
Am Fam Physician. 2001;63(5):883-893
Child victims of sexual abuse may present with physical findings that can include anogenital problems, enuresis or encopresis. Behavioral changes may involve sexual acting out, aggression, depression, eating disturbances and regression. Because the examination findings of most child victims of sexual abuse are within normal limits or are nonspecific, the child's statements are extremely important. The child's history as obtained by the physician may be admitted as evidence in court trials; therefore, complete documentation of questions and answers is critical. A careful history should be obtained and a thorough physical examination should be performed with documentation of all findings. When examining the child's genitalia, it is important that the physician be familiar with normal variants, nonspecific changes and diagnostic signs of sexual abuse. Judicious use of laboratory tests, along with appropriate therapy, should be individually tailored. Forensic evidence collection is indicated in certain cases. Referral for psychologic services is important because victims of abuse are more likely to have depression, anxiety disorders, behavioral problems and post-traumatic stress disorder.
It is estimated that by the age of 18, 12 to 25 percent of girls and 8 to 10 percent of boys have been victims of sexual abuse.1 With this high prevalence, it is likely that primary care physicians will encounter child victims of abuse in their practice. Because the diagnosis of sexual abuse often has significant psychologic, social and legal ramifications, evaluating children who allegedly have been sexually abused can be anxiety provoking for physicians, as well as for patients and their families. It is important that the physician be knowledgeable about the basic evaluation of children for sexual abuse and cognizant of the resources available in the community.
Definition
Sexual abuse is defined as any sexual activity that a child cannot comprehend or give consent to, or that violates the law.2 The sexual activity may include fondling, oral-genital, genital and anal contact, as well as exhibitionism, voyeurism and exposure to pornography. Sexual abuse must be differentiated from “sexual play” or age-appropriate behavior. In sexual play, the developmental level of the participants should be similar, and the activity should occur without coercion. For example, preschool children viewing each other's genitalia without force is considered to be “normal,” while a developmentally more mature child engaging a young child in sexual behavior warrants investigation. Perpetrators may be relatives or nonrelatives and are most frequently male.3 Adolescent perpetrators are not uncommon, and many have a personal history of sexual and/or physical abuse.4
Presentation
Concern about possible sexual abuse should be raised when children exhibit behavioral changes or have anogenital or other medical problems. Behavioral changes include sexual acting out, aggression, problems in school, regression (e.g., return to thumb sucking, use of a security blanket), sleep disturbances, depression and eating disturbances. Sexual acting-out behavior is the most specific indicator of possible sexual abuse.5 Medical problems include anogenital trauma, bleeding, irritation or discharge, dysuria, frequent urinary tract infections, encopresis, enuresis (especially after continence has been achieved), pregnancy, diagnosis of a sexually transmitted disease (STD) and oral trauma. Children may present with somatic complaints such as recurrent abdominal pain or frequent headaches resulting from the psychologic stress.
Interviewing the Child
Even in legally confirmed cases of sexual abuse, most children do not have physical findings diagnostic of sexual abuse. Therefore, the child's disclosure is often the most important piece of information in determining the likelihood of abuse. Investigative interviewing should be performed by the appropriate agencies and, if possible, by forensic interviewers. In addition, physicians should ask questions relevant to medical diagnosis and treatment. The child should be interviewed, preferably alone, using open-ended questions such as “Has anyone ever touched you in a way that you didn't like or in a way that made you feel uncomfortable?” It is important to keep a neutral tone of voice and manner when the child responds and to ask the child to elaborate in a nonleading manner. The medical interview may be admissible in court as an exception to hearsay; thus, careful documentation of questions and responses is critical. Questions and answers should be recorded verbatim.6
Physical Examination
The physician should maintain a gentle and calm demeanor and be considerate of the apprehensive child. It is helpful to explain the examination beforehand to the patient and caretaker. A complete physical examination, including careful documentation of any lacerations, ecchymoses or petechiae, is critical. Physical examination of the oral cavity includes inspection of the hard and soft palate for bruising or petechiae, and inspection of the frenulum for any lacerations that can result from forced oral penetration.
If the sexual assault has occurred within 72 hours of the physical examination, forensic evidence collection should be conducted. Rape evidence collection kits are available in the emergency department of most hospitals. Evaluation of acute sexual assault may be conducted in an emergency department setting or, if available, at a children's advocacy center. In nonacute cases, the office of the family physician has the benefit of being a familiar location for the patient.
Magnification and illumination are essential when examining the genitalia. An otoscope or, if available, a colposcope can be used. Demonstration of the instruments before use can be helpful in alleviating a child's fears about the examination. Colposcopy allows enhanced illumination and magnification as well as photographic documentation. If photographic documentation is unavailable, diagrams can be used to illustrate abnormalities.
PHYSICAL EXAMINATION OF PREPUBERTAL AND PUBERTAL GIRLS
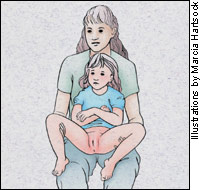
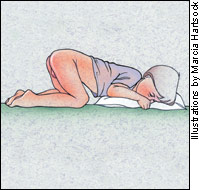
Examination of the genitalia of the prepubertal girl is best performed with the child in the frog-leg, frog-leg while sitting on caretaker's lap or prone knee-chest position (Figures 1a, 1b and 1c). In the frog-leg position, the child is supine with the knees apart. If the child is anxious, the examination may be performed while the child is sitting on the caretaker's lap. In the knee-chest position, the child is prone, with knees, chest and head in contact with the table, and the back is in lordosis. It is necessary to perform an examination in the prone knee-chest position to confirm or exclude abnormalities of the posterior aspect of the hymen.7 Pubertal girls can be examined in the lithotomy position.

Because the examination position can influence findings, it is important to document the position in which the child was examined.8 The use of labial traction can greatly enhance visualization of the hymen. The labia majora are gently retracted between the thumb and forefinger with force applied downward and outward (Figure 2). When performing the anogenital examination, it is important to be familiar with pre-pubertal anatomy and normal variants. The most common hymenal configurations are crescentic, annular, cuff-like, septate (Figures 3a, 3b, 3c and 3d) and fimbriated.
Locations of abnormalities should be described as on a clock face with the urethra in the 12-o'clock position and the anus at the 6-o'clock position. In prepubertal girls, use of the speculum is reserved for unexplained bleeding and may require an examination with sedation. In pubertal girls, estrogen causes the hymenal tissue to become thicker and more compliant; therefore, detection of trauma can be more challenging (Figure 4). The use of a moistened cotton swab to gently move the hymen may be helpful in viewing all aspects of a fimbriated or redundant hymen. Another method of improving visualization of the pubertal hymen requires the use of a Foley catheter. The catheter is inserted into the vagina, the balloon is inflated and, with mild retraction, the hymen is stretched (Figure 5).
PHYSICAL EXAMINATION OF PREPUBERTAL AND PUBERTAL BOYS
A genital examination of boys may be performed with the patient in the sitting, supine or standing position. The physician should examine the penis, testicles and perineum for bite marks, abrasions, bruising or suction ecchymoses. Evaluation of the anus may be performed with the patient in the supine, lateral recumbent or prone position with gentle retraction of the gluteal folds.
Physical Findings
Results of a physical examination will be within normal limits in 80 percent of child victims of sexual abuse.9 The absence of physical findings can be explained by several factors. Many forms of sexual abuse do not cause physical injury. Although the lay public and law enforcement representatives may be fixated on vaginal penetration, sexual abuse may be nonpenetrating contact and may involve fondling, oral-genital, genital or anal contact, as well as genital-genital contact without penetration. Mucosal tissue is elastic and may be stretched without injury, and damage to these mucosal surfaces heals quickly. Finally, many victims of sexual abuse do not seek medical care for weeks or months after the abuse, and superficial abrasions and fissures can heal within 24 to 48 hours.10
Most patients have normal and nonspecific findings on examination. These findings include the following: (1) hymenal tags, bumps or mounds, (2) labial adhesions, (3) clefts or notches in the anterior half (between the 9- and 3-o'clock position) of the hymen, (4) vaginal discharge, (5) erythema of the genitalia or anus, (6) perianal skin tags, (7) anal fissures and (8) anal dilatation with stool in the ampulla. Physical findings that are concerning but not diagnostic of sexual abuse include the following: (1) notches or clefts in the posterior half of the hymen extending nearly to the vaginal floor, confirmed in all positions, (2) condylomata acuminata in a child older than two years who gives no history of sexual contact, (3) immediate, marked anal dilatation and (4) anal scarring.11
Physical findings that are diagnostic of penetrating trauma include: (1) acute laceration or ecchymosis of the hymen, (2) absence of hymenal tissue in the posterior half, (3) healed hymenal transection or complete cleft (Figure 6), (4) deep anal laceration and (5) pregnancy without a history of consensual intercourse (Table 1).1,11
| Normal and nonspecific anogenital findings |
| Hymenal tags |
| Hymenal bumps or mounds |
| Labial adhesions |
| Clefts or notches in the anterior half of the hymen |
| Vaginal discharge |
| Genital or anal erythema |
| Perianal skin tags |
| Anal fissures |
| Anal dilatation with stool in ampulla |
| Physical findings that are concerning for sexual abuse |
| Notches or clefts in the posterior half of the hymen extending nearly to the vaginal floor, confirmed in all positions |
| Condylomata acuminata in a child older than two years who gives no history of sexual contact |
| Immediate, marked anal dilatation |
| Anal scarring |
| Physical findings that are diagnostic of penetrating trauma |
| Acute laceration or ecchymosis of the hymen |
| Absence of hymenal tissue in any portion of the posterior half |
| Healed hymenal transection or complete cleft |
| Deep anal laceration |
| Pregnancy without history of consensual intercourse |
Laboratory
Evidence collection should be performed if sexual contact occurred within 72 hours of the physical examination. Forensic evidence includes blood, semen, sperm, hair or skin fragments that could link the assault to an individual person, as well as debris (e.g., carpet fibers) that could link the assault to a location. Rape evidence collection kits are available and include detailed instructions for the handling of clothes and undergarments, and specimen collection. A history should include obtaining information about the assault, including the use of a condom or lubricants, and whether the victim has eaten, washed, voided, defecated, bathed or douched since the contact. The history should also note if the victim is menstruating or not.
Use of a Wood's lamp may be useful in the detection of semen. Areas that fluoresce should be sampled with a moistened cotton swab, and the specimen sent for laboratory analysis. Although many other substances fluoresce, the collection of semen can be vitally important in a legal case.12 The “chain of custody” ensures that the evidence has remained with the medical staff until given to a representative of a law enforcement agency before arrival of the specimens at the crime laboratory. Because these specimens are used only for forensic evidence, additional specimens are necessary if cultures are to be obtained.
The decision to obtain cultures and to perform serologic testing should be based on the likelihood of oral, genital or anal penetration and the presence of symptoms. Prepubertal females are more likely to be symptomatic if they have Chlamydia or gonorrhea. Pubertal females may be asymptomatic but remain infected. Local prevalence of STDs and risk factors of the child and the alleged perpetrator of abuse should also be taken into consideration. Risk factors for the child or adolescent include other history of sexual contact, multiple sexual partners, intravenous drug use and exchange of sex for food, shelter or money. Risk factors for the alleged perpetrator include a history of multiple sexual partners, intravenous drug use and STDs. Asymptomatic children who disclose only fondling have a very low incidence of STDs.13 The implications of common STDs for the diagnosis of sexual abuse are outlined in Table 2.5
| STD confirmed | Sexual abuse? | Suggested action |
|---|---|---|
| Gonorrhea* | Diagnostic† | Report‡ |
| Syphilis | Diagnostic | Report |
| HIV§ | Diagnostic | Report |
| Chlamydia* | Diagnostic† | Report |
| Trichomonas vaginalis | Highly suspicious | Report |
| Condylomata acuminata* (anogenital warts) | Suspicious | Report |
| Herpes simplex virus (genital location) | Suspicious | Report∥ |
| Bacterial vaginosis | Inconclusive | Medical follow-up |
When testing for Chlamydia and gonorrhea, it is vital that true cultures be obtained. If only nonculture methods (e.g., antigen detection or nucleic acid detection methods) are available, patients must be referred to a location where true cultures can be obtained. Antimicrobial treatment should not be initiated before cultures are obtained. In most states, results of nonculture methods are not admissible in court.14
In cases of acute sexual assault, it is important to remember that performing tests for gonorrhea, Chlamydia, trichomonas and bacterial vaginosis should occur two weeks following the assault if the patient did not receive prophylactic treatment at the time of the initial examination. Serologic testing may be performed for syphilis, human immunodeficiency virus (HIV) infection and hepatitis B (depending on immunization status) at six, 12 and 24 weeks following the assault.15(pp108–16)
Treatment
MEDICAL
Antimicrobial therapy should be initiated in prepubertal children based on the results of laboratory testing. Prophylactic antibiotics for the treatment of gonorrhea, Chlamydia, trichomonas and bacterial vaginosis should be given to sexually active adolescents following an acute sexual assault (Table 3).15(pp49–75) Following acute sexual assault, pregnancy prophylaxis should be offered to adolescent girls after an informed consent has been obtained and urine pregnancy test results are negative. Prophylactic treatment must be started within 72 hours of the assault with two tablets of emergency contraceptive pills (Ovral or Preven) given immediately and two tablets given 12 hours later.16 Because nausea is a common side effect, antiemetics may also be prescribed. Postexposure hepatitis B vaccination (without hepatitis B immunoglobulin) should also be offered at the time of the initial examination if the child has never been immunized. Follow-up doses should be administered one to two and four to six months after the first dose.15(pp108–16)
| Gonorrhea | |
| Ceftriaxone (Rocephin), 125 mg intramuscular in a single dose | |
| or | |
| Cefixime (Suprax), 400 mg orally in a single dose | |
| or | |
| Ciprofloxacin (Cipro), 500 mg orally in a single dose | |
| or | |
| Ofloxacin (Floxin), 400 mg orally in a single dose | |
| and | |
| Chlamydia | |
| Azithromycin (Zithromax), 1 g orally in a single dose | |
| or | |
| Doxycycline (Vibramycin), 100 mg orally twice daily for seven days | |
| and | |
| Bacterial vaginosis and trichomonas | |
| Metronidazole (Flagyl), 2 g orally in a single dose | |
| or | |
| Metronidazole, 500 mg orally twice daily for seven days | |
| or | |
| Clindamycin 2 percent cream (Cleocin), one full applicator (5 g) intravaginally at bedtime for seven days | |
| or | |
| Metronidazole 0.75 percent gel (MetroGel–vaginal), one full applicator (5 g) intravaginally twice daily for five days | |
PSYCHOSOCIAL
The family physician has a unique perspective in the assessment of a child victim of sexual abuse. The ongoing relationship with the parent(s) and the child(ren) may provide the physician with valuable insight regarding the protective nature of one or both parents toward their children. Another issue is the importance of caution when the alleged perpetrator of abuse is a parent or step-parent. The physician must remain unbiased, especially when parental custody disputes are involved.
Care of a child victim of sexual abuse and the family should include a referral for psychologic services. Sexually abused children are at greater risk for depression, anxiety disorders, behavior problems, increased sexual behavior and post-traumatic stress disorder. Adult survivors are also at greater risk for depression, anxiety disorders and interpersonal difficulties. One mediating factor that decreases psychologic distress should be emphasized: the presence of a supportive adult who believes the child's disclosure and takes protective action.17
Child advocacy centers specialize in the evaluation and treatment of sexual abuse victims and the prosecution of sexual abuse perpetrators. Such resources are available in many communities. These centers often include social services, law enforcement agencies, legal services and medical evaluation. The advocacy center can be a resource for services or for a medical consultation. Local advocacy centers can be located by calling the National Children's Alliance at 800-239-9950.
For children with a protective parent and an unrelated perpetrator, child protective services may not be involved. In these cases, law enforcement may be involved; for example, a 2-year-old girl who is raped by a neighbor and the parents have already notified the police. In these instances, it is prudent to refer the family to social services. Social workers can aid the family in locating services. Many victims of sexual abuse are eligible for assistance from the Crime Victim's Compensation Funds, which can be used to reimburse various costs, including psychologic services.
REPORTING GUIDELINES
Physicians are mandated to report suspected cases of child sexual abuse to the local child protective services agency. When sexual abuse is suspected or when a child discloses a sexual abuse event, a report should be made. In most states, the person who reports the suspected abuse case will not be held liable if the report is made in “good faith.” The Guidelines of the American Academy of Pediatrics for reporting abuse based on the history and physical examination are presented in Table 4.5
Final Comment
By working with law enforcement and social service agencies, the family physician can play an integral role in establishing a protective environment for the child victim of sexual abuse to begin the healing process. Child sexual abuse is a complex problem that requires the family physician to evaluate and treat the patient using a multidisciplinary approach. It is important to be comfortable in the initial evaluation of the child and to be aware of the many resources and agencies available within the community. A thorough history and physical examination by a trusted family physician can help alleviate anxiety for the child and the family.