
Am Fam Physician. 2003;67(9):1979-1980
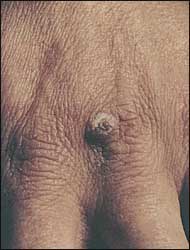
A 41-year-old welder presented with right-hand skin lesions thought to be welding burns that had become infected. He was scheduled to have neck surgery for an unrelated problem, but when the surgeon saw the lesions, surgery was canceled, and he was given levofloxacin. He later visited his primary care physician who gave him an injection of ceftriaxone and another prescription for levofloxacin. He was diagnosed as having cellulitis of the right hand. When the patient presented to an occupational health clinic three days later, the wounds had ulcerated and had increased in size dramatically. He was complaining of severe pain in the hand but no itching. On the dorsum of his right hand, he had three large, ulcerated, plum-colored plaques with central ulceration. Surrounding the plaque borders was a narrow band of erythema (Figure 1). The physical examination was normal otherwise except for a hyperkeratotic papule on the dorsum of the left hand, which also was thought to be caused by a hot solder burn. The patient noted that this papule looked like the lesions on the right hand before they began to ulcerate (Figure 2). A complete blood count was performed revealing a normal white cell count of 7,000 per mm3 with a normal differential. A punch biopsy of the lesion was performed and sent for pathology.

Question
Discussion
The answer is C: systemic steroids. The punch biopsy was reported back two weeks later as neutrophilic dermatosis, the skin finding associated with Sweet's syndrome. Special stains for infectious organisms were negative.
The patient responded rapidly to an injection of betamethasone. The pain was gone in 24 hours. The raised borders of the lesions that originally mimicked a deep burn ulcer resolved in the first three days after treatment (Figure 3). By 10 days, the wounds were almost re-epithelialized.

Intravenous antibiotics would not be effective in this case, nor would the topical anti-impetigo drug mupirocin. The patient had already finished two courses of levofloxacin and received an injection of ceftriaxone. A wound culture after antibiotic treatment would only show colonizing bacteria and complicate the picture. Gram stain of any wound exudate might have been helpful, but there was no exudate in this case. Cellulitis also is a less likely etiology given the multiple discrete lesions on one hand and the distant lesion on the other hand.
Excision with skin grafting or debridement has been known to exacerbate the skin lesions in Sweet's syndrome.
Observation might be an appropriate answer; however, these lesions were rapidly growing and painful to the patient, and if left untreated they could increase up to 20 cm in size. It is not likely that a single injection of betamethasone would have made anything worse if the suspected neutrophilic dermatosis was not confirmed by pathology.
Sweet's syndrome was first described in 1964.1 It is characterized by painful erythematous pustular-appearing plaques, usually on the face and upper body, accompanied by fever, leukocytosis, and arthralgias. Several subsets have been described, including paraneoplastic, pregnancy-related,2 and localized neutrophilic dermatosis,3 where fever and other systemic signs are not present. The etiology of neutrophilic dermatosis is unknown. Hypothesized mechanisms include infection, altered neutrophil function, and an auto-immune mechanism. Convincing evidence for any one of these mechanisms has not been forthcoming.2
The typical lesions of neutrophilic dermatosis are painful purplish raised plaques. The lesions are firm, and on biopsy, no fluid or exudate is present. Treatment with antibiotics seldom is helpful unless secondary infection is present. Prompt relief of cutaneous and systemic symptoms is rapidly achieved with systemic steroids.2 Even with no treatment, many lesions may heal with time.
It often is speculated that widespread lesions, especially when accompanied by fever and other systemic manifestations, may herald the onset or recurrence of a malignancy. When faced with a wound that does not heal as expected, and especially if there are multiple lesions rapidly increasing in size without response to antibiotics, remember to include Sweet's syndrome in the differential diagnosis. Once having seen a typical lesion, it is much easier to make the diagnosis in the future.