
Am Fam Physician. 2004;70(2):361-363
A seven-year-old girl with a three-day history of fever as high as 40°C (103°F) came to an urgent care clinic located in the Central Valley area of California. Twelve hours after the onset of fever, she started to have flank and abdominal pain. She had no complaints of cold or influenza symptoms; no cough; and no diarrhea, nausea, or vomiting. Her parents reported no known drug allergies. Her fever was reduced by acetaminophen. Her only antibiotic exposure was amoxicillin as an infant. She had no recent travel history and no pets at home. The urgent care physician started her on trimethoprim-sulfamethoxazole for possible urinary tract infection.
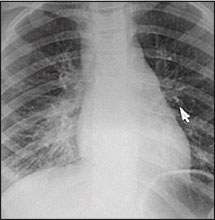
Approximately 12 hours after receiving her first antibiotic dose, she started to have red spots on her trunk and extremities. These spots later became confluent, with some central clearing and a purple hue (Figures 1 and 2). Ulcerations appeared on her lips, but she was still able to eat and drink. Her parents brought her back to the urgent care clinic. On repeat evaluation, she was ill-appearing but was in no respiratory distress. Her white blood cell count was 7,700 per mm3 (7.7 × 109 per L), with a differential that showed 80 percent polymorphonucleocytes (with no bands), 12 percent lymphocytes, 8 percent monocytes, and no eosinophils. Serum chemistries and urinalysis were normal. Clinical chest examination was normal, but a chest radiograph demonstrated right lower lobe pneumonitis (Figure 3).


Question
Discussion
The answer is C: Valley fever. Coccidioidomycosis is endemic to dry, arid areas of the Western Hemisphere, including the southwestern United States. It is particularly common in the Central Valley of California where this patient lived. Only 40 percent of persons who are infected become symptomatic. Of these, most have a self-limited infection. Pregnant women and immunocompromised patients (e.g., those with human immunodeficiency virus infection) are at increased risk for disseminated infection. If the infection is symptomatic, it often presents with chest pain, cough, and fever. Several different types of immune-mediated rashes may occur, including erythroderma, macular exanthem, erythema multiforme (as in this patient), or erythema nodosum. Arthralgias also can occur with primary infection. Disseminated disease, which occurs in about 1 percent of patients, can affect the skin (e.g., granulomas, abscesses, pustules), joints, or the central nervous system. Serologic testing for IgM antibody is positive in most, but not all, cases within one to three weeks of symptom onset. If initial antibody testing is negative, but clinical suspicion of coccidioidomycosis is high, repeat testing is indicated because it may take a month or more to develop measurable antibody titers. Cases that are not self limiting are treated with antifungals, and occasionally surgery is necessary for persistent focal lesions.1,2
The fever, rash, and mucosal changes in this patient could be consistent with Kawasaki disease. However, this disease typically occurs in children younger than five years, is more common in boys, and does not include pneumonitis as a typical finding. The criteria for Kawasaki disease include fever lasting more than five days (often as high as 40 to 41°C [104 to 105°F], with poor response to antipyretics) and four of the five following clinical findings: conjunctivitis, oropharyngeal changes (e.g., fissured lips, injection, strawberry tongue), peripheral extremity changes (e.g., edema, desquamation, erythema), exanthem, and cervical lymphadenopathy.3,4
Multiple medications, including those containing sulfa, can cause erythema multiforme. Erythema multiforme can be divided into minor and major types. The major type also is known as a Stevens-Johnson reaction, which is associated with a greater number and severity of skin lesions and affects the mucous membranes. When a medication causes erythema multiforme, it usually occurs two to three weeks after exposure,3 not hours after the first dose, as occurred in this case. An allergic reaction could have happened within this 12-hour timeframe, but it would have caused hives or a morbilliform rash, sometimes with associated wheezing or even circulatory collapse from anaphylaxis.
Rocky Mountain spotted fever has been diagnosed all across the United States, but the highest incidence occurs in a band from Oklahoma to North Carolina. It is caused by infection with Rickettsia rickettsii, an intracellular bacterium transmitted by ticks that are found on wild animals and domestic dogs. Infection in humans can occur at any age, but more serious sequelae may develop in young children. The prodrome starts with fever, malaise, and severe headache. Blanching macules or papules on the extremities (especially palms and soles) appear two to three days later, which may then progress to palpable purpura or necrotic ecchymoses. Associated laboratory findings may include thrombocytopenia, hyponatremia, and liver function test abnormalities. Rocky Mountain spotted fever is fatal in 2 to 7 percent of cases, primarily because of the delay in diagnosis and initiation of treatment with doxycycline.3–5
Measles begins with a typical viral prodrome, followed by prominent cough, coryza, and conjunctivitis, which did not occur in this patient. The maculopapular rash that occurs with measles begins at the face, then spreads to the trunk and extremities, and may become confluent. Children who lack proper immunization are at risk of measles.
| Condition | Characteristics |
|---|---|
| Kawasaki disease | Fever lasting longer than five days, conjunctivitis, mucosal changes, edema, desquamation, and cervical lymphadenopathy |
| Bacterial pneumonia with allergy to sulfa medication | Systemically ill, raised plaque-like hives in response to allergy to antibiotic, subacute rash may be morbilliform |
| Valley fever (coccidioidomycosis) | Endemic to Southwest United States, influenza-like illness, pneumonitis, several types of rash possible, another great imitator |
| Rocky Mountain spotted fever | Fever, malaise, headache, thrombocytopenia, hyponatremia, and petechial rash |
| Measles | Cold-like symptoms, Koplik spots (white spots with red halo) on buccal mucosa, then rash starts on head, quickly spreads, confluent, all areas maximal intensity simultaneously |