
Am Fam Physician. 2005;71(5):961-962
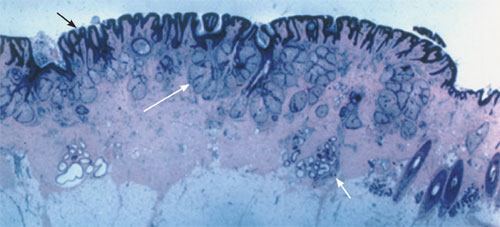
A 13-year-old girl presented with a 13-year history of slowly enlarging scalp lesions. Her medical history was unremarkable. Examination revealed yellow to dark-brown, hairless, verrucous and micronodular lesions on the right temporal area of her scalp (Figure 1). The results of routine blood tests and urinalysis were within normal limits. A biopsy specimen was obtained (Figure 2).

Question
Discussion
The answer is C: Nevus sebaceus. Nevus sebaceus arises secondary to disordered development of epithelial, pilar, sebaceous, and apocrine structures.1 Lesions generally present as a yellowish orange area on the scalp, face, neck, and auricular area2; the vast majority of lesions arise before patients reach 10 years of age. The lesions are most common on the scalp, followed by the face, with few lesions situated away from the head. At puberty, the lesions become verrucous, micronodular, and yellow to dark brown in color.2 Nearly all are hairless, and the final stage of nevus sebaceus is the development of secondary tumors within the lesion.2 While most neoplastic proliferations are benign, several malignant tumors have been reported in these lesions.1,3 The most common benign growth is syringocystadenoma papilliferum, while basal cell carcinoma is the most frequently seen malignant process.1 In Figure 2, the long white arrow = increased number of sebaceous glands; short white arrow = increased number of apocrine glands; short black arrow = hyperplastic, papillated epidermis.
Because various neoplasms may occur, prophylactic surgical excision during childhood often is recommended. However, malignancy is rare in children. There are great variations in the proportion of malignant tumors reported in published series because many of the previously described basal cell carcinomas actually could be trichoblastomas, which are benign follicular tumors.3–4 One study3 suggests that the benefit of prophylactic surgery in young children is uncertain because most tumors occur in adults older than 40 years. Excision should be recommended for patients in whom benign or malignant neoplasms are suspected clinically or for cosmetic considerations.5 Even lesions with clinical changes often are proved to be benign tumors or warts.3
Verruca vulgaris lesions grow relatively faster than those of nevus sebaceus, occur more often on the extremities and digits, and generally are the color of the patient’s skin. Unlike nevus sebaceus, they are rough in texture, and not yellow or red in color.
Epidermoid cysts are normally the same color as the patient’s complexion or reddish if inflamed, can be mobile when pinched, and may excrete cottage-cheese–like material.
Basal cell carcinomas are an extremely rare occurrence in a generally healthy adolescent, usually more rapidly growing, with a rolled pearl border and, rarely, a necrotic center.
Epidermal nevus is a congenital lesion presenting at birth or in childhood. The lesions are yellow to brown in color, may be wart-like, and may develop in a linear pattern.6
| Condition | Characteristics |
|---|---|
| Verruca vulgaris(common wart) | Round, firm, hyperkeratotic papules; mostly on extremities, 1 to 10 mm |
| Epidermoid cyst | Dermal to subcutaneous nodule, usually with a central punctum, containing keratinaceous material, 0.5 to 5 cm |
| Nevus sebaceus | Hairless, verrucous, micronodular, elevated plaque, 1 to 2 cm |
| Basal cell carcinoma | Smooth, firm, “pearly,” umbilicated papule or nodule with fine telangiectasia, and sometimes a necrotic center with rolled border, mostly a few millimeters to several centimeters |
| Epidermal nevus | Yellow to brown, verrucous, elevated lesions with well-defined borders; may form a linear pattern |
| Seborrheic keratosis | Skin-colored to gray to brown/black, papule or plaque with warty surface, 1 mm to 6 cm |