
Am Fam Physician. 2004;70(11):2113-2120
Early childhood caries is the most common chronic disease in young children and may develop as soon as teeth erupt. Bacteria, predominately mutans streptococci, metabolize simple sugars to produce acid that demineralizes teeth, resulting in cavities. Physicians should examine children’s teeth for defects and cavities at every well-child visit. Any child with significant risk factors for caries (e.g., inadequate home dental care and poor oral hygiene, a mother with a high number of cavities, a high sugar intake, enamel defects, premature birth, special health care needs, low socioeconomic status) should be referred to a dentist by 12 months of age. Promoting appropriate use of topical and systemic fluoride and providing early oral hygiene instruction can help reduce caries in young patients, as can regularly counseling parents to limit their child’s consumption of sugar.
The most common chronic disease of childhood is early childhood caries (dental caries in children younger than six years).1 It is five times more prevalent than asthma.2 Most children do not receive dental care until they are three years old, yet by that time more than 30 percent of children from lower socioeconomic groups already have caries.3
| Key clinical recommendation | Label | References |
|---|---|---|
| Maternal periodontal disease has been linked to preterm labor. The results of initial trials suggest that periodontal therapy can decrease the risk of prematurity. | B | 15,16 |
| Mothers with caries should use xylitol chewing gum four times daily because this may reduce the risk for caries in her child. | B | 20 |
| Systemic fluoride is one of the most effective tools in the prevention of dental decay and has been shown to reduce caries in young children by 40 to 50 percent. | A | 24 |
| Maternal oral health should be monitored after delivery because decreasing maternal mutans streptococci levels can reduce infant colonization and subsequent caries risk. | B | 18 |
Despite its high prevalence, early childhood caries is a preventable disease. Primary care physicians see children at least 11 times for well-child visits through age three and serve as the entry point into the dental care system. Family physicians caring for both pregnant mothers and infants are uniquely situated to provide early risk assessment, prevention, detection, and referral. Addressing oral health during well-child visits requires little time and involves refocusing existing activities rather than introducing new ones.
Etiology
Early childhood caries (Figure 1) can develop as soon as teeth erupt. Cavities (Figure 2) may be visible as early as 10 months of age.4 Caries typically presents in children as white spots or lines (Figure 3) on the maxillary incisors, which are among the first teeth to erupt and the least protected by saliva. If untreated, these white areas will rapidly break down into yellow-brown cavities (Figure 4), and the disease will spread to the posterior teeth.




Early childhood caries is an infectious bacterial disease of teeth. Bacteria, predominately mutans streptococci, metabolize monosaccharide and disaccharide sugars to produce acid that demineralizes teeth and causes cavities. The interplay of these three etiological factors (teeth, bacteria, and sugar) controls the severity of the disease.
Eruption of teeth in infants is highly variable. The primary incisors typically begin to erupt between six and 12 months of age. The first molars erupt at about one year and the second molars at about two years. Teeth that erupt with enamel defects, typically areas of white, brown, or rough enamel, are at greater risk of caries.5 Defects are more prevalent in children who are born prematurely or have a low birth weight, and in children of low socioeconomic status.6
The exact age at which mutans streptococci colonization occurs in children is controversial, but it usually does not happen until teeth erupt. The earlier colonization occurs, the greater the risk of caries.7 Mutans streptococci typically originate in the mother8 and are transmitted to the child via saliva contact. Elevated maternal levels of mutans streptococci, due to active or untreated caries and frequent sugar consumption, increase the risk of transmission.9 In addition, recent evidence suggests that exposure to environmental tobacco smoke increases the likelihood of streptococci colonization in children.10
The frequency of sugar consumption is the main dietary variable in caries etiology.11 After bacteria metabolize sugar into acid, it takes 20 to 40 minutes for the acid to be neutralized or washed away by saliva. Therefore, if sugars are frequently consumed, the potential for demineralization is greater. Although mutans streptococci can metabolize many different carbohydrates, they produce acids most efficiently from sugars, especially sucrose. Lactose is one of the least cariogenic sugars. Evidence suggests that bovine milk is not cariogenic and may be protective.5 Sugars located within the cellular structure of food (such as fructose in whole fruit) are thought to be less cariogenic than sugars intentionally introduced into foods.12
Early childhood caries was historically attributed to inappropriate and prolonged bottle use; hence the older terms of “baby-bottle tooth decay” and “nursing caries.” Recent analysis indicates that the disease is multifactorial.13 Any practice that allows frequent sugar consumption in the presence of mutans streptococci may result in caries formation. Common contributing etiological practices in children include propped bottles containing sweetened liquids, frequent consumption of sweetened liquids from infant- and toddler-size “sippy” cups, and frequent snacking. The caries risk generated by on-demand breastfeeding is unclear, but because lactose is poorly metabolized by mutans streptococci,14 other concomitant inappropriate dietary practices (e.g., frequent juice consumption or snacking) are more likely to be the culprits.
Oral Health Promotion
PRENATAL VISITS
Pregnant women should be evaluated for cavities, poor oral hygiene, inflamed gingiva, and loose teeth, as well as frequency of sugar consumption. Prenatal counseling should focus on referral to a dentist to treat existing caries and periodontal disease. Oral hygiene should be optimized with twice-daily toothbrushing using fluoride toothpaste and once-daily flossing. An over-the-counter, alcohol-free, 0.05 percent fluoride mouth rinse also may be recommended for women with active caries.17 The consumption of sugars should be minimized and restricted to meal times.
Maternal oral health should be monitored after delivery because decreasing maternal mutans streptococci levels can reduce infant colonization and subsequent caries risk.18 It also has been suggested that mothers use xylitol chewing gum four times daily19 because this may reduce caries in their children.20
BIRTH TO THREE MONTHS OF AGE
A risk assessment is integral to development of an appropriate prevention and referral plan for infants. Young infants with special health care needs, mothers with high caries rates, and families of low socioeconomic status have high caries risk.19 Identification of increased risk warrants reinforcement of good maternal oral health habits as well as vigilant preventive efforts for the infant.
Initial counseling should focus on diet. Breastfeeding is the preferred source of infant nutrition. If the infant is bottle-fed, the mother should hold the infant when feeding, and the bottle should not be propped or placed in bed. Only formula or breast milk should be used in the bottle. Fruit juice is discouraged because it is cariogenic and has been associated with failure to thrive.21 Some formulas, especially soy-based formulas that contain sucrose, can be cariogenic.22
FOUR MONTHS OF AGE
Teething symptoms include fussiness, increased sucking behavior, and loose stools. Increased drooling is common at this age but not necessarily associated with teething. Temperatures higher than 38.1°C (100.6°F) are not associated with teething and should be evaluated for other causes.23 Symptomatic relief of teething discomfort includes sucking on cold teething rings or wash-cloths. Numbing gels are less helpful and, in high doses, can be harmful.
At the four-month well-child visit, sources of systemic fluoride should be assessed. Systemic fluoride is one of the most effective tools in the prevention of dental decay and has been shown to reduce caries in young children by 40 to 50 percent.24 Fluoride increases the resistance of the teeth to demineralization, promotes re-mineralization, and exerts bacteriostatic properties. Many large municipal drinking water supplies are fluoridated to an optimal level of 1 part per million (ppm). However, more than one water utility often serves a community. Therefore, patients must determine the fluoridation level of their drinking water by contacting their supplier. Well water must be tested for fluoride content because levels vary even within neighborhoods. Testing kits and services are widely available.
SIX TO 12 MONTHS OF AGE
All children should receive appropriate systemic and topical fluoride beginning at six months of age.17,25 If a child’s home receives commercially fluoridated water, or the family’s well water has more than 0.6 ppm of fluoride, no systemic supplementation should be given, even if alternative water sources are used at times (e.g., bottled water). Systemic supplementation also is not recommended if the child is breastfeeding. If a child receives water from a nonfluoridated source or a well with less than 0.6 ppm of fluoride, supplementation should begin at six months of age. Table 117 provides fluoride supplementation guidelines. Fluoride solution or chewable tablets should be specified because these increase oral levels of fluoride. Fluoride supplementation should not be given with formula or milk, which decrease absorption.
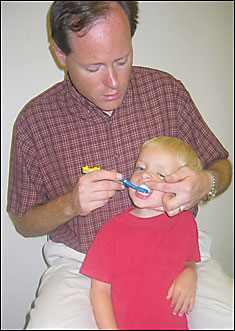
The use of fluoridated toothpaste along with oral hygiene instructions should be promoted at the six-month well-child visit. Caregivers should brush children’s teeth twice a day using a small soft brush with a dab of fluoride toothpaste the size of a rice grain or the tip of a pencil eraser (Figure 5). The caregiver should brush the child’s teeth from behind the child while supporting the child’s head (Figure 6). Brushing should focus on the junction between the gingiva and teeth. Excess toothpaste should be spit out, but rinsing should be discouraged because residual fluoride toothpaste on the teeth increases the caries preventive effect.26

Chronic excessive fluoride intake can result in fluorosis, an unaesthetic mottling of the teeth. Therefore, fluoride intake should be optimal but not excessive.27 In children at low risk for caries, the risks and benefits of fluoride supplementation should be weighed. It may be appropriate to consider decreasing or eliminating fluoride supplementation and delaying the use of fluoride toothpaste until the age of two years in some low-risk patients.17,24
Acute excessive fluoride intake at doses under 5 mg per kg can cause nausea and vomiting. For an average five-year-old, a dose of 5 mg per kg of fluoride from toothpaste represents 95 mL, or about one half of a typical 8-oz tube. Larger doses of fluoride can cause life-threatening hypocalcemia with convulsions, tetany, decreased myocardial contractility, ventricular arrhythmias, and cardiac arrest. Management of overdosing includes oral administration of calcium, induction of vomiting, and cardiac monitoring. Parents should be counseled to keep fluoride preparations out of reach of children and to assist with dispensing them. Prescriptions for fluoride supplements should not exceed 120 mg.28–30
Dietary instruction should be provided within a dental health construct. As finger foods are introduced, sugar-containing foods should be limited to meal times, and a regular pattern of meals and set snacks should be developed, rather than “grazing.”
The sippy cup should be introduced at six months of age in preparation for weaning from the bottle or breast at 12 months. Drinks between meals should be limited to water and plain milk. Juice, if introduced, should be limited to no more than 4 to 6 oz per day and only consumed in cups31 and during a meal. Eating whole fruit is preferable to drinking fruit juice.31
Dental screening should be instituted at the 12-month well-child visit, with the child examined in a lap-to-lap position or supine on the examination table to ensure adequate visualization of the teeth and oral structures (Figure 7). The teeth should be examined for white spots, cavities, and defects. Any deviation from normal creamy white teeth, or the presence of plaque, indicates a significant caries risk and the child should be referred immediately for dental care.19

The American Academy of Pediatric Dentistry recommends that all children see a dentist by the age of 12 months,32 while the American Academy of Pediatrics recommends that children at “caries risk” see a dentist by the age of 12 months.19 At 12 months, it is considered appropriate to briefly reassess the caries risk of the child and mother and determine if variables have changed. Children at risk for caries should be referred immediately to a dentist. Physicians who choose to refer low-risk children closer to the third birthday must continue active dental prevention and screening at every well-child visit.
FIFTEEN MONTHS AND OLDER
From the 15-month well-child visit forward, messages about dental care should become consistent. Each child should have an established source of dental care. Dental screening should be performed at each visit to evaluate for caries and other pathology, and to monitor oral hygiene. Oral hygiene should be reinforced along with the use of fluoride toothpaste for every child from two years of age and onward.17 Parental assistance with toothbrushing should continue until eight years of age. Dietary advice should focus on limiting snacks and drinks between meals and limiting sweetened foods to meal times. The need for systemic fluoride supplementation should continue to be evaluated and supplements prescribed, if appropriate, through age 16. The appropriate use of mouth guards and face shields should be advocated. Table 2 summarizes guidelines for infant oral health.
| Visit | Dentist referral | Caries risk assessment | Screening | Diet | Fluoride | Oral hygiene |
|---|---|---|---|---|---|---|
| Prenatal | Refer mother for treatment of active caries and periodontal disease | Yes | Yes, to help determine caries risk | Restrict simple sugars to meals Limit number of snacks | Fluoride toothpaste and fluoride mouthwash | Toothbrushing and flossing |
| Birth to three months | — | Yes | — | Hold infant if bottle feeding No bottle in bed or bottle propping | — | — |
| Four months | — | Yes | — | Hold infant if bottle feeding No bottle in bed or bottle propping | Determine water fluoride level (test if well water) | — |
| Six to 12 months | Refer child for preventive dental care | Yes | Check for presence of defects, caries, and poor oral hygiene | Hold infant if bottle feeding No bottle in bed or bottle propping Introduce sippy cup Discontinue bottle by 12 months Restrict simple sugars to meals Limit number of snacks Only plain milk/tap water between meals | Prescribe systemic fluoride if indicated Use fluoride toothpaste | Toothbrushing instruction before teeth erupt |
| ≥ 15 months | Ensure child has regular source of dental care | Yes | Check for presence of defects, caries, and poor oral hygiene | Bottle discontinued No ad lib sippy cup use Restrict simple sugars to meals Limit number of snacks Only plain milk/tap water between meals | Prescribe systemic fluoride if indicated Use fluoride toothpaste | Reinforce toothbrushing |