
Am Fam Physician. 2005;71(10):online-only-
to the editor: We read with interest the article, “Management of Corneal Abrasions” by Drs. Wilson and Last1 in American Family Physician. We would like to highlight the importance of looking for subtarsal foreign bodies in relevant cases of eye injury.
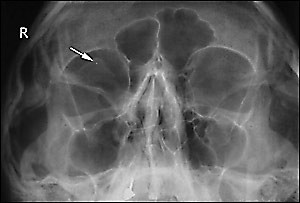
A 25-year-old man attended the emergency department after molten metal splashed into his right eye. His eyes had been irrigated at his workplace. The emergency department physician examined his eyes and could not find any obvious foreign body. When the patient still had pain and foreign body sensation in his right eye, orbital radiographs were taken, which showed a small, round, radio-opaque shadow in the right orbit consistent with a metallic foreign body (Figure 1). The exact location of the foreign body could not be determined, so the patient was referred to the on-call ophthalmologist.
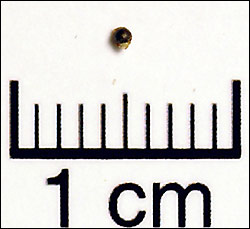
On ocular examination, the patient’s visual acuities were 20/20 (unaided) in both eyes. Slit lamp examination showed mild medial conjunctival congestion in the right eye. No abnormalities of the conjunctiva or cornea were seen on fluorescein staining, and there was no entry wound. Eversion of the right upper eyelid showed a subtarsal metallic foreign body. The rest of the ocular examination was unremarkable. The subtarsal foreign body (Figure 2) was removed under topical anesthesia, and the patient was discharged with a prescription for topical antibiotics.
Eye injuries from foreign bodies remain one of the most common presentations to the emergency department. Eversion of the upper eyelids to rule out subtarsal foreign bodies is an essential part of ocular examination in all patients with a history of eye injuries. In our patient, the subtarsal foreign body was overlooked because eyelid eversion was not performed. Failing to do this simple technique may result not only in performing unnecessary investigations, but, more importantly, in subtarsal foreign bodies going undetected, which can lead to complications such as persistent grittiness, corneal abrasions, recurrent traumatic keratitis,2 and granuloma formation.3
A review article4 showed that most orbital radiographs are performed needlessly. They suggested restricting radiologic investigations to patients with clinical evidence of penetrating ocular or orbital trauma, or a subconjunctival hemorrhage.
Newman5 reported that an eyelid foreign body may mimic an intraocular foreign body on plain radiography, which was the case in our patient.
This case report demonstrates the importance of examination by upper-eyelid eversion in patients who present with a history of ocular injury or grittiness and a foreign body sensation in the eye. This simple technique may prevent complications caused by missed subtarsal foreign bodies such as corneal abrasions and infections, and also avoid unnecessary imaging studies.