
Am Fam Physician. 1999;59(7):1919-1920
An 86-year-old woman presented to the emergency department with worsening pain in the left groin and a two-day history of nausea and poor oral intake. She had been in fair health until the day before, when she presented to her private physician with pain in her left groin and occasional abdominal discomfort, but no vomiting, fever or change in bowel habits. She had a past history of hypertension, peptic ulcer disease, rheumatic heart disease and diverticular disease that required a colostomy.
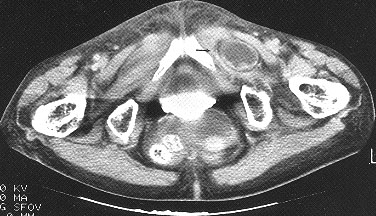
On physical examination, the patient was afebrile with normal vital signs. Her abdomen was soft with hypoactive bowel sounds; no palpable masses or lesions were noted. She had mild tenderness but no guarding or rebound on palpation of the left groin region. Results from laboratory tests were unremarkable. A plain abdominal radiograph showed a few dilated loops of small bowel but no air-fluid levels. The findings of a computed tomographic (CT) scan are shown in the accompanying figure.
Question
Discussion
The answer is D: incarcerated obturator hernia. This patient underwent surgery and was found to have an incarcerated obturator hernia on her left side. Following successful reduction and repair of the hernia, she was discharged in stable condition after six days of hospitalization.
An obturator hernia is a rare but serious condition that occurs most often in elderly, debilitated women; hence the nickname, “little old lady's hernia.” Obturator hernias are up to five times more common in women than in men and may be secondary to anatomic changes in the pelvis in elderly women or to hormonal changes, such as lack of estrogen. Signs and symptoms are often nonspecific, making a preoperative diagnosis uncommon.1 Obturator hernias have the highest mortality rate (range: 13 to 40 percent) of all abdominal wall hernias.2 They typically manifest as a small bowel obstruction with cramping, abdominal pain and vomiting, when the hernia passes through the obturator foramen or canal.
The most specific finding for an obturator hernia is pain that extends down the medial aspect of the thigh on abduction, extension or internal rotation of the lower extremity. This is referred to as a positive Howship-Romberg sign.3 A mass may be palpated on rectal examination if the hernia sac is incarcerated or strangulated. Since Howship-Romberg sign is present in less than one half of patients, physicians should suspect an obturator hernia in any elderly debilitated woman with any degree of bowel obstruction. A CT scan is the study of choice for diagnosis of an otherwise stable patient.
Of the other possible multiple-choice answers, lymphomas are the most common noncarcinomatous malignant tumors of the large intestine; however, they typically present with some degree of lymphadenopathy associated with abnormal values on laboratory tests, such as an elevated lactic dehydrogenase level.
Adhesions from previous surgeries are the most common cause of mechanical obstruction of the small bowel. Patients presenting with small bowel obstruction secondary to adhesions typically have colicky abdominal pain, vomiting and abdominal distention. Dilated loops of small intestine can be seen on radiographs in these patients; however, masses, such as those found on the CT shown here, will not be present. A follow-through radiographic series of the small bowel should reveal the obstruction higher in the abdomen.
Patients with an incarcerated inguinal hernia would have a mass that could become gangrenous without surgical intervention. Adenocarcinomas of the colon may manifest as changes in bowel habits, with alternating constipation and increased frequency of defecation, gross blood in the stool and symptoms of obstruction. Masses in the large colon and retroperitoneal adenopathy may also be seen on the CT scan.