
A more recent article on vertebral compression fractures is available.
Am Fam Physician. 2004;69(1):111-116
Compression fracture of the vertebral body is common, especially in older adults. Vertebral compression fractures usually are caused by osteoporosis, and range from mild to severe. More severe fractures can cause significant pain, leading to inability to perform activities of daily living, and life-threatening decline in the elderly patient who already has decreased reserves. While the diagnosis can be suspected from history and physical examination, plain roentgenography, as well as occasional computed tomography or magnetic resonance imaging, are often helpful in accurate diagnosis and prognosis. Traditional conservative treatment includes bed rest, pain control, and physical therapy. Interventional procedures such as vertebroplasty can be considered in those patients who do not respond to initial treatment. Family physicians can help patients prevent compression fractures by diagnosing and treating predisposing factors, identifying high-risk patients, and educating patients and the public about measures to prevent falls.
Vertebral compression fractures affect approximately 25 percent of all postmenopausal women in the United States.1 The prevalence of this condition steadily increases with advancing age, reaching 40 percent in women 80 years of age.2 Women diagnosed with a compression fracture of the vertebra have a 15 percent higher mortality rate than those who do not experience fractures.3 Although less common in older men, compression fractures also are a major health concern in this group.4–6 Because the age group of those older than 65 years is now the fastest growing segment of the U.S. population, the incidence of this age-specific fracture is likely to increase.
According to data collected in 1995, the annual direct medical cost of vertebral compression fractures in the United States is estimated to be $746 million.1 Vertebral compression fractures are less expensive compared with hip fractures; however, vertebral compression fractures have a substantial negative impact on the patient's function and quality of life.7 Acute and chronic pain in the elderly commonly is attributed to severe pain from vertebral compression fractures, and often leads to further disability.8
In addition to physical limitations, vertebral compression fractures may produce a psychosocial and emotional burden on the aging person who already faces losses of independent function. This may cause the person to worry about what the future may bring. These worries are not unfounded, because there is a substantial risk of subsequent fractures of all types and further morbidity in persons who have had a vertebral compression fracture.9
Pathophysiology and Risk Factors
Vertebral compression fractures are recognized as the hallmark of osteoporosis,10 and many of the risk factors are the same.11 Risk factors are categorized as those not modifiable and those that are potentially modifiable. Nonmodifiable risk factors include advanced age, female gender, Caucasian race, presence of dementia, susceptibility to falling, history of fractures in adulthood, and history of fractures in a first-degree relative.
Potentially modifiable risk factors include being in an abusive situation, alcohol and/or tobacco use, presence of osteoporosis and/or estrogen deficiency, early menopause or bilateral ovariectomy, premenopausal amenorrhea for more than one year, frailty, impaired eyesight, insufficient physical activity, low body weight, and dietary calcium and/or vitamin D deficiency.
Fracture rates are lower in most nonwhite populations, but vertebral compression fractures are as common in Asian women as in white women. Ironically, obesity is protective to fractures as it is to bone loss in general.
Acute fractures occur when the weight of the upper body exceeds the ability of the bone within the vertebral body to support the load. Generally, some trauma occurs with each compression fracture. In cases of severe osteoporosis, however, the cause of trauma may be simple, such as stepping out of a bathtub, vigorous sneezing, or lifting a trivial object, or the trauma may result from the load caused by muscle contraction.12(p 880–1) Up to 30 percent of compression fractures occur while the patient is in bed.13 In cases of moderate osteoporosis, more force or trauma is required to create a fracture, such as falling off a chair, tripping, or attempting to lift a heavy object. Of course, a healthy spine can sustain a compression fracture from severe trauma such as an automobile crash or a hard fall.
The applied force usually causes the anterior part of the vertebral body to crush, forming an anterior wedge fracture (Figure 1). The middle column remains intact and may act as a hinge. This results in loss of anterior height of the vertebra while the posterior height remains unchanged. As the collapsed anterior vertebrae fuse together, the spine bends forward, causing a kyphotic deformity. Because the majority of damage is limited to the anterior vertebral column, the fracture is usually stable and rarely associated with neurologic compromise.14 A fracture is considered a “burst fracture” if the entire vertebral body breaks (Figure 2).
Spinal compression fractures can be insidious and may produce only modest back pain early in the course of progressive disease. Over time, multiple fractures may result in significant loss of height. Progressive loss of stature results in shortening of paraspinal musculature requiring prolonged active contraction for maintenance of posture, resulting in pain from muscle fatigue. This pain may continue long after the acute fracture has healed.15
Patients develop thoracic kyphosis and lumbar lordosis as vertebral height is lost. The rib cage presses down on the pelvis, reducing thoracic and abdominal space. In severe cases, this results in impaired pulmonary function, a protuberant abdomen, and—because of compressed abdominal organs—early satiety and weight loss.16 Complications from compression fractures are summarized in Table 1.
Diagnosis
About one third of vertebral fractures are actually diagnosed,17,18 because many patients and families regard back pain symptoms as “arthritis” or a normal part of aging. Therefore, compression fracture should be suspected in any patient older than 50 years with acute onset of sudden low back pain. Most patients will remember a specific injury as the cause10; however, fractures may occur without any history of increased force on the spine. Lying in the supine position generally relieves some of the discomfort. Standing or walking exacerbates the pain.
Physical examination will reveal tenderness directly over the area of acute fracture, and an increased kyphosis may be noted.19 In cases of uncomplicated compression fractures, straight leg raise will be negative and neurologic examination will be normal. An ileus, or decreased bowel sounds, may be present. The diagnosis can be confirmed if plain radiographs show the classic wedge deformity correlating with the area of tenderness found on physical examination.
Radiographic Findings
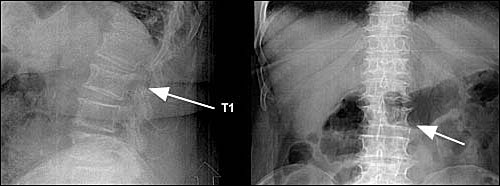
Radiographically, a decrease in vertebral height of 20 percent or more, or a decrease of at least 4 mm compared with baseline height is considered positive for compression fracture.10
Compression fractures can occur anywhere from the occiput to the sacrum, although they usually occur at the lumbodorsal junction, namely T8-T12, L1, and L4.13 It is important to image the entire spine because 20 to 30 percent of vertebral compression fractures are multiple. When multiple, the fractures occur at different levels or in one to five consecutive vertebral bodies.12(p 250–1) Serial plain films may be necessary to visualize the vertebral injury because the deformity can take days to weeks to develop.
| Constipation Bowel obstruction Prolonged inactivity Deep venous thrombosis Increased osteoporosis Progressive muscle weakness Loss of independence Kyphosis and loss of height | Crowding of internal organs Respiratory decrease-atelectasis, pneumonia Prolonged pain Low self-esteem Emotional and social problems Increased nursing home admissions Mortality |
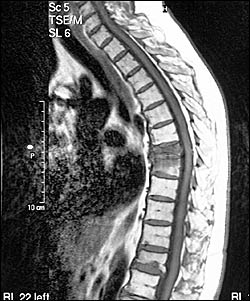
Computed tomography (CT) and magnetic resonance imaging (MRI) are used for evaluating the posterior vertebral wall integrity and for ruling out other causes of back pain (Figure 4).21 CT can be helpful for identifying a fracture that is not well visualized on plain films, for distinguishing a compression fracture from a burst fracture, and for further evaluation of a complex fracture. CT also can reveal spinal canal narrowing. MRI is recommended when patients have suspected spinal cord compression or other neurologic symptoms.
Malignancy, not osteoporosis, should be considered as the cause in patients younger than 55 years with a compression fracture without trauma or only minimal trauma.19 In these patients, or in patients with known or suspected malignancy, MRI should be obtained as part of the work-up. The “fluid-sign” (presence of a fat-fluid level, or lipohemarthrosis) on MRI can be useful to distinguish osteoporosis from malignancy as the cause for pathologic fracture.22 MRI also allows for the differentiation of edema caused by a benign fracture from that of tumor infiltration.
The bone marrow signal on MRI can help identify an acute fracture and distinguish ages of compression fractures.23 Follow-up films or further evaluation with CT or MRI is indicated for patients with continued pain despite conservative therapy or when symptoms are progressive. Bone density studies are beneficial for evaluating the severity of osteoporosis and in advising patients of the likelihood of subsequent fractures.24
A nuclear medicine bone scan (Figure 5) is useful when surveying the entire skeleton for osteoporotic fractures, especially when symptoms are atypical. It is particularly helpful in diagnosing sacral insufficiency fractures, which are common in osteoporosis but difficult to visualize on radiographs. On bone scan, they appear as increased radiotracer activity in an “H” or “butterfly” pattern across the sacrum. Bone scans also can differentiate between an acute versus healed compression fracture because new fractures will appear “hot.”
Treatment
The physician must first determine if the fracture is stable or unstable. A stable fracture will not be displaced by physiologic forces or movement. Fortunately, compression fractures are normally stable secondary to their impacted nature. Traditional treatment is nonoperative and conservative. Patients are treated with a short period (no more than a few days) of bedrest. Prolonged inactivity should be avoided, especially in elderly patients. Oral or parenteral analgesics may be administered for pain control, with careful observation of bowel motility. If bowel sounds and flatus are not present, the patient may require evaluation and treatment for ileus. Calcitonin-salmon (Miacalcin) nasal spray can be used for treatment of pain.25 Muscle relaxants, external back-braces, and physical therapy modalities also may help.26 [Evidence level B] Nonsteroidal anti-inflammatory drugs have been shown to significantly increase gastrointestinal bleeding in the elderly and must be used with caution.27 [Evidence level A, randomized control trial (RCT)]

Patients who do not respond to conservative treatment or who continue to have severe pain may be candidates for percutaneous vertebroplasty. Percutaneous vertebroplasty involves injecting acrylic cement into the collapsed vertebra to stabilize and strengthen the fracture and vertebral body.21 This procedure does not, however, restore the shape or height of the compressed vertebra. Kyphoplasty, where cement is injected into a cavity created by a high-pressure balloon, is being evaluated for use and may be successful in restoring height to the collapsed vertebra.
Most patients can make a full recovery or at least significant improvements from their compression fracture after six to 12 weeks, and can return to a normal exercise program after the fracture has fully healed. A well-balanced diet, regular exercise program, calcium and vitamin D supplements,28 smoking cessation, and medications to treat osteoporosis (such as bisphosphonates) may help prevent additional compression fractures. Age should never preclude treatment.
There is now good evidence that diagnosing and treating osteoporosis does indeed reduce the incidence of compression fractures of the spine.24,29,30 [Reference 29—Evidence level A, RCT; Reference 30—Evidence level A, RCT] Regular activity and muscle strengthening exercises have been shown to decrease vertebral fractures and back pain.31 Measures to prevent falls must be initiated by patients and their caregivers. Table 232 lists items that should be assessed when determining what preventive measures should be followed.
Additionally, family physicians can take a leadership role in their communities by assessing and addressing those factors that can increase the incidence of vertebral compression fractures in elderly persons, such as inappropriate or over-medication, use of restraints, unsafe home situations, and physical abuse.
| Avoidance of restraints Balance assessment Cardiac function, cardiac rhythm heart rate, orthostatic pulse, and blood pressure Gait | Muscle strength Neurologic function; cortical, extrapyramidal, and cerebellar functions; lower extremity peripheral nerves; proprioception; reflexes Vision |