
Am Fam Physician. 2000;62(1):175-176
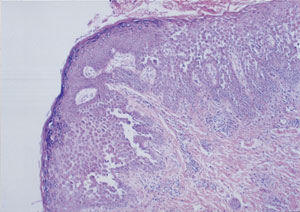
A 90-year-old woman presented with a history of rash under her breasts (Figure 1) and axillae that progressively worsened over a period of two months. She described the eruption as red, irritated, painful and prone to bleeding. No pruritus or scaliness was present. She had tried numerous over-the-counter medications, but none had provided relief. The patient had no rash in any other location and no history of recent antibiotic use, medication changes, new undergarments or exposure to new hygiene products. She denied any associated fevers or chills or recent infection. The biopsy (Figure 2) demonstrated focally impetiginized and inflamed skin with multifocal acantholysis (disrupted connections between keratinocytes in the epidermis). Immunofluorescence studies for immunoglobulins and fibrinogen were negative. The patient responded to a course of oral prednisone, cephalexin (Keflex) and fluconazole (Diflucan).

Question
Discussion
The answer is D: benign familial pemphigus. Chronic benign familial pemphigus, or Hailey-Hailey disease, is a rare autosomal dominant, intraepidermal, nonscarring bullous dermatosis with variable expressivity. About 70 percent of patients report an antecedent family history. The dermatosis was first described by the Hailey brothers in 1939.
Impetigo alone would not generally cause such a prolonged and confluent rash. In addition, there would usually be other areas with bullae or rash associated with autoinoculation.
Intertrigo, which is usually caused by Candida, often occurs in the inframammary folds, and an empiric trial of antifungal treatment would have been a reasonable course of action in this patient. The severe inflammation is less common for intertrigo alone, and a likely incomplete response to antifungal treatment would prompt a search for other diagnostic possibilities.
Contact dermatitis under the breast may be associated with allergens in brassiere materials or topical powders and creams applied to the area. Again, the severity of the rash, its long duration and superinfection make this relatively benign diagnosis less likely.
Histologically, pemphigus vulgaris may appear similar to benign familial pemphigus but generally has more prominent acantholysis and positive immunofluorescence studies.
The basic defect in benign familial pemphigus is a disruption of cellular cohesion resulting in acantholytic damage to the epidermis.1 A number of external stimuli can precipitate acantholysis, including friction, freezing, heat, perspiration, ultraviolet radiation, toxic compounds, allergens and, more importantly, infectious agents (bacteria, yeasts and viruses).
Benign familial pemphigus usually begins in adulthood and is characterized by recurrent blistering lesions with a marked predilection for the intertriginous areas2 (Figure 1). The eruption begins with groups of small, flaccid, pruritic, easily ruptured vesicles. Secondary impetiginization is common. The lesions may become verrucous and usually heal without scarring. Rarely, the oral, esophageal or ocular mucosa may be involved.
The course of Hailey-Hailey disease is characterized by periods of exacerbation and remission. The disease severity and frequency usually decrease with age. Remissions lasting several months to years may occur. The disease has a seasonal pattern with exacerbations in the summer months, mostly because perspiration and friction can precipitate the appearance of the lesions. Malignant degeneration of the lesions, although reported, is rare.
Multiple treatment options are available for Hailey-Hailey disease. Most patients respond to topical corticosteroids and antibacterial creams. However, in severe cases, oral antibiotic therapy should be started. Candida, if present, should be eradicated. Systemic corticosteroids should be reserved for severe cases. Superficial ablation through electrodessication, dermabrasion or laser treatment may be beneficial. Chronic and unresponsive lesions have been treated by surgical excision followed by split-thickness skin grafting.3
The affected areas should be kept as dry and as free of friction as possible. Talcum powder or antiperspirant products that contain aluminum chloride are beneficial, although aluminum chloride products should only be used on intact skin to avoid irritation. Because benign familial pemphigus is autosomally inherited, genetic counseling is recommended.