence of colorectal cancer is increasing, the overall mortality rate is decreasing. Whether improved survival is a result of earlier detection, more accurate diagnosis, more effective treatment or the identification and removal of premalignant polyps is unclear.
A multidisciplinary panel of experts representing the American Cancer Society (ACS), the American College of Gastroenterology and the American Society of Gastrointestinal Endoscopists has made specific recommendations for the screening and surveillance of patients at average or increased risk for colorectal cancer (Table 1).3 The American Academy of Family Physicians (AAFP) and the U.S. Preventive Services Task Force also recommend sigmoidoscopy, starting at 50 years of age. Interestingly, persons at increased risk account for only 25 percent of colorectal cancers.3 Thus, most malignancies would be missed if screening were limited to the high-risk group.
| Risk category | Risk factors | Recommendations |
|---|---|---|
| Average risk | Age 50 years or older but asymptomatic and without any of the characteristics or situations indicating increased risk | Fecal occult blood screening yearly |
| Flexible sigmoidoscopy every 5 years or colonoscopy every 10 years or double contrast barium enema every 5 to 10 years | ||
| Increased risk | Close relative(s) have had colorectal cancer or an adenomatous polyp | Same recommendations as above, but screening is initiated when the patient is 40 years old |
| Family history of familial adenomatous polyposis | Genetic counseling/testing | |
| In a gene carrier, flexible sigmoidoscopy every12 months, beginning at puberty | ||
| Family history of hereditary nonpolyposis colorectal cancer | Genetic counseling/testing | |
| Examination of the entire colon every 1 to 2 years, starting when the patient is 20 to 30 years old | ||
| Examination of the entire colon yearly after the patient is 40 years old | ||
| History of adenomatous polyps | Colonoscopy 3 years after initial examination, with subsequent examinations, depending on the types of polyps detected | |
| History of colorectal cancer | Complete examination 1 year after colon surgery; if normal, reexamination of colon in 3 years; if still normal, reexamination in 5 years | |
| Inflammatory bowel disease | Surveillance colonoscopy every 1 to 2 years, beginning after 8 years of disease in the patient with pancolitis and after 15 years in the patient with left colon involvement only |
To date, no randomized, controlled trials have shown that flexible sigmoidoscopy reduces the mortality rate associated with colorectal cancer. However, in one case-control study4 it was found that in patients screened with rigid sigmoidoscopy the risk of fatal distal colon cancer was only 30 percent of the risk in unscreened patients.
Flexible sigmoidoscopy is a valuable procedural skill for family physicians. Many physicians acquire this skill in residency training and thus are more likely to use it later in practice.5 On January 1, 1998, Medicare began covering colorectal cancer screening. Physicians should now be able to convince more patients to undergo sigmoidoscopy.
The AAFP offers courses in flexible sigmoidoscopy and provides clinical workshops at its annual scientific assembly. Instructional materials are available to assist in sigmoidoscopy training.
Colorectal cancer screening procedures are performed with a rigid 25-cm scope or flexible 35- or 60-cm scopes. Flexible scopes are preferred because they provide superior visualization of the mucosa and facilitate complete bowel examination with minimal patient discomfort. The 60-cm scope affords direct visualization to the proximal sigmoid and descending colon. With this lengthy scope, approximately 50 percent of cancerous tumors and adenomas of the large bowel can be identified.6
Sigmoidoscopy is most commonly used to screen asymptomatic patients for precancerous changes and malignancies. Signs and symptoms such as diarrhea, proctitis and rectal pain can be evaluated by flexible sigmoidoscopy, but further examination using a barium enema or colonoscopy may be required in symptomatic patients.
Contraindications for sigmoidoscopy include acute peritonitis, acute diverticulitis, toxic megacolon and recent bowel surgery. Furthermore, it may be difficult to perform sigmoidoscopy successfully in patients who are uncooperative, or medically or emotionally unstable.7(pp56–7)
Abdominal cramping and bloating are the complications most frequently associated with sigmoidoscopy. Patients commonly experience mild to moderate discomfort throughout the examination. Stretching and traction from the instrument are primarily responsible for this discomfort, but overdistention as a result of air insufflation is also believed to play a role.7(pp117–25) Patients who have had previous abdominal surgery (e.g., hysterectomy) may experience more discomfort than patients who have not had such surgery.
Trauma induced by the scope can cause postprocedure bleeding. This bleeding is usually minor and self-limited.
Bowel perforation is the most serious complication of sigmoidoscopy. Fortunately, this complication is very rare, with an estimated incidence of one case per 5,000 to 10,000 examinations.7(pp117–25) Bowel perforation may be caused by excessive insertional force, overdistention with air or biopsy trauma. Perforation may require surgical intervention.
Patient Preparation
Before sigmoidoscopy is performed, the physician should provide educational materials and discuss the details of the examination with the patient. The physician must also review the risks of the procedure and obtain informed consent.
A complete medical history should be obtained to ensure the appropriateness and safety of the examination. Although medications do not have to be withheld for sigmoidoscopy, the physician should be aware of any drugs the patient is taking.
Bowel preparation is essential for adequate visualization during sigmoidoscopy. Different regimens may be used, but thorough emptying of the left side of the colon should be achieved. In most patients, the bowel can be adequately prepared by administering two Fleet enemas on the morning of the examination. Even better results may be achieved by adding an oral cathartic. An oral regimen alone, such as two 10-mg bisacodyl tablets (Dulcolax) with one bottle of magnesium citrate (taken the evening before the procedure), also provides good bowel preparation.8 Compared with enemas, oral regimens are often better accepted by patients.
Antibiotic prophylaxis for bacterial endocarditis associated with flexible sigmoidoscopy is optional, even when biopsy is performed. Prophylaxis is more commonly used in high-risk patients such as those with previous endocarditis or prosthetic valves.9 Generally, antispasmodics and sedatives are not indicated or needed.
Equipment
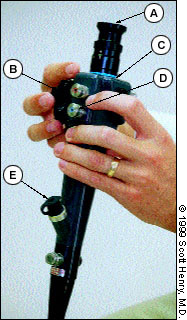
The flexible sigmoidoscope consists of a control head, an insertion tube and an umbilical cord. The control head houses the eyepiece, deflection knobs, valves (air-water and suction) and biopsy channel (Figure 1). An adapter can be placed over the eyepiece to provide visualization on a television monitor. Two deflection knobs control the up-down and right-left movements of the distal portion of the insertion tube. The air-water valve is generally located below the suction valve on the control head. Air is insufflated into the colon when a finger is placed over the aperture of the valve. The lens can be washed with water during the examination by rapidly depressing this valve. Suction can be used to removed mucus and liquid stool, thereby improving visualization; however, particulate matter cannot be removed through the suction channel.
Two types of sigmoidoscopic systems are available: a fiberoptic system and a video pathway system. The diameter of the insertion tube is greater with the video system. Although a video system is about twice as expensive as a fiberoptic system, it provides clearer images and allows a visual record to be obtained. A video system is helpful in documenting procedures and supporting examiner competence in training programs.10
The flexible sigmoidoscope may be used with a disposable sheath that protects the working surfaces of the instrument from contamination. The air-water and suction channels are located in the reusable section of the scope. Use of a disposable sheath reduces cleaning time, a very practical consideration for physicians who examine several patients in succession.11
The procedure room should be large enough that the examination can be performed with ease. The examination table should be adjustable, with adequate space around it to allow movement of the examiner and an assistant. A mobile cart is ideal for setting up the light source, suction pump and scope (Figure 2). Nonsterile gloves, 4- by 4-inch gauze pads and water-soluble lubricating jelly are the only additional supplies required. It is helpful to have a restroom adjacent to the procedure room for patient use.

Procedure
The patient is placed on the examination table in the left lateral position with knees drawn to the chest. A drape is placed over the patient from the waist down and positioned for optimal visualization.
The anus is carefully inspected for abnormalities such as external hemorrhoids, fissures or fistulas. A digital rectal examination is performed to palpate the rectum and, in male patients, the prostate gland.
After the digital rectal examination, the endoscopist changes gloves and prepares for the sigmoidoscopic procedure. Lubricant jelly is smeared on the scope to reduce patient discomfort.
With the index finger positioned along the well-lubricated scope tip, the endoscopist guides the tip of the instrument through the anus and into the rectum, where it is then advanced about 6 to 8 cm. During the learning stage, the endoscopist should advance and withdraw the scope tip to perfect the technique.
The scope should not be advanced against resistance. “Red-out” is the term used to describe what occurs when the tip of the scope is placed too close to the bowel wall mucosa. In this situation, the reflection of light off the vascularized tissue produces a red haze. By slightly withdrawing the scope, the endoscopist can again obtain a clear view of the bowel wall.
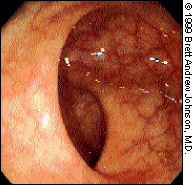
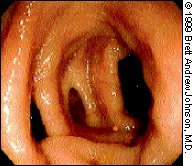
The rectum follows the curvature of the sacrum and extends about 12 cm to the rectosigmoid junction. The rectum generally has three folds (the valves of Houston) that must be negotiated (Figure 3). Typically, two of these semilunar folds are located on the patient's left side, and one is located on the right side. However, the number and location of these folds may vary.12
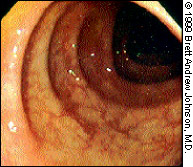
The translucency of the rectal mucosa allows blood vessels to be observed. The vasculature of the rectum is more marked than that of the sigmoid or descending colon (Figure 4).
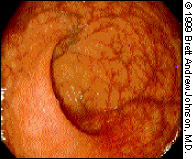
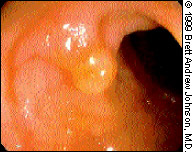
The sigmoid colon has prominent circular folds; the recesses between the folds are called “haustra” (Figure 5). This section of the colon is tortuous and mobile because it is not anatomically fixed. Various techniques can be used to negotiate the bends in the sigmoid colon. Fortunately, the descending colon is straight and relatively simple to navigate. The luminal folds become triangular in appearance as the distal colon is traversed.13
The colon is best and most easily inspected as the scope is withdrawn after full advancement. At this time, the lumen and folds of the colon should be examined for pathology, and the location of any abnormalities should be documented. So that no lesions are overlooked, the folds of the colon must be carefully inspected.
Once the scope has been withdrawn to the level of the rectum, it should be retroflexed to look down on itself (Figure 6). The J maneuver (described in the following section on techniques) provides an opportunity to view the distal area of the rectum, which is difficult to observe during insertion.14
After the distal colon is inspected, the scope tip is returned to its nondeflected position. When the lumen is again identified, air is suctioned for patient relief. Then the scope is removed from the rectum. Soapy water should be suctioned through the scope immediately to prevent drying and clogging of the channels.
Once the examination is completed, the physician should remind the patient to expect some abdominal cramping, gas or watery stools. The patient should be instructed to report more severe problems to the physician.
After the procedure, the sigmoidoscope must be cleaned and disinfected. A protocol must be established for the proper maintenance of equipment. Mechanical cleansing removes organic matter and reduces the risk of contamination. Disinfection eliminates the risk of pathogen transmission. For disinfection, the scope must be soaked in a 2 percent glutaraldehyde solution or another acceptable disinfectant in a properly ventilated room.15
Techniques
INSUFFLATION
Air is introduced into the colon by covering the opening on the water valve (the valve closest to the patient). Distention of the colon aids in visualization, but care must be taken not to overinflate the colon. Overinflation causes patient discomfort and may also create more acute bends for the scope to negotiate.
SUCTION
The insufflated air is removed from the colon by depressing the suction valve (the valve closest to the operator). Suction also removes mucus and liquid stool from the colon. However, the endoscopist must use suction carefully to avoid drawing the colonic mucosa into the scope. This can produce an area of localized mucosal swelling that resembles a polyp. A “suction polyp” typically resolves within a minute.7(pp56–7)
RINSE
If the view becomes blurred, the lens of the scope can be rinsed by rapidly and intermittently depressing the water valve. In addition, water can be flushed through the working or biopsy channel to clear debris from the mucosal surface, thereby facilitating a more complete examination.
BIOPSY
Not all family physicians perform biopsies during sigmoidoscopy. However, when performed safely and under the appropriate conditions, biopsy specimens can provide valuable information.
The biopsy forceps is advanced through a special port just below the control head of the scope. The instrument is directed at the lesion by moving the tip of the scope and then advancing the end of the forceps toward the lesion. It is useful to have an assistant open and close the biopsy forceps. After the lesion is grasped, the endoscopist withdraws the forceps slightly to see if the lesion moves away from the bowel wall. If so, the endoscopist uses a quick snap of the forearm and wrist to remove the lesion. Bleeding at the biopsy site is usually minimal.
It is preferable to perform biopsies when withdrawing the scope and to start with more proximal colonic lesions. A biopsy should not be performed on a vascular lesion or within a diverticulum.16
HOOK AND PULLBACK
The hook and pullback technique is helpful in straightening the sigmoid colon. In this technique, the tip of the scope is deflected 30 to 90 degrees behind a mucosal fold, and the scope is withdrawn 5 to 10 cm. This action pulls the segment of colon downward.17
DITHERING-TWIST MANEUVER
The dithering-twist maneuver pleats the colon onto the endoscope, effectively allowing more colon to be examined. For this maneuver, the tip of the scope is deflected about 30 degrees in the direction of the lumen. As the shaft is advanced 3 to 6 cm, it is twisted counterclockwise 45 to 60 degrees. The process is then reversed by withdrawing and twisting the scope clockwise to its original position. The maneuver is repeated in a rhythmic fashion.18
JIGGLING
The jiggling technique involves moving the scope in and out in 5- to 10-cm increments. A view of the lumen is maintained while the maneuver is performed.
RETROFLEXION J MANEUVER
From the anal verge, the scope tip is positioned approximately 10 cm into the rectum. The tip is then deflected maximally, and the scope is advanced 5 to 10 cm along the bowel mucosa. This inverts the scope tip to allow visualization of hemorrhoids and other pathologic conditions in the rectum. At this point the scope can be twisted for a 360-degree view of the anorectal region.14
Abnormal Findings
A form should be used to document all normal and abnormal findings discovered on sigmoidoscopic examination. This form can be used to review the examination results with the patient.
Patients with many of the pathologic conditions discussed in the following sections should be referred for colonoscopy. Follow-up depends on the endoscopic findings and the individual patient's level of risk.
HEMORRHOIDS
Hemorrhoids originating above the dentate line are called “internal,” and those originating below this line are termed “external.” Internal hemorrhoids are painless and can be seen on retroversion (Figure 7). Typically, they consist of bluish, engorged veins near the anus. External hemorrhoids can be easily observed when the anus is examined with the buttocks spread apart. These varicose dilatations can be quite painful, especially if they are thrombosed.

ANAL FISSURES
Anal fissures are painful mucosal tears that generally occur in the posterior midline but may also occur in the anterior midline. Both external inspection and anoscopic examination are required to identify anal fissures. Tears found other than in the midline position should raise the suspicion of inflammatory bowel disease, immunosuppression, syphilis or carcinoma.19
RECTAL CANCERS
Rectal cancers may appear as large fungating masses or an isolated ulcer. These malignancies are usually painless but tend to bleed.
DIVERTICULA
A diverticulum is a blind sac or pouch that typically develops as a result of long-standing elevated intraluminal pressure7(pp56–7) (Figure 8). The physician must take care not to mistake the opening of a diverticulum for the colonic lumen and advance the scope into it. Diverticulitis occurs when a diverticulum becomes infected.
CROHN'S COLITIS
Crohn's disease or colitis involves both the mucosa and the submucosa. Crohn's ulcers are surrounded by normal-appearing mucosa (Figure 9). “Cobblestoning” is the term used to describe an area of uniform nodularity caused by submucosal edema. Crohn's disease or colitis can spare segments of the bowel. The rectum is involved in only one half of affected patients.13

ULCERATIVE COLITIS
Ulcerative colitis affects the mucosal layer of the colon. The rectum is involved in approximately 95 percent of patients with this disease. The epithelium is red, granular and friable. Superficial ulcerations occur and are surrounded by erythematous mucosa.13 Toxic megacolon is a serious complication of ulcerative colitis.
PSEUDOMEMBRANOUS COLITIS
Pseudomembranous colitis is characterized by a yellow membrane that covers the mucosal surface. The underlying mucosa is inflamed and at times hemorrhagic. If only the proximal colon is affected, the mucosa may appear normal on sigmoidoscopic examination.
POLYPS
Colorectal polyps are classified as adenomatous or hyperplastic. The adenomatous polyp is a premalignant lesion. About 5 percent of large-bowel adenomas undergo malignant transformation.20 Factors affecting this transformation include polyp size, villous features and the presence of severe dysplasia. Surface irregularities such as ulceration, nodularity and firmness can be signs of cancerous invasion.
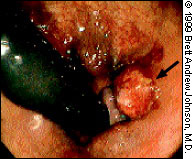
Adenomatous polyps are either pedunculated or sessile. A pedunculated polyp is attached to the wall of the colon by a stalk (Figure 10), whereas a sessile polyp is attached directly to the wall (Figure 11). Benign features include sharp demarcation between the adenoma and the bowel wall, absence of ulceration and lack of fixation to the submucosa.

A hyperplastic polyp is typically less than 6 mm in size and appears as a small sessile protrusion. It is the most common benign polyp of the large intestine, particularly in the distal colon and rectum. Endoscopically, a hyper-plastic polyp is very difficult to distinguish from an adenoma.7(pp56–7)
ADENOCARCINOMA
Adenocarcinoma of the rectum usually appears as a polypoid or exophytic lesion with a diameter of 1 to 10 cm. The lesion typically is firm, has an irregular contour and is associated with ulcerations and necrosis (Figure 12). In patients with localized spread, the lesion may form a ring within the lumen and therefore obstruct the rectal canal.

Primary Prevention of Colon Cancer
It is the role of the family physician to review lifestyle changes with patients to reduce the risk of colorectal cancer. Patients should be advised to do the following:
Engage in 30 minutes of physical activity each day.
Eat foods that are low in fat and high in fiber. The ACS recommends eating at least five servings of fruits and vegetables every day and six servings of other foods from plant sources (e.g., breads, rice, pasta and grains).
Stop smoking.
Limit alcohol consumption.
A recent study21 suggested that nonsteroidal anti-inflammatory drugs and aspirin may reduce the risk of colorectal cancer. It is also important to encourage the close relatives of a patient with colorectal cancer to undergo screening.
With the combination of primary prevention and improved screening, the number of colorectal cancer cases should decrease significantly in the future.