
Am Fam Physician. 1999;59(10):2773-2782
See related patient information handout on shoulder instability, written by the authors of this article.
The term “shoulder instability” constitutes a spectrum of disorders that includes dislocation, subluxation and laxity. Anterior instability is the most common form of glenohumeral instability and may be associated with nerve injury. The diagnosis of anterior, posterior or multidirectional instability is based on a thorough history and physical examination that includes specific provocative maneuvers. The load-and-shift test, the relocation test, the drawer test, the sulcus test and the anterior apprehension test are useful for assessment of the shoulder. Radiographic studies should include special views to delineate specific lesions, such as a Bankart lesion and a Hill-Sachs defect. Early surgical intervention may be a consideration, especially in younger patients. Recent studies suggest that surgical intervention after the first dislocation may reduce the rate of recurrence. Rehabilitation is accomplished in four phases, beginning with rest and pain control and proceeding to isometric and isotonic exercises. The goal is for the patient to reach 90 percent strength in the injured shoulder compared with the uninjured shoulder.
Shoulder injuries can be devastating in young athletes, particularly in those whose sport requires strong overhead motions, such as baseball, softball, volleyball and swimming. A decrease in shoulder function may end an athlete's career. Common shoulder injuries in athletes include acute dislocation and acute subluxation of the glenohumeral joint, chronic subluxation, impingement syndromes, rotator cuff injuries and acromioclavicular joint injuries.1
Shoulder instability, characterized by subluxation or dislocation of the glenohumeral joint, is an increasingly recognized problem in young athletes, although its incidence is difficult to determine. The prevalence of shoulder injuries, however, has been reported to range from 4 to 8 percent of all injuries sustained in an active population.2,3
The term “shoulder instability” refers to a spectrum of disorders that includes dislocation, subluxation and laxity. Dislocation is defined as complete loss of the humeral articulation with the glenoid fossa as a result of acute trauma. Subluxation is a partial loss of the articulation to the degree that symptoms are produced. It is caused by repetitive trauma.1,4,5 As with subluxation, laxity is defined as a partial loss of the glenohumeral articulation; however, patients with laxity are asymptomatic.
Shoulder Anatomy
The glenohumeral joint is one of three joints that constitute the shoulder girdle; the other two are the acromioclavicular and the sternoclavicular joints. In addition to these three joints, a fourth critical articulation is the scapulothoracic joint.
The glenoid fossa is a shallow structure, lending minimal bony support for the humeral head4–6 (Figure 1). Therefore, stability of the glenohumeral joint depends on soft tissue integrity, including the rotator cuff muscles, the cartilaginous glenoid labrum and the joint capsule. The joint capsule contains the glenohumeral ligaments.4 These ligaments, along with the rotator cuff muscles and the glenoid labrum, can be further divided into static and dynamic stabilizers of the glenohumeral joint.
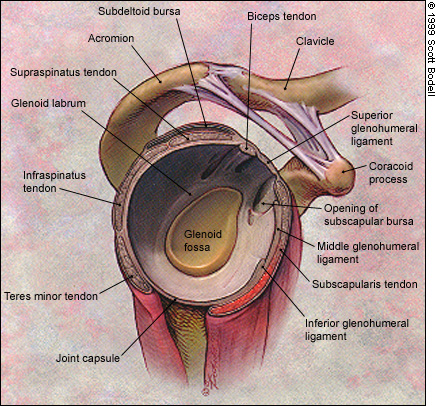
The dynamic stabilizers include the rotator cuff muscles, which consist of the subscapularis, the supraspinatus, the infraspinatus and the teres minor, and the scapular muscles, including the serratus anterior, the pectoralis and the latissimus dorsi (Figure 2). These larger muscles that surround the shoulder are responsible for controlling scapular stability and the glenoid position and for producing the forces necessary for glenohumeral movements.7
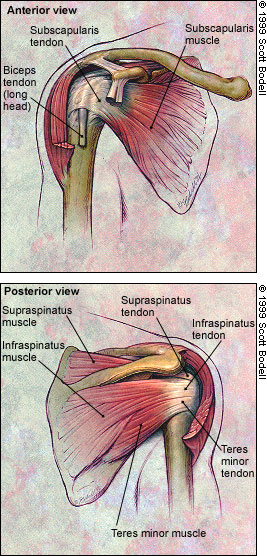
Scapular stability is an important factor in the overall stability of the shoulder, much like the foundation of a building. The long head of the biceps tendon, which attaches superiorly on the glenoid labrum, is also a stabilizer but may not be truly dynamic.5,7,8 The primary function of the rotator cuff is to maintain the humeral head in the glenoid fossa throughout the shoulder's range of motion. The rotator cuff accomplishes this function through eccentric actions, with the muscles maintaining their strength while they lengthen during movement of the joint.4,9
The glenoid labrum and the joint capsule serve as the static stabilizers by deepening the glenoid fossa and maintaining negative intra-articular pressure of the joint.4 The superior, middle and inferior glenohumeral ligaments attach to the labrum, and their function is very important for glenohumeral static stability.4
Types of Instability
Attempts have been made to classify different types of shoulder instability, according to degree of laxity, frequency of symptoms and specific anatomic lesion.4,5,10 Classifying instability by direction (i.e., anterior, posterior or multidirectional), however, is helpful in understanding the cause of the instability and in formulating the approach to diagnostic testing and treatment.4,5,10,11 This system is used by most orthopedic surgeons and primary care physicians specializing in sports medicine.5,10
ANTERIOR INSTABILITY
Anterior instability, the most common type of glenohumeral instability, can be due to either dislocation or subluxation. As many as 85 to 95 percent of all shoulder dislocations occur anteriorly.6,7 Men aged 18 to 25 years are most susceptible to this injury.6,7 Anterior glenohumeral injuries usually occur when the shoulder is in abduction and external rotation, the weakest position of the glenohumeral joint biomechanically.1 It has been termed the “classic position” for anterior instability.5,6
Anterior dislocations occur equally in dominant and nondominant extremities; associated rotator cuff tears are infrequent before age 40.6 A patient with anterior dislocation presents holding the arm in slight abduction and internal rotation and reports pain with any attempt to rotate the arm. A mass may be palpable over the anterior shoulder.11 The patient may also report transient loss of sensation, and numbness and tingling of the involved extremity, termed the “dead arm” syndrome. This syndrome may also occur with subluxation.1,4,7 Axillary nerve injury is not unusual with anterior dislocations. Typically, axillary nerve injury is manifested by loss of sensation over the lateral deltoid as well as decreased strength of the deltoid.1,11
Anterior subluxation is common in patients who have had an acute dislocation. Subluxation may also become a problem secondary to overuse microtrauma and underlying rotator cuff weakness, a common mechanism of injury in baseball pitchers.8
POSTERIOR INSTABILITY
Posterior instability, especially traumatic dislocation, is less common than anterior instability. While posterior instability may be the result of trauma in athletes, it typically stems from an episode of generalized muscle contraction, such as a seizure or a severe electric shock.5,11–13 After posterior dislocation, the shoulder adductors and internal rotators, which are generally stronger than the abductors and external rotators, contract, adduct, flex and internally rotate the humeral head.13 The humeral head loses its congruence with the posterior labrum and glenoid, dislocating posteriorly. Standard shoulder radiographs do not demonstrate posterior displacement of the humeral head. Therefore, this diagnosis is missed acutely about 50 percent of the time.13,14
The hallmark of posterior dislocation of three or four days' duration is loss of external rotation of the shoulder, along with prominence of the humeral head on the posterior shoulder.11 Posterior instability in athletes presents as subluxation resulting from repetitive microtrauma and the development of posterior rotator cuff weakness.4,12,13,15 Offensive linemen are particularly vulnerable to this injury because of the forward-flexed and internally rotated shoulder position needed for blocking.12
MULTIDIRECTIONAL INSTABILITY
Multidirectional instability is associated not with an acute dislocation but rather with congenital hyperlaxity of the glenohumeral joint capsule or the development of generalized joint laxity in association with rotator cuff weakness.4,16 Patients with congenital hyperlaxity of the shoulder generally have laxity of other joints as well. Capsular laxity may develop in athletes without congenital laxity if they perform repetitive overhead motions. When joint laxity is accompanied by a rotator cuff injury, pathologic multidirectional instability may occur. Patients may note weakness and vague pain with activity. The weakened rotator cuff allows subluxation of the humeral head.
Diagnosis
Identifying the type of shoulder instability depends on a thorough history and physical examination (Tables 1 and 2). In a patient with acute injury, pertinent historical information includes arm dominance, previous episodes of injury or dislocation and neurologic symptoms. It is important to determine whether reduction occurred spontaneously or required manual manipulation. The position of the arm and the direction of the force when the injury occurred are also important pieces of information.4,11,17
| Type of shoulder instability | History | Findings on physical examination |
|---|---|---|
| Anterior instability | Usually occurs in men in their early 20s Direction of force anterior on arm or posterior on shoulder “Dead arm” syndrome common Often associated with acute injury but can be from overuse, such as in baseball pitchers | Patient presents acutely with arm in abduction and internal rotation, perhaps with palpable anterior mass Axillary nerve injuries can occur Drawer and load-and-shift tests result in anterior displacement and popping Apprehension and relocation tests positive |
| Posterior instability | More commonly associated with seizure or severe electric shock Offensive linemen vulnerable to repetitive subluxation Subluxation occurs when arm is in a foward-flexed, adducted and internally rotated position Posterior shoulder pain with activity | Patient presents with arm externally rotated and a prominent humeral head on the posterior shoulder Missed clinically in 50% of cases Posterior joint line tenderness on palpation Posterior rotator cuff weakness Drawer and load-and-shift tests result in posterior displacement and popping Apprehension and relocation tests negative |
| Multidirectional instability | Most commonly occurs in athletes with congenital hyperlaxity of multiple joints in sports requiring overhead arm motions Usually vague symptoms with activity | Evidence of generalized ligamentous laxity Usually rotator cuff weakness is present Drawer and load-and-shift tests result in anterior and posterior planes of displacement without popping Positive sulcus test is pathognomonic |
| Did your shoulder completely come out of its joint or did your shoulder feel like it was going to slip out of place? |
| How many other times have you had a shoulder injury? |
| When did your present shoulder injury happen? |
| What was the position of your arm when the injury occurred? |
| What was the direction of the force when you were injured? |
| How long was your shoulder out of place before it was put back into place? |
| Did your shoulder go back into place by itself or was it put back into place by someone? |
| What kind of treatment have you had in the past for any shoulder injuries? |
| Did you have numbness or tingling in your arm after you were injured? |
| Do you have unilateral or bilateral problems with your shoulders? |
| Does the shoulder injury affect your dominant or nondominant arm? |
After the shoulder has been put back into place, examination should include assessment of neurovascular integrity, specifically the motor and sensory innervation of the axillary nerve.11 The axillary nerve supplies motor innervation to the deltoid muscle and sensory innervation to the lateral shoulder. Palpation of the bony anatomy and the musculature is important. Rotator cuff strength and range of motion of the injured shoulder should be compared with that of the contralateral shoulder, with documentation of external rotation being the most important evidence for acute dislocation.6
SPECIFIC TESTS
In patients without acute injury, the test that best subjectively quantifies instability is the load-and-shift maneuver. As the patient lies in a supine position with the shoulder relaxed, the examiner places both hands around the patient's upper arm and first the humeral head is “loaded,” or pushed against the glenoid fossa, and then the humeral head is moved (shifted) anteriorly and posteriorly.
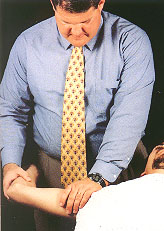
The relocation test is done with the patient in the supine position by abducting and externally rotating the humerus using the edge of the table as a fulcrum (Figure 3). The test is positive for anterior instability if the patient experiences apprehension that is relieved by posterior stress on the shoulder.
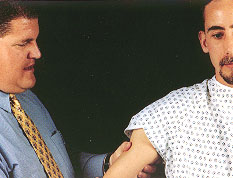
The drawer test is similar to the supine load-and-shift test (Figure 4). In this maneuver, the patient sits while the examiner pushes the humeral head against the glenoid fossa and then moves it anteriorly and posteriorly. Anterior displacement of the joint is a positive response.
The sulcus test is a very important maneuver for evaluating the possibility of multidirectional instability. In this test, the patient sits while the examiner applies caudal traction on the humerus in an attempt to displace the humerus inferiorly (Figure 5). If inferior displacement occurs, the sulcus test is positive, and multidirectional instability is present.

The anterior apprehension test, or crank test, is also used to evaluate shoulder instability. With the patient in a sitting position, the examiner applies abduction and external rotation stress on the joint (Figure 6). The test is positive for anterior instability if the patient experiences apprehension during the test and fears the shoulder is going to slip out of place.

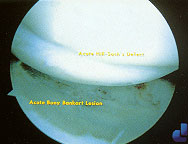
A Bankart lesion may be present if displacement occurs or a pop is appreciated during the anterior apprehension test. The classic Bankart lesion is defined as a tear of the anterior glenoid labrum in association with detachment of the inferior glenohumeral ligament (Figure 7). This type of lesion often occurs with an acute anterior injury, dislocation or severe subluxation.6,11,14
RADIOLOGIC STUDIES
Radiologic studies are helpful in making an accurate diagnosis of shoulder injury. Anteroposterior views with the shoulder in internal and external rotation, an axillary or modified axillary view and the Stryker notch view are standard.4,14 The axillary view is particularly important in ruling out posterior dislocation because it highlights the humeral head position in relation to the glenoid fossa.11,14 The modified axillary view, also called the “West Point” view, is helpful in assessing anterior instability, as it gives an excellent view of the glenoid rim. A fracture of the anterior glenoid is referred to as a bony Bankart lesion. 5,11,14
A Stryker notch view can delineate a Hill-Sachs defect6,11,14 (Figure 8). A Hill-Sachs defect occurs during acute anterior dislocation, when the anterior glenoid rim and the posterolateral humerus contact, creating an osteochondral lesion in the humerus.18 An anteromedial osteochondral lesion, termed the trough sign, can occur with posterior dislocation.14 A Hill-Sachs lesion carries a worse prognosis for anterior instability secondary to the decreased bony support, which is minimal to begin with.6,11,14

Magnetic resonance imaging (MRI), although expensive, may be helpful in the evaluation of chronic subluxation because it provides visualization of all of the shoulder structures. MRI is reported to be 90 to 94 percent accurate in the diagnosis of labral pathology when the MRI findings correlate with the clinical examination.14,19 The use of intra-articular contrast dye during MRI may result in an even higher diagnostic yield. In patients over age 40, accurate radiologic diagnosis of rotator cuff pathology in association with instability is possible only with MRI or arthrography.8
Treatment
Reduction should be accomplished as soon as possible in patients with acute dislocation of the shoulder. A sedating intravenous dose of a narcotic such as meperidine (Demerol) and a benzodiazepine such as midazolam (Versed) is usually required to facilitate the reduction.
Two commonly used techniques for reduction of anterior dislocations are the modified Kocher method and the Stimson method.1,20 The modified Kocher method is performed by placing the patient in the supine position with the body stabilized and applying traction on the humerus while the arm is in an adducted, externally rotated and flexed position (Figure 9). If spontaneous reduction is not accomplished with this technique, the arm is then internally rotated and further adducted. In the Stimson technique, the patient lies in a prone position, and a weight is placed on the dislocated arm (Figure 10). The humerus spontaneously returns to its normal position with the aid of gravity. This may take five to 15 minutes. Posterior dislocations are reduced by applying traction on the arm while it is in an adducted and internally rotated position. If muscle spasm is present or locking is noted with attempted reduction, anesthesia may be required before reduction can be accomplished.20


SURGICAL INTERVENTION
If a Hill-Sachs defect is identified, surgical treatment is recommended because of the decreased bony support of the glenohumeral joint. Many orthopedic surgeons believe surgical repair should also be a consideration in patients under age 25 to prevent further episodes of anterior dislocation and arthritic changes. Early arthroscopic surgery represents a change in the approach, a result of studies that have shown the benefits of arthroscopic repair in reducing the rate of recurrent dislocation. Even in athletes engaged in contact sports, the incidence of recurrent dislocation is only 10 to 20 percent following arthroscopic surgery.10,21,22 Redislocation occurs in some athletes, however, about five years after surgery.23
Open repair for anterior shoulder instability is now used more commonly in patients with recurrent instability or capsular laxity. Although open repair may be more invasive and expensive, the overall recovery time is the same as that associated with arthroscopic repair.6,10,11,22 The rate of recurrent instability is 3 to 7 percent with open repair, compared with 4 to 25 percent following arthroscopic repair, depending on the patient's activity level and the surgeon's experience.6
Posterior and multidirectional instability usually respond to conservative treatment with physical therapy for rehabilitation, unless a specific anatomic lesion is noted.4,16 If patients with posterior or multidirectional instability continue to experience dislocation or subluxation after conservative treatment, referral for possible surgical intervention should be considered.
REHABILITATION
| Phase I |
| Rest and immobilization |
| Pain control with nonsteroidal anti-inflammatory drugs and ice applied to the shoulder |
| Phase II |
| Isometric strengthening |
| Isotonic strengthening |
| Begin exercises with shoulder in adducted, forward-flexed position, progressing to abducted position |
| Phase III |
| Endurance building along with strengthening exercises |
| Goal: the patient reaches 90% strength in the injured shoulder compared with the uninjured shoulder |
| Phase IV |
| Increase activity to sport- or job-specific activities |
Phase II begins with strengthening exercises for the dynamic rotator cuff and the scapular stabilizers (the serratus anterior, pectoralis and latissimus dorsi muscles), initially with isometric exercises and progressing to isotonic exercises. Isometric exercises strengthen a muscle without changing its length, while isotonic exercises allow the resistance to move through the muscle's range of motion.9 About 20 different weight-lifting exercises are useful for strengthening the shoulder muscles. The specific exercises recommended for an individual patient vary, depending on the preference of the physical therapist or athletic trainer and whether the patient is exercising at home or in a weight room. Exercises are started with the shoulder in an adducted, forward-flexed position and progress to abduction in the scapular plane. The adducted, forward-flexed shoulder position minimizes stress placed on the glenohumeral joint.
The last phase consists of progressively increasing the patient's activity to sport- or job-specific activities. The rate at which the patient progresses through each phase of rehabilitation depends on the level of pain and the degree of improvement in strength. It may be helpful to refer the patient to an athletic trainer or physical therapist for one to two visits for instruction in the proper techniques for performing rehabilitation exercises at home.