
Am Fam Physician. 1999;59(6):1547-1556
See related patient information handout on vulvodynia, written by the author and Elizabeth S. Smoots, M.D..
Vulvodynia is a problem most family physicians can expect to encounter. It is a syndrome of unexplained vulvar pain, frequently accompanied by physical disabilities, limitation of daily activities, sexual dysfunction and psychologic distress. The patient's vulvar pain usually has an acute onset and, in most cases, becomes a chronic problem lasting months to years. The pain is often described as burning or stinging, or a feeling of rawness or irritation. Vulvodynia may have multiple causes, with several subsets, including cyclic vulvovaginitis, vulvar vestibulitis syndrome, essential (dysesthetic) vulvodynia and vulvar dermatoses. Evaluation should include a thorough history and physical examination as well as cultures for bacteria and fungus, KOH microscopic examination and biopsy of any suspicious areas. Proper treatment mandates that the correct type of vulvodynia be identified. Depending on the specific diagnosis, treatment may include fluconazole, calcium citrate, tricyclic antidepressants, topical corticosteroids, physical therapy with biofeedback, surgery or laser therapy. Since vulvodynia is often a chronic condition, regular medical follow-up and referral to a support group are helpful for most patients.
Vulvodynia is frequently misdiagnosed. In a general gynecologic practice population, the prevalence of this condition may be as high as 15 percent.1 Before the 1980s, very little was written about vulvodynia. In the 1980s, renewed interest was generated with the publication of articles by Friedrich, Lynch and McKay.2–4
Epidemiology
Vulvodynia is a syndrome of unexplained vulvar pain that is frequently accompanied by physical disabilities, limitation of daily activities (such as sitting and walking), sexual dysfunction and psychologic disability.2 Originally suggested by McKay,4 the term “vulvodynia” has also been suggested by the International Society for the Study of Vulvar Disease Task Force to describe any vulvar pain. The incidence and prevalence of vulvodynia have not been well studied.1 Age distribution for the condition may range from the 20s to the 60s, and it is limited almost exclusively to white women.2 Obstetric and gynecologic history is usually unremarkable. Risk-taking sexual behavior is rare, and few patients have a history of sexually transmitted diseases.5 Vulvar pain usually has an acute onset, at times associated with episodes of vaginitis or certain therapeutic procedures of the vulva (cryotherapy or laser therapy). In most cases, vulvodynia becomes a chronic problem lasting months to years. Vulvar pain is frequently described as burning or stinging, or a feeling of rawness or irritation.4
Most patients consult several physicians before being diagnosed. Many are treated with multiple topical or systemic medications, with minimal relief. In some cases, inappropriate therapy may even make the symptoms worse.6 Since physical findings are few and cultures and biopsies are frequently negative, patients may be told that the problem is primarily psychologic, thus invalidating their pain and adding to their distress.7(pp1–15)
Diagnostic and Management Challenges
ILLUSTRATIVE CASE 1
A 23-year-old woman was treated twice for a suspected urinary tract infection while traveling in Europe. The patient did not know what antiobiotic she had taken. On returning to the United States, she continued to experience dysuria and urgency with vaginal soreness, slight itching and dyspareunia. Urinalyses, urine cultures and vaginal and cervical cultures were negative. Over the course of two months, the patient went to emergency departments twice and visited four different family physicians. She was treated with numerous antibiotics, including trimethoprimsul-famethoxazole, cephalexin and ciprofloxacin, for presumed cystitis. She also was treated with oral fluconazole and over-the-counter topical anticandidal preparations for presumed candidal infection, with only temporary relief.
During the following two months, the patient experienced dyspareunia with intermittent vulvar pain and irritation. She subsequently saw four gynecologists, a urologist and two primary care physicians. Pelvic examination revealed erythema of the posterior fourchette and a reaction of mild tenderness on swab test. A biopsy of this area was normal. The patient was treated with doxycycline for possible cervicitis; the symptoms were not relieved. She was then given a diagnosis of vulvodynia and was prescribed gradually increasing dosages of amitriptyline, along with oral calcium gluconate three times daily and a low-oxalate diet. She was referred to a support group for persons with vulvodynia and to a physical therapist specializing in women's health problems for pelvic strengthening, relaxation training and biofeedback training. Over the next three months, the patient reported a 70 to 90 percent improvement in her symptoms, with occasional mild exacerbations.
ILLUSTRATIVE CASE 2
A 45-year-old woman with a history of one term pregnancy developed urgency, erythema in the vulvar area and irritation at the base of the clitoris that began suddenly after intercourse one evening. Subsequent symptoms included burning, rawness and dyspareunia, which increased with walking, sitting and intercourse, and also increased one week before menses. The use of terconazole cream caused further burning and irritation. Over the next five months the patient saw a nurse practitioner and two family physicians. She received treatment numerous times for yeast vaginitis and bacterial vaginosis with topical antifungal medications, fluconazole and metronidazole gel. Any improvement was temporary, and the symptoms invariably returned.
Vaginal cultures grew various enteric organisms, and no yeasts were detected on KOH examination. Conjugated estrogen vaginal cream gave no significant relief. Over the following two months the patient saw two gynecologists and was diagnosed with vestibulitis. She was treated with triamcinolone-nystatin cream for two months and felt improvement in the first week but later developed further irritation of the vulvar and clitoral area. No biopsies were performed. She was referred to a third gynecologist, who instructed her to stop all topical medications. She began taking calcium citrate three times daily, started a low-oxalate diet and was referred to a vulvar pain support group. Over the next year, she was treated with fluconazole, 150 mg once weekly for two months, and then once every other week for two months. She also began biofeedback training and physical therapy for pelvic muscle relaxation and strengthening. The patient underwent a total of two and one half years of treatment. During her last year of treatment, she experienced a 90 percent improvement in symptoms.
Subsets of Vulvodynia
| Subset of vulvodynia | Typical history | Physical findings | Treatment |
|---|---|---|---|
| Cyclic vulvovaginitis | Pain is worse just before or during menses Pain is exacerbated by intercourse (especially on the next day) Some relatively symptom-free days Frequent use of antibiotics for other conditions | Variable erythema and edema Minimal vaginal discharge | Refer to support group Fluconazole (Diflucan), 150 mg weekly for 2 months, then twice monthly for 2 to 4 months Physical therapy with biofeedback Low-oxalate diet Oral calcium citrate (Citracal) |
| Vulvar vestibulitis syndrome | Usually premenopausal Entry dyspareunia or pain with insertion of tampon Possible history of carbon dioxide laser therapy, cryotherapy, allergic drug reactions or recent use of chemical irritants | Positive swab test (vestibular point tenderness when touched with cotton swab) Focal or diffuse vestibular erythema | Refer to support group |
| Topical estradiol cream, 0.01% (Estrace Vaginal Cream) twice daily | |||
| Intralesional interferon injection | |||
| Physical therapy with biofeedback | |||
| Low-oxalate diet | |||
| Oral calcium citrate | |||
| Dysesthetic vulvodynia (essential vulvodynia) | Usually postmenopausal or perimenopausal Diffuse, unremitting burning pain that is not cyclic Less dyspareunia or point tenderness than in vulvar vestibulitis | Usually no erythematous cutaneous changes | Refer to support group Tricyclic antidepressants in gradually increasing amounts (6 or more months of therapy) Physical therapy with biofeedback |
| Papulosquamous vulvar dermatoses | Itching is prominent Variable chronic symptoms | Erythema Thick and/or scaly lesions May have additional skin lesions elsewhere on body Biopsy required | Topical corticosteroids (2.5% hydrocortisone ointment or 0.1% triamcinolone ointment) for psoriasis, lichen planus, contact dermatitis, lichen simplex chronicus Topical 2% testosterone propionate for lichen sclerosis Topical imidazole creams for tinea cruris |
| Vesiculobullous vulvar dermatoses | Itching or burning Variable chronic symptoms | Blisters or ulcers that are not related to scratching Biopsy may be required | Depends on condition |
| Neoplastic vulvar lesions | Variable persistent lesion | Variable; possible white plaques, ulcers or erythema | Refer to gynecologic oncologist |
| Biopsy required | |||
| Vestibular papillomatosis | Normal anatomic variant Variable history of human papillomavirus infection Many are asymptomatic | Papillomatous appearance of mucosal surfaces Biopsy to rule out koilocytosis or human papillomavirus infection if symptomatic or questionable | No treatment required Treat for human papillomavirus infection only if biopsy is positive |
VULVAR VESTIBULITIS SYNDROME


Chronic vestibulitis lasts for months to years, and patients may experience entry dyspareunia and pain when attempting to insert a tampon.6,8 The etiology of vulvar vestibulitis syndrome is unknown. Some cases seem to be provoked by yeast vaginitis. Other suspected causes include recent use of chemical irritants, a history of destructive therapy such as carbon dioxide laser or cryotherapy, or allergic drug reactions.5 When surgical specimens were evaluated by polymerase chain reaction, human papillomavirus was present in many women with vulvar vestibulitis syndrome.9–13
Histologic examination of symptomatic vestibular tissue has confirmed the presence of mixed chronic inflammatory infiltrates in the superficial stroma, but inflammatory cells have not been found to invade the vestibular glands or gland lumens, vessels or nerves.2
CYCLIC VULVOVAGINITIS
Cyclic vulvovaginitis is probably the most common cause of vulvodynia and is believed to be caused by a hypersensitivity reaction to Candida.14,15 While vaginal smears and cultures are not consistently positive, microbiologic proof should be sought by obtaining candidal or fungal cultures during an asymptomatic phase. Pain is typically worse just before or during menstrual bleeding. It also may be exacerbated after intercourse, especially on the following day.4,8 Findings on pelvic or colposcopic examination are usually normal. The diagnosis of cyclic vulvitis is made retrospectively based on the patient's report of cyclic symptomatic flare-ups (or, conversely, symptom-free days). The diagnosis is suggested prospectively by the patient's report of symptomatic improvement after the administration of long-term topical or systemic anticandidal therapy.3
DYSESTHETIC VULVODYNIA
Dysesthetic vulvodynia (essential vulvodynia) typically occurs in women who are peri- or postmenopausal.16 Pain that occurs in women with this subtype of vulvodynia is usually a diffuse, unremitting, burning pain that is not cyclic. Patients with dysesthetic vulvodynia have less dyspareunia or point tenderness than patients with vulvar vestibulitis syndrome.16 The physical examination shows no evidence of vestibulitis or cutaneous changes.6 Urethral or rectal discomfort is often associated with vulvar pain.5 The hyperesthesia is believed to result from altered cutaneous perception, either centrally or at the nerve root. Patients describe burning pain similar to that occurring in cases of postherpetic neuralgia or glossodynia (burning tongue syndrome).16 Some authors believe that pudendal neuralgia (pain along the pudendal nerve) is one of the causes of essential vulvodynia.17
VULVAR DERMATOSES
Vulvar dermatoses may be manifested by itching and, in some cases, pain (Figures 3 through 5). Vulvar dermatoses include papulosquamous (thick and scaly) lesions. Erosions or ulcers may result from excessive scratching. If the patient has blisters or ulcers and denies scratching, the cause may be a vesiculobullous disease. Differential diagnoses of papulosquamous lesions and vesiculobullous lesions are included in Table 2.6 Neoplastic lesions include extramammary Paget's disease, squamous cell carcinoma, lichen sclerosis and vulvar intraepithelial neoplasia.6 Colposcopy and biopsy as indicated are recommended to rule out dermatoses or neoplastic lesions (Figure 6). A recent study showed the most common cause of symptomatic vulvar disease (itching or burning) to be dermatitis or another dermatosis.18


| Papulosquamous vulvar dermatoses |
| Psoriasis |
| Tinea cruris |
| Lichen planus |
| Lichen sclerosis |
| Seborrheic dermatitis |
| Contact or irritant dermatitis |
| Lichen simplex |
| Bullous dermatoses with potential involvement of the vulva |
| Erythema multiforme |
| Bullous pemphigoid |
| Pemphigus |
| Benign familial pemphigus |
| Systemic diseases with potential involvement of the vulva |
| Behçet's disease |
| Lupus erythematosus |
| Reiter's disease |
PAPILLOMATOSIS
Vestibular papillomatosis is the term describing the presence of multiple small (1-to 3-mm) papillae over the entire inner labia (Figure 7). These papillae are probably congenital in origin and are a normal anatomic variant.19 A link with human papillomavirus has not been confirmed.20,21 Patients with vulvar pain and papillomatosis should undergo a colposcopically directed biopsy to rule out pathology. The significance of papillomatosis identified in the vulvar vestibule with acetowhitening is uncertain.22

Evaluation
The evaluation of patients with vulvar vestibulitis or vulvodynia should include a thorough history, pelvic examination, fungal and bacterial cultures, and KOH microscopic examination. Biopsy of any suspicious areas should be performed using acetowhitening and/or colposcopy to rule out dermatoses or neoplastic lesions.6 A swab test (which involves palpation of the vestibulum with a moist, cotton-tipped swab) may elicit point tenderness or sharp pain in the posterior vestibulum, the anterior vestibulum, or both.6
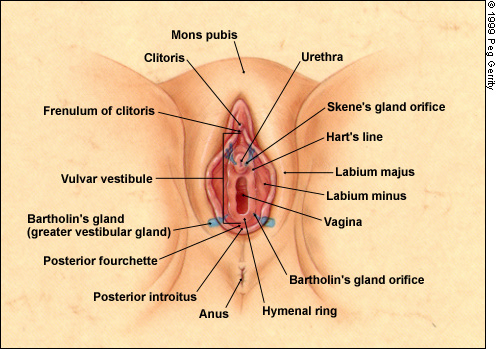
In patients with vulvar vestibulitis, erythema may commonly be visualized at the 5 and 7 o'clock positions or on a horseshoe-shaped area of the lower vestibulum.23 The vestibule comprises the area between the labia minora and the hymenal ring, which marks the beginning of the vaginal mucous membrane. It extends from the frenulum of the clitoris anteriorly to the fourchette of the vaginal introitus posteriorly. This area includes the Bartholin's glands, Skene's glands and numerous minor vestibular glands (Figure 8).
Treatment and Management of Vulvodynia and Vulvar Vestibulitis
MEDICAL THERAPY
Some treatments are specific to the subtype of vulvodynia that can be most closely associated with the patient. Vulvodynia is multifactorial in cause, and each subset probably has a different etiology. Cyclic vulvovaginitis is believed to be a reaction to yeast, which may be detected at times and not detected at other times with KOH preparation or fungal cultures. Some physicians may use a test for anticandidal antibodies in directing treatment. Because of the link with Candida, treatment for cyclic vulvovaginitis may include anticandidal medication even if cultures are not positive. One regimen is fluconazole (Diflucan), 150 mg orally once weekly for two months and then once every other week for two months. Other anticandidal agents that may be used include long-term therapy with topical nystatin (Micostatin Cream, Mytrex Cream), miconazole nitrate (Monistat-Derm Cream) and clotrimazole (Lotrimin).4
Vulvar vestibulitis syndrome has been treated successfully in some cases with topical estrogen cream (about a pea-sized amount), applied two times a day for four to eight weeks, or longer. Intralesional injections of interferon in 13 women with vulvar vestibulitis resulted in significant improvement of dyspareunia in 50 percent.24 Severe, recalcitrant cases may be treated with vestibulectomy or laser therapy. Tricyclic agents (amitriptyline [Elavil], imipramine [Tofranil] or desipra mine [Norpramin]) have been successful in the treatment of dysesthetic vulvodynia. A recommended regimen begins with 10 mg daily, gradually increasing to 40 to 60 mg daily. Patients should continue taking the highest tolerable dosage that gives symptom relief for four to six months and then gradually decrease the dosage to the minimum amount required to control symptoms.14
Since some patients do not wish to take a psychiatric drug, it is important to explain that the medication is being used for its effect on cutaneous nerves. In one study, the average time required for effective treatment with amitriptyline was seven months, after which therapy was either discontinued or tapered.14
Other treatments that have been helpful in patients with vulvodynia are a low-oxalate diet and, in some cases, the addition of oral calcium citrate (Citracal), two tablets (200 mg/950 mg each) orally three times a day to neutralize oxalates in the urine. One theory is that oxalate may irritate the vestibulum and may be a contributing cause to vulvodynia pain over a long period.7(p16), 25
Therapy with potent topical corticosteroids should be limited to brief or short-term use. Long-term use may induce telangiectasias, skin friability, striae formation and easy bruising. Potent steroids can also cause periorificial dermatitis, a rebound inflammatory reaction with erythema and a burning sensation that occurs as the steroid is withdrawn. A cycle of vulvar dermatitis may become worse as the patient treats the erythema and discomfort with the same potent topical steroids that started the problem.6 Self-help tips for patients with vulvodynia vulvar vestibulitis are included in the patient information handout that follows this article.
Physical Therapy and Biofeedback
Since vaginal muscle spasm aggravates the pain and discomfort of vulvodynia, physical therapy using biofeedback and gynecologic instruments has been successful in many patients with vaginismus (spasm of the vaginal muscle) and instability of the pelvic floor. Biofeedback training helps patients learn exercises to strengthen weakened pelvic floor muscles and to relax these same muscles, with a resultant reduction in pain.
Surgical and Laser Therapy
Laser or surgical treatment should be reserved for use in cases in which all forms of medical treatment have failed. Many cases of vulvar vestibulitis that are refractive to medical therapy respond to vulvar vestibulectomy or treatment with excited dye laser. According to Marinoff and Turner,26 surgery should be reserved for use in patients with pain of at least six months' duration, pain that partly or completely prevents sexual intercourse and patients who have undergone failed treatment for a specific subset of vulvodynia or in whom no cause can be established. Surgical excision of vulvar tissue containing vestibular glands has been reported to alleviate symptoms in up to two thirds of patients.24,27 Complications include wound hematoma, partial or complete wound dehiscence, uneven healing requiring minor revision, and stenosis of the Bartholin's duct with cyst formation.26
Flashlamp-excited dye laser therapy for the treatment of idiopathic vulvodynia has been used with some success and may reduce the need for resective surgery in many cases.28
Psychologic Considerations
Vulvodynia may cause drastic alterations in lifestyles. It may decrease the patient's ability to walk, exercise, sit for long periods or participate in sexual activities. All of these normal activities may exacerbate the vulvar pain.5 Many women with vulvodynia have been diagnosed with a psychologic problem because of the lack of physical findings.15 Patients may become anxious or angry as diagnosis is delayed after numerous physician visits and as their concerns increase that the condition may be a serious health problem. Many patients with vulvodynia worry that they will never recover.
The prevalence of physical and sexual abuse in patients with vulvodynia does not appear to be increased.29 Family physicians can be of immense help by making the diagnosis of vulvodynia as early as possible, identifying a specific subtype, educating the patient and beginning a management plan. Patients should be supported with the acknowledgement that vulvodynia does not appear to be a psychosomatic condition and that it has no predisposition toward cancer or other life-threatening conditions. It should be explained that improvement will occur with appropriate treatment, but that successful treatment may take months or years, and patients may have intermittent exacerbations and remissions.
Many patients benefit from referral to a group that provides information and emotional support.
Final Comment
Research indicates that vulvodynia and vulvar vestibulitis are being identified by physicians with increasing frequency. Since the physician “sees only what he already knows,” family physicians must be aware of and recognize this condition early. Failure to consider vulvodynia as the cause of vulvar pain is the most common reason for misdiagnosis.
Vulvodynia is a multifactorial problem with subsets that may overlap. Proper management is based on identification of the subsets of vulvodynia and identification of any concurrent infections that may be appropriately treated. Family physicians working together with gynecologists who are experienced in treating patients with vulvodynia can properly diagnose vulvodynia, identify subsets and institute the management plan that can best benefit the patient. Family physicians are in an ideal position to help and support the patient psychologically with validation, education and referral to support groups. Appropriate medical treatment should be instituted and, when indicated, physical therapy with biofeedback training should be considered.
More research is needed to further identify patients with subsets of vulvodynia and to evaluate various treatment modalities.