
Am Fam Physician. 2004;70(10):1969-1970
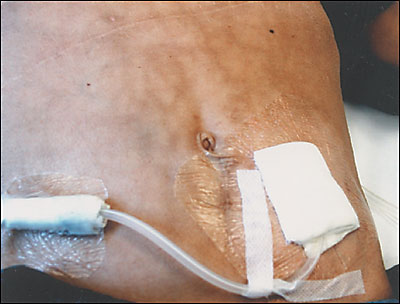
An 18-year-old patient on peritoneal dialysis presents to an outpatient clinic with asymptomatic reticular hyperpigmentation of the skin on the upper left abdomen. This condition has been present for at least six months. The patient is receiving dialysis treatment for end-stage renal disease from hemolytic uremic syndrome (catheter exit site is visible in the accompanying figure). The long-term management of the renal failure has been complicated by anemia, acidosis, secondary hyperparathyroidism, growth retardation, and malnutrition. The patient has recurrent episodes of abdominal pain caused by an enteropathy of unknown origin. Pain medication consists of an opioid, a spasmolytic agent, and nonsteroidal anti-inflammatory drugs. In addition, the patient uses a hot water bottle over the upper abdomen regularly for pain alleviation.
Question
Discussion
The correct answer is B: erythema ab igne. Erythema ab igne is a reticular erythematous hyperpigmentation caused by repeated skin exposure to moderate heat. This patient uses a hot water bottle daily to alleviate pain.
Erythema ab igne is caused by heat radiation or direct application of heat (e.g., hot water bottles or heating pads). In the past century, erythema ab igne was a common condition on the legs of persons who used to sit close to open fires or ovens. It also has been described in patients with occupational exposure to heat, for example on faces and palms of cooks and silversmiths, and on the legs of chimney sweeps. There are anecdotal descriptions of associations between erythema ab igne and chronic pancreatitis,1 peptic ulcers, chronic back pain, and abdominal primary or metastatic cancer.2 Chronic pain with use of heat for pain relief is the likely unifying factor for these reported associations, rather than a pathophysiologic link to the diseases. Also, there is a possible association with squamous cell skin cancers, which have been reported to occur in areas of erythema ab igne.
Erythema ab igne begins as a mild transient reticular pattern of erythema. Over months of continued heat application, the erythema persists and becomes more hyperpigmented. Later in the course, the affected skin becomes widely hyperpigmented and atrophic with only the borders showing a reticular pattern. Sometimes subepidermal bullae or hyperkeratotic changes develop. Erythema ab igne is usually asymptomatic, although mild itching or burning may occur.
A 3- to 4-mm punch biopsy to confirm the diagnosis is recommended only if the history is inconclusive or malignant skin changes are suspected. Histology usually shows epidermal atrophy with flattening of the dermo-epidermal junctions, collagen degeneration, and relative increase in dermal elastic tissue.
Mildly hyperpigmented lesions may resolve within several months if the heat application is stopped. With more advanced lesions, patients should be advised about the possible risk of skin cancer and regularly monitored for malignant changes. Topical treatment with 5-fluorouracil cream has been shown to clear epithelial atypia.3 Cosmetic improvement has been reported with laser therapy or topical treatment with tretinoin or hydroquinone.4
Cutis marmorata is a reticular bluish skin discoloration that occurs as a physiologic reaction to cold exposure, especially in young children and infants. In contrast to erythema ab igne, there is no hyperpigmentation and the discoloration resolves with warming of the skin.
Livedo reticularis occurs with conditions that lead to spasm or obstruction of the deep vascular network in the skin, such as Raynaud’s phenomenon, systemic lupus erythematosus, antiphospholipid antibody syndrome, or cryoglobulinemia. The reticular pattern is accentuated by cold but tends to persist somewhat when the skin is rewarmed. The trunk, legs, and forearms are most commonly affected.
Acanthosis nigricans is a brown or gray hyperkeratotic skin discoloration that most often is associated with obesity and insulin resistance, especially in persons with a darker skin complexion. Patches of confluent discoloration most commonly occur on the posterior neck or in the axillae. Acanthosis nigricans also may be seen as a paraneoplastic syndrome, associated with gastrointestinal malignancies. In these cases, lesions tend to arise more rapidly, are more extensive, and may occur in atypical locations such as the hands and feet or mucous membranes.
Granuloma annulare may present as a serpiginous, hyperpigmented skin discoloration, but the skin lesions would be raised papules, not just macular skin changes as in this case. Granuloma annulare may involve the trunk or any other skin surface, but it most commonly occurs on the extremities.
| Condition | Characteristics |
|---|---|
| Cutis marmorata | Reticular bluish discoloration; no hyperpigmentation; resolves with warming of skin; young children and infants |
| Erythema ab igne | Reticular (net-like) erythematous and/or hyperpigmented in areas of chronic and repeated heat exposure |
| Livedo reticularis | Livid reticular pattern; no hyperpigmentation; accentuated by cold; persists with rewarming of skin; common on trunk, legs, and forearms |
| Acanthosis nigricans | Brown or grey keratotic hyperpigmentation; not reticular; usually on posterior neck, in axilla, or other skinfolds; possibly paraneoplastic |
| Granuloma annulare | Circular array (a few centimeters in diameter) of papules or coalesced papules; usually on the extremities |