
Am Fam Physician. 2001;63(12):2391-2398
A more recent article on benign anorectal conditions is available.
Anorectal symptoms and complaints are common and may be caused by a wide spectrum of conditions. Although most conditions are benign and may be successfully treated by primary care practitioners, a high index of suspicion for colorectal cancer should be maintained, and all patients should be appropriately investigated. Inspection, palpation and anoscopic examination using an Ive's slotted anoscope provide adequate initial assessment. Pruritus ani usually represents a self-perpetuating itch-scratch cycle and is uncommonly due to infection. The history, as well as the physical examination, can distinguish anal pain due to hemorrhoids, fissure, abscess, cancer or proctalgia fugax. The most frequent causes of rectal bleeding are hemorrhoids, fissures and polyps. Diagnoses associated with difficulty in passing stool can range from constipation to fecal incontinence.
Patients frequently consult primary care physicians because of concerns about or symptoms related to the anorectal area. Although many anorectal conditions are benign and easily treated, patients may delay seeking medical advice because of embarrassment or fear of cancer. Thus, both malignant and nonmalignant conditions often present as advanced disease, requiring more extensive treatment and causing greater patient distress than if conditions had been adequately diagnosed and managed at an earlier stage.
Conversely, both patients and physicians should be aware of the need for adequate assessment of all anorectal symptoms because of the high incidence of colorectal cancer. The average American is estimated to have a one in 18 lifetime risk of developing colorectal cancer.1 This risk is equal for men and women and increases with age. In 2001, an estimated 138,000 new cases of cancer of the colon, rectum or anus will be diagnosed; these cancers will cause the death of more than 57,200 adults each year in the United States.1 In nonsmokers, colorectal cancer is the leading cause of death from cancer.
Colorectal cancer may present as rectal bleeding and coexist with a benign condition such as hemorrhoids. Every patient with anorectal symptoms, especially those with rectal bleeding, must have an assessment that includes, at a minimum, digital rectal examination and visual inspection by anoscope. Increasing access to primary care physicians leads to earlier detection of colorectal cancer.2
Current American Academy of Family Physicians (AAFP) and American Cancer Society (ACS) guidelines call for screening of all patients for colorectal cancer beginning at 50 years of age in the general population and 40 years of age in those with risk factors or a family history of the disease.3 Family physicians can play a major role in the prompt recognition of cancer and appropriate management of other anorectal conditions. All clinicians can and must perform a basic examination to appropriately treat or refer patients with anorectal complaints. After proper evaluation, the majority of nonmalignant anorectal conditions can be treated by the primary caregiver.
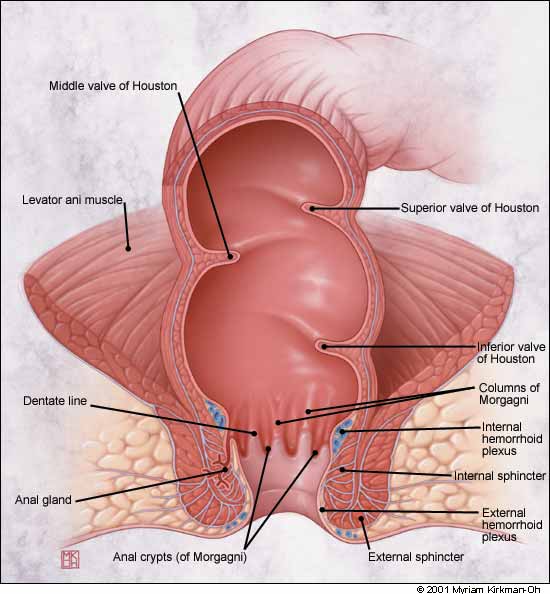
Anal/Rectal Anatomy
The anus is the outlet to the gastrointestinal tract, and the rectum is the lower 10 to 15 cm of the large intestine (Figure 1). The valves of Houston are not true valves but are prominent mucosal folds. The dentate or pectinate line divides the squamous epithelium from the mucosal or columnar epithelium. Four to eight anal glands drain into the crypts of Morgagni at the level of the dentate line. Most rectal abscesses and fistulae originate in these glands. The dentate line also delineates where sensory fibers end. Above (proximal to) the dentate line, the rectum is supplied by stretch nerve fibers but not pain nerve fibers. This allows many surgical procedures to be performed without anesthesia above the dentate line. Conversely, below the dentate line there is extreme sensitivity, and the perianal area is one of the more sensitive areas of the body. The evacuation of bowel contents depends on action by the muscles of both the involuntary internal sphincter and the voluntary external sphincter.
Anorectal Examination
Anorectal assessment consists of inspection, palpation and anoscopic examination. The patient can be positioned in the left lateral decubitus position for this examination and for almost all anorectal procedures. This position is much more comfortable for the patient than the traditional head-down “jackknife” position, yet still allows adequate visualization and access for the examiner.
The glutei must be spread to provide adequate visualization of the anus. If necessary, the patient can assist by raising the right gluteal area with the right hand to better expose the perianal area. Inspection alone can reveal fissures, fistulae, perianal dermatitis, masses, thrombosed hemorrhoids, condyloma and other growths.
Unless the patient is experiencing extreme pain, a digital examination should always be performed. In males, the prostate should be palpated in addition to digital assessment of the anal canal. The finger sweep must include all 360 degrees around the anal canal, and any palpable mass must be defined. Because of the redundant mucosa, small tumors may not be visualized even with the anoscope but can often be detected by palpation.
The final step in the initial office examination is usually anoscopy. Although many types of anoscope are available, the best visualization is provided by the Ive's slotted anoscope (Figure 2). A lubricant is applied to the entire unit, and it is inserted gently. The introducer is removed and one quarter of the mucosa is visualized as the anoscope is slowly removed. The instrument is then rotated 90 degrees and reinserted. This is done four times to visualize the entire circumference of the anal canal. The currently available plastic anoscopes are smaller and do not provide the view of the larger Ive's scope. Although preparation with an enema is not usually necessary before anoscopy, it can improve visualization and may be aesthetically more acceptable to the examiner and to the patient.
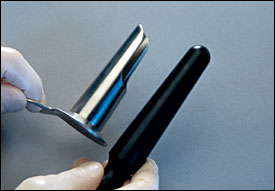
Further examination using flexible sigmoidoscopy and/or colonoscopy may be indicated in individual patients. Even if endoscopic examination includes retroflexion of the scope to inspect the anal canal, optimal visualization is obtained with the Ive's slotted anoscope.
Common Anorectal Symptoms
PRURITUS ANI
Pruritus ani is an extremely common symptom and is associated with a wide range of mechanical, dermatologic, infectious, systemic and other conditions (Table 1). Regardless of the etiology, the itch/scratch cycle becomes self-propagating and results in chronic pathologic changes that persist even if the initiating factor is removed.
| Systemic illness |
| Diabetes mellitus |
| Hyperbilirubinemia |
| Leukemia |
| Aplastic anemia |
| Thyroid disease |
| Mechanical factors |
| Chronic diarrhea |
| Chronic constipation |
| Anal incontinence |
| Soaps, deodorants, perfumes |
| Over-vigorous cleansing |
| Hemorrhoids producing leakage |
| Prolapsed hemorrhoids |
| Alcohol-based anal wipes |
| Rectal prolapse |
| Anal papilloma |
| Anal fissure |
| Anal fistula |
| Tight-fitting clothes |
| Allergy to dyes in toilet paper |
| Intolerance to fabric softener |
| Skin sensitivity from foods |
| Tomatoes |
| Caffeinated beverages |
| Beer |
| Citrus products |
| Milk products |
| Dermatologi conditions |
| Psoriasis |
| Seborrheic dermatitis |
| Intertrigo |
| Neurodermatitis |
| Bowen's disease |
| Various squamous disorders |
| Atopic dermatitis |
| Lichen planus |
| Lichen sclerosis |
| Contact dermatitis |
| Infections |
| Erythrasma (Corynebacterium) |
| Intertrigo (Candida) |
| Herpes simplex virus |
| Human papillomavirus |
| Pinworms (Enterobius) |
| Scabies |
| Local bacterial abscess |
| Gonorrhea |
| Syphilis |
| Medications |
| Colchicine |
| Quinidine |
When pruritus ani becomes chronic, the perianal area becomes lichenified and appears white with fine fissures (Figure 3). Although older texts emphasized parasitic infestation, this is a rare cause of pruritus ani except for pinworms (Enterobius vermicularis) in children. Many patients believe pruritus ani is caused by poor hygiene and are overzealous in their attempts to clean the perianal area. Excessive cleaning, and particularly the use of brushes and caustic soaps, aggravates the sensitive tissues and exacerbates the condition. Many patients have an underlying eczematoid-type skin. The perianal area can be highly sensitive to perfumes, soaps, clothes, fabrics, dietary intake and superficial trauma.

Successful treatment of pruritus ani depends on recognizing the condition, ruling out other potential diagnoses, addressing precipitating or exacerbating conditions and relieving the itch/scratch cycle. Many patients scratch excessively during sleep and are unaware of their actions. An antihistamine such as hydroxyzine hydrochloride (Atarax) taken before bedtime is often quite helpful because it provides both antipruritic and sedative effects. Topical corticosteroids are usually necessary to control pruritus ani but must be limited to short-term use to avoid thinning of the perianal tissues. This, in itself, can lead to more pruritus. Topical 5 percent xylocaine ointment (Lidocaine) can also reduce the itching sensation and break the cycle. It should be noted that uncomplicated hemorrhoids rarely cause pruritus ani. Only hemorrhoidal tags that are inflamed or associated with poor hygiene may produce pruritus. Any pruritic lesion that persists after adequate treatment should be biopsied.
ANAL PAIN
A careful history focusing on the nature of the pain and its relationship to bowel movements frequently provides the diagnosis of pain in the anorectal area. Aching after a bowel movement can occur with internal hemorrhoids. Pain during bowel movements that is described as “being cut with sharp glass” usually indicates a fissure. This pain is most intense during the bowel movement and usually persists for an hour or so afterward. It may then either abate until the next bowel movement or continue, usually to a lesser degree. The pain of anal fissure is frequently accompanied by bright red rectal bleeding and often begins after a hard, forced bowel movement.
The acute onset of pain with a palpable mass is almost always due to a thrombosed external hemorrhoid (Figure 4). This intense pain typically lasts 48 to 72 hours and then subsides spontaneously but may take several days to abate. Internal hemorrhoids, because they start above the dentate line, are not painful even if prolapsed or thrombosed. Similarly, rectal cancer seldom causes pain unless it is extremely advanced because of the innervation of the rectal area. Anal cancers more commonly cause pain after invasion of the sphincter muscle. Anorectal pain that begins gradually and becomes excruciating over a few days may indicate infection. A localized area of tenderness could signal an abscess. Anal pain accompanied by fever and inability to pass urine signals perineal sepsis and is a medical emergency.

Proctalgia fugax is a unique anal pain. Patients with proctalgia fugax experience severe episodes of spasm-like pain that often occur at night. Proctalgia fugax may only occur once a year or may be experienced in waves of three or four times per week. Each episode lasts only minutes, but the pain is excruciating and may be accompanied by sweating, pallor and tachycardia. Patients experience urgency to defecate, yet pass no stool.
No specific etiology has been found, but proctalgia fugax may be associated with spastic contractions of the rectum or the muscular pelvic floor in irritable bowel syndrome. Other unproven associations are food allergies, especially to artificial sweeteners or caffeine. Reassurance that the condition is benign may be helpful, but little can be done to treat proctalgia fugax. Medications are not helpful since the episode is likely to be over before the drugs become active. Sitting in a tub of hot water or, alternatively, applying ice may provide symptomatic relief. A low dose of diazepam (Valium) at bedtime may be beneficial in cases of frequent and disabling proctalgia fugax.
LUMP'/PALPABLE MASS
When a palpable mass is discovered in the anal area, the patient may be concerned about cancer or assume the mass is a hemorrhoid. Anal or perineal “lumps” may be due to a wide range of conditions including condyloma, molluscum contagiosum, hemorrhoids (thrombosed, tags or prolapsed), polyps, sentinel tags related to fissure, or cancer. Full assessment, including a detailed history, inspection, palpation, anoscopy and, in some cases, biopsy, sigmoidoscopy or colonoscopy, is needed to define the exact nature of these lesions. Rectal masses will be further discussed in part II of this article.
RECTAL BLEEDING
Many conditions can cause rectal bleeding (Table 2), but all cases of rectal bleeding must be evaluated and the cause identified. Even the occasional finding of blood on toilet paper after a bowel movement (“wipe hematochezia”) must be taken seriously.4 Significant pathologic conditions such as cancers and polyps can bleed intermittently. A study of patients presenting to family physicians5 found the most common causes of rectal bleeding to be hemorrhoids, fissures and polyps (Table 3). The authors of that study concluded that if one of these common conditions were identified as the probable site and cause of bleeding, colonoscopy and other investigations were not usually necessary. Indications for further investigation include older age, significant family history of bowel disease or cancer, and nonresolution of the bleeding after treatment of the condition that is presumed to be the source of bleeding. Total colon examination is mandated if rectal bleeding is accompanied by systemic symptoms, if there is a clinical suspicion of proximal disease and when the cause of rectal bleeding cannot be readily established.
| Bright red rectal bleeding | Occult blood |
|---|---|
| Hemorrhoids | Gastritis |
| Diverticula | Gastric ulcer |
| Regional enteritis | Gastric carcinoma |
| Ulcerative colitis | Esophageal varices |
| Infectious colitis (entero-hemorrhagic) | Arteriovenous malformation |
| Carcinoma | Esophageal tumor |
| Polyps | Esophagitis |
| Arteriovenous malformation | Hiatal hernia |
| Intussusception | Duodenal ulcer |
| Fistula | Duodenitis |
| Fissure | Polyps |
| Chronic solitary ulcer | Carcinoma |
| Diverticula |
| Hemorrhoids | Colorectal cancer |
| Fissures | Ulcerative proctocolitis |
| Polyps | Gastritis |
| Proctitis | Diverticula disease |
| Peptic ulcer | Systemic disease |
| Anorectal Conditions |
DIFFICULTY PASSING STOOL
The term constipation can have a variety of meanings. Patients may use the term to indicate the lack of an urge to defecate, a decreased frequency of bowel movements, difficulty in passing hard scybalous stools, the sensation of incomplete evacuation or prolonged straining at toilet. In general, constipation is regarded as fewer than three bowel movements per week in a person consuming at least 19 g of fiber daily. This condition can be due to diet, medications, functional disturbances, endocrine and metabolic disorders, collagen vascular disease, central or peripheral neuromuscular disorders or colonic inertia. It is imperative that the clinician rule out obstructing lesions or painful anal lesions.6
FECAL IMPACTION
Fecal impaction can present with either constipation or fecal incontinence (“overflow”). It is common in bedridden or nursing home patients or after a cerebral vascular accident and is the most common gastrointestinal disorder occurring in patients with a spinal cord injury. Medications such as narcotics predispose to this problem, and it is a common complication of anorectal procedures as a result of reflex spasm of the anal sphincter. The patient may present with acute abdominal pain or chronic large-bowel obstruction. Rectal examination reveals hard, bulky stool. Medical therapy is usually attempted first in an otherwise ambulatory patient. Careful administration of one or two enemas (Fleet) into the bolus to soften and hydrate the stool should be followed one hour afterward by the administration of a mineral oil enema to assist in passage of the softened stool.
Manual disimpaction is required in most patients. This may require a circumanal block of the anal musculature with local anesthetic. A four-quadrant field block allows for complete muscle relaxation and a painless disimpaction. After disimpaction, a bowel program that includes the use of a laxative, stool softeners and/or enemas should be initiated to prevent recurrence. If impaction recurs, it is important to rule out an anatomic cause of obstruction such as an anal or rectal stricture or tumor.
FECAL INCONTINENCE
Fecal incontinence is the inadvertent passage of flatus, liquid or solid stool. Normal continence depends on many interrelated factors, including stool volume and consistency, colonic function, rectal compliance, rectal sensation and sphincter function. Patients may be partially or completely incontinent. It is important to rule out fecal impaction with overflow before seeking a pathophysiologic cause for uncontrolled passage of liquid stool. Patients at risk for fecal incontinence include the elderly, mentally ill and parous women, particularly those with a history of sphincter damage during delivery.
Fecal incontinence with significant decrease in sphincter tone can be caused by any prior anorectal operative procedure or birthing injury. Obstetric injury can include direct sphincter disruption (usually anterior) or injury to the pudendal nerves. Not uncommonly, these may occur simultaneously. Neuropathy, particularly that associated with diabetes mellitus, can result in fecal incontinence. Other causes include rectal prolapse, diarrheal states, radiation injury to the rectum and overflow fecal incontinence secondary to impaction.
Digital examination of the patient with fecal incontinence includes palpation for muscle defects of the sphincter, assessment of resting and squeeze pressures of the sphincter, and testing of the sensory anocutaneous reflex. Stroking the skin of the anal area, usually with the end of a paper clip, should cause a contraction (“wink”) of the anal musculature. In selected cases, additional studies may include anal manometry to objectively measure sphincter pressures, endo-anal ultrasonography to morphologically visualize the sphincter searching for discrete defects, and electromyelographic or pudendal nerve terminal motor latencies to assess denervation injury.7
Fecal incontinence can seriously impair or restrict normal activities and complicate the care of already frail patients. Treatment is generally directed at the underlying cause and minimizing symptoms. Discrete muscle injuries are usually best treated by surgical sphincter repair. Fecal incontinence secondary to neuropathy is treated with bulking and antimotility agents. Pelvic floor strengthening with biofeedback is also a useful modality.