
A more recent article on evaluating the child with a limp is available.
Am Fam Physician. 2000;61(4):1011-1018
A limp may be defined as any asymmetric deviation from a normal gait pattern. The differential diagnosis of a limp includes trauma, infection, neoplasia and inflammatory, congenital, neuromuscular or developmental disorders. Initially, a broad differential diagnosis should be considered to avoid overlooking less common conditions such as diskitis or psoas abscess. In any patient with a complaint of knee or thigh pain, an underlying hip condition should be considered. The patient's age can further narrow the differential diagnosis, because certain disease entities are age-specific. Vigilance is warranted in conditions requiring emergent treatment such as septic hip. The challenge to the family physician is to identify the cause of the limp and determine if further observation or immediate diagnostic work-up is indicated.
Normal gait follows a predictable pattern and uses energy efficiently. Gait can be divided into swing and stance phases: the swing phase forms 40 percent of the gait cycle, and the stance phase forms 60 percent. The most common form of limp, an antalgic gait, is caused by pain. To minimize weight bearing on an injured limb, the time in stance phase is shortened in the painful limb with a resultant increase in swing phase.
An acute limp implies an underlying pathology that causes disruption of the standard gait pattern; the challenge for the physician is to identify this pathology. The cause of a limp can range from something as serious as a life-threatening bone tumor to something as minor as a pebble in a shoe. The clinician must consider the spine, pelvis and lower extremities for a possible etiology. A useful approach is to consider the causes of limping from head to foot to avoid overlooking common underlying conditions such as diskitis, psoas abscess or septic hip, which are less obvious than conditions involving the lower extremities.
In considering the differential diagnosis of the acutely limping child, the clinician should first consider broader categories of etiologies, such as traumatic, infectious, neoplastic, inflammatory, congenital, neuromuscular or developmental causes (Table 1). Because certain diseases are more common in a given age group, the age of the patient provides critical information to narrow the diagnosis. For example, Legg-Calvé-Perthes disease is rare in toddlers and adolescents but more common in boys four to nine years of age. Table 2 categorizes many etiologies of limping by age.
| Trauma |
| Fracture |
| Stress fracture |
| Toddler's fracture (minimally displaced spiral fracture of the tibia) |
| Soft tissue contusion |
| Ankle sprain |
| Infection |
| Cellulitis |
| Osteomyelitis |
| Septic arthritis |
| Lyme disease |
| Tuberculosis of bone |
| Gonorrhea |
| Postinfectious reactive arthritis |
| Tumor |
| Spinal cord tumors |
| Tumors of bone |
| Benign: osteoid osteoma, osteoblastoma |
| Malignant: osteosarcoma, Ewing's sarcoma |
| Lymphoma |
| Leukemia |
| Inflammatory |
| Juvenile rheumatoid arthritis |
| Transient synovitis |
| Systemic lupus erythematosus |
| Congenital |
| Developmental dysplasia of the hip |
| Sickle cell |
| Congenitally short femur |
| Clubfoot |
| Developmental |
| Legg-Calvé-Perthes disease |
| Slipped capital femoral epiphysis |
| Tarsal coalitions |
| Osteochondritis dissecans (knee, talus) |
| Neurologic |
| Cerebral palsy, especial mild hemiparesis |
| Hereditary sensory motor neuropathies |
| All ages |
| Septic arthritis |
| Osteomyelitis |
| Cellulitis |
| Stress fracture |
| Neoplasm (including leukemia) |
| Neuromuscular |
| Toddler (ages one to three) |
| Septic hip |
| Developmental dysplasia of the hip |
| Occult fractures |
| Leg-length discrepancy |
| Child (ages four to 10) |
| Legg-Calvé-Perthes disease |
| Transient synovitis |
| Juvenile rheumatoid arthritis |
| Adolescent (ages 11 to 16) |
| Slipped capital femoral epiphysis |
| Avascular necrosis of femoral head |
| Overuse syndromes |
| Tarsal coalitions |
| Gonococcal septic arthritis |
History
The child or caretaker should be questioned about the onset and duration of the limp and the association of the limp with pain. It is useful to ask if the limp is getting better, getting worse or staying the same. Usually a child whose limp shows signs of improvement may safely be observed as long as there are no constitutional symptoms. The older patient can localize a painful joint or focal area of pain, which is helpful in narrowing the differential diagnosis; however, referred pain patterns must also be considered (e.g., hip pathology causing knee pain). The very young child can rarely verbalize the location of the discomfort. In younger children, it is useful to ask the caretaker if the child prefers to crawl or walk on his or her knees; a positive response to this question makes foot pathology more likely.
A history of limp that appears worse in the morning suggests a rheumatologic process. Night pain, especially pain that wakes a child from sleep, is a worrisome indicator of a malignant process, and steps should be taken toward rapid diagnosis.
A diagnosis of “growing pains” must meet three criteria: (1) the leg pain is bilateral; (2) the pain occurs only at night; and (3) the patient has no limp, pain or symptoms during the day.1 To inaccurately diagnose a limping child with “growing pains” can be dangerous, as the physician risks missing the underlying pathology. However, if a child does fit the criteria for growing pains, the parents should be reassured that this is a benign, self-limited process that occurs for unknown reasons.
A review of systems should be completed to obtain a history of recent fever or other signs of infection. A recent upper respiratory infection could be the instigating event to a septic process or raise the possibility of poststreptococcal reactive arthritis.2,3 Fever suggests an infection or an inflammatory condition. A family history should also be obtained for rheumatalogic or neuromuscular diseases that may be inherited.
Physical Evaluation
In an antalgic gait, the gait is uneven because less time is spent in the stance phase of the affected leg. If the examiner is uncertain if a limp is present, listening to the sound of the feet hitting the floor may reveal an asymmetric cadence. A child who walks stiffly may be attempting to reduce pain in the spine, such as that occurring in diskitis. In a Trendelenburg gait, the torso shifts over the pathologic limb.4 This gait pattern is commonly seen in older adults with arthritis of the hip, although it also occurs in any condition causing hip inflammation or hip muscle weakness, including Perthes' disease and transient synovitis.
In a young child who clings to a parent and is hesitant to ambulate, the physician can separate the child from the parent and observe the child walking back to the parent. Having the patient run may bring out a gait disturbance not seen with walking.2
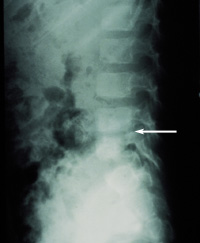
A focused neurologic examination should include observing the child walking on the toes, walking on the heels and hopping on one foot. Inspection of the feet may demonstrate clawing of the toes or cavus foot deformity, which are red flags for an underlying neurologic condition, especially if either condition is unilateral. The patient should be tested for deep tendon reflexes and clonus. The clinician should observe the patient bending forward to identify an asymmetric turning of the spine during flexion, another sign of spinal cord pathology. Limited spinal flexion accompanied by a stiff posture and local tenderness is suggestive of diskitis, which may sometimes be diagnosed with the use of plain radiographs (Figure 1).
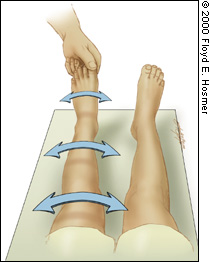
In addition to testing spinal motion in flexion, the standing child should be asked to extend the spine by bending backward. Adolescents with spondylolysis or spondylolisthesis experience an exacerbation of lumbosacral pain with spinal extension. The sacroiliac joint may be involved in infectious or inflammatory conditions. On physical examination, the FABER test (consisting of hip flexion, abduction and external rotation) causes pain in the sacroiliac joint. This test is performed by placing the ipsilateral ankle on the contralateral knee in the supine patient and then providing gentle downward pressure on the knee (Figure 2).

Examination of the hip may be the most important part of the physical examination in a child whose site of pathology is not unequivocally localized, because hip pathology often results in vague pain and many hip conditions require emergent treatment. While infection of the knee or ankle joint may be readily apparent from swelling, tenderness, warmth and erythema, the hip joint is not as easily visualized, and the clinician must rely on indirect assessment on physical examination through range of motion.
Nearly all hip joint pathology causes increased production of fluid within the joint capsule.4 In children with transient synovitis of the hip, the mean intracapsular pressure is only 18 mm Hg when the hip is in 45 degrees of flexion, but it increases to 178 mm Hg when the hip is in extension and internal rotation.5 Clinically, this explains why a child with a septic hip keeps the hip in a position of flexion, abduction and external rotation. Conversely, the position of prone internal rotation is provocative in a child with hip pathology. Every child lacking a clear explanation for a limp should be placed prone, with the knees flexed and the ankles falling away from the body (Figure 3) so the physician can look for a difference in internal rotation between the hips. It is important that the pelvis be kept flat on the table, or the difference in internal rotation between the two sides may not be appreciated.

Hip abduction may also be tested with the hips flexed and extended, again making certain the pelvis remains level. Asymmetry in hip abduction may be indicative of inflammatory conditions of the hip, as well as developmental dysplasia of the hip (Figure 4). The Galeazzi test is performed by putting the child in a supine position and bringing the ankles to the buttocks with the hips and knees flexed. The test is positive when the knees are at different heights, suggesting developmental dysplasia or a leg-length discrepancy (Figure 5). Measurement of thigh and calf circumference should reveal atrophy (more than 1 to 2 cm of difference between sides) in a patient with any hip or knee condition that has limited function for more than one to two months.


To diagnose slipped capital femoral epiphysis, the examiner will observe obligate external rotation of the involved lower extremity when the hip is flexed (Figure 6). These rotational changes can occur when the radiographic findings are still quite minimal. Prompt referral for operative management is warranted.

Differentiating transient synovitis from septic arthritis is particularly challenging, because both conditions present with decreased motion of the hip. A modified log-roll test (Figure 7) may be helpful in differentiating the degree of hip irritation. While distracting the supine child by gently holding the big toe and pretending to examine the foot from different angles, significant hip rotation may be attempted. If an arc of 30 degrees or more of hip rotation is possible without complaints of pain, it has been our experience that a diagnosis of transient synovitis is more likely than one of sepsis.
All joints should be taken through their full range of motion passively and actively and be palpated for tenderness and warmth. Loss of range of motion will help localize the site of pathology. The knee examination should include ballotment of the patella to identify an effusion or hemarthrosis (blood in the joint). Pain at extremes of flexion or extension can signal meniscal pathology; however, in an acute injury, the amount of fluid and pain in the knee joint often makes motion limited, and the examination should be repeated once the fluid has resorbed.
Examination of the ankle should include careful palpation of the fibula physis; often an occult fracture through the growth plate occurs with the same mechanisms of injury that cause ligamentous injuries in the adult.
Laboratory Studies
If, after the history and physical examination, infection is being considered, a complete blood count with differential, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level should be ordered. The platelet count may be low, or the white cell count elevated in the child with leukemia. The CRP becomes elevated earlier than the sedimentation rate and is considered more sensitive for an infectious process. In addition, having a baseline ESR and CRP helps monitor clinical improvement during antibiotic treatment. When examined together, the combination of an ESR greater than 20 and a temperature above 37.5°C (99.5°F) identified septic arthritis of the hip in 97 percent of patients presenting with a limp in one series.6
If the patient lives in an area that is endemic for Lyme disease, blood titers should be determined because acute Lyme disease can mimic a septic process.7
If a septic process is suspected, the first priority should be to aspirate joints with effusion and get a white cell count from the synovial fluid. Gram stain, anaerobic and aerobic cultures, protein and glucose analyses should also be obtained. While there is significant overlap of synovial white cell counts in infection and inflammatory conditions, a white blood cell count above 50,000 per mm3 (50 × 109 per L) should be presumed to be an infection.
A septic joint partially treated with antibiotics may have a lower-than-expected white cell count. A negative culture does not rule out a septic joint; in about 33 percent of cases, the joint aspirate does not recover an organism in a septic joint.8 If the joint in question is the knee in a sexually active patient, the fluid should be cultured for gonorrhea9; this requires a special media (Thayer-Martin) for growth.
Serum rheumatoid factor antinuclear antibody and HLA typing should not be considered initially, because inflammatory diseases in children tend to be seronegative, making blood work less critical than the clinical history and physical examination. Table 3 presents diagnostic criteria for various categories of limp.
| Category | History | Physical examination may show | Laboratory studies | Radiology |
|---|---|---|---|---|
| Traumatic | Fall | Localized pain, swelling, loss of motion | None unless infection is possible | Plain films, bone scan |
| Infectious | Fever, chills, erythema, pain | Rigid guarding, warmth, erythema | CBC, ESR, CRP, joint aspirate | Plain films, MRI, bone scan |
| Neoplastic | Night pain, pain unrelated to activity | Mass | CBC, ESR, CRP, alkaline phosphatase, calcium, electrolytes, joint aspirate | Plain films, MRI/CT, bone scan, staging work-up |
| Congenital | Problem since birth | Deformity, leg-length discrepancy, loss of ROM | None | Plain films |
| Neurologic | Ataxia, loss of balance, disorganized gait | High/low muscle tone, increased/decreased deep tendon reflexes, cavus foot or claw toes | Creatine kinase (if DMD is in differential diagnosis) | Plain films |
| Inflammatory | Pain > 6 months, family history of rheumatoid arthritis | Warmth/erythema, one or more joints | CBC, ESR, CRP, joint aspiration | Plain films |
| Developmental | Painless limp (LCP disease) Knee pain (LCP disease, SCFE) | Loss of ROM in joints, asymmetric ROM, pain with ROM | None | Plain films |
Radiographic Analysis
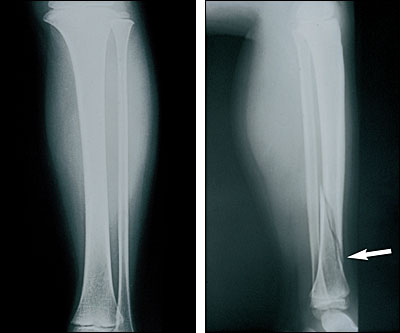
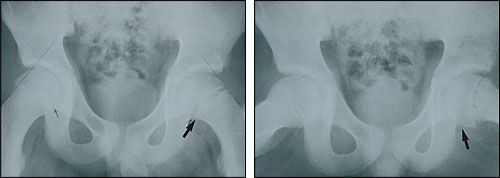
Plain films of the areas in question should be the first radiographic studies ordered.10–12 If an area of pathology is localized by examination or history, anteroposterior and lateral views are indicated because a single view often misses pathology that is obvious in the second view (Figure 8). The pelvic films should be examined for bone fragmentation (Perthes'), joint space widening (sepsis, Perthes') and structural abnormalities (hip dysplasia). Especially in hip films, anteroposterior and frog-lateral views are necessary because the pathology is frequently best seen on lateral views (Figure 9).
In the nonverbal patient, a screening anteroposterior film from hips to feet identifies a fracture in one fifth of patients presenting with a limp.11 It is useful to remember that the growth plate is weaker than the ligamentous attachments to the bone; thus, a ligamentous injury is considerably less common than an occult fracture through the growth plate.
In patients with a history and physical examination consistent with infection of the hip, ultrasonography is useful in identifying fluid in the hip joint.13,14 Ultrasonography is much more sensitive than plain films, identifying an effusion in two thirds of a series of 500 children with normal plain films.14 Ultrasonography is noninvasive but highly dependent on the operator for an accurate result. It is also helpful in identifying fluid in the soft tissues consistent with a soft tissue abscess.13
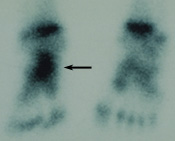
When the cause of a child's limp cannot be localized by history or physical examination, a bone scan is an excellent way to help localize pathology15,16 (Figure 10). A negative bone scan makes an infection, a fracture or most tumors less likely so that observation may be more safely pursued. An area that is bright on bone scan can be further evaluated with plain films, computed tomographic (CT) scan with bone windows or magnetic resonance imaging (MRI) studies. CT best delineates bone structure, whereas MRI best highlights areas of pathology in the soft tissues, as well as inflammation of bone.
Need for Immediate Attention
A delay in diagnosis may be devastating in certain processes that cause a limp. For example, in a septic hip, the increased intra-articular pressure caused by purulence will compromise the blood supply to the femoral head, possibly resulting in catastrophic avascular necrosis unless surgical decompression is performed emergently. In any septic joint process, the body's attempt to eradicate pathogens results in damage to the cartilage surface.
Bone tumors and leukemia are rare but life-threatening, and should be ruled out as quickly as possible as the cause of a limp. Hip pathology is notorious for presenting as knee or thigh pain, and must always be considered in patients with these complaints.
If the child has multiple fractures or a fracture of a suspicious nature, child abuse should be considered.17 Missing this diagnosis and returning a child to an abusive situation can put the child at high risk of mortality.
A frequent dilemma is a limping child with no constitutional symptoms and no localized abnormalities by history or physical examination. We recommend using plain films to rule out a fracture, followed by observation and reevaluation in a few days, depending on the severity of the limp and the family situation. A bone scan should be performed after two to four weeks if symptoms do not resolve or localize.