
Am Fam Physician. 2006;73(5):827-834
This is part II of a two-part article on finger injuries. Part I, “Tendons and Ligaments” appears in this issue of AFP.
Related article: Common Finger Fractures and Dislocations
Patient information: See related handout on rehabilitation exercises after finger injuries, written by the authors of this article.
Author disclosure: Nothing to disclose.
Family physicians can treat most finger fractures and dislocations, but when necessary, prompt referral to an orthopedic or hand surgeon is important to maximize future function. Examination includes radiography (oblique, anteroposterior, and true lateral views) and physical examination to detect fractures. Dislocation reduction is accomplished with careful traction. If successful, further treatment focuses on the concomitant soft tissue injury. Referral is needed for irreducible dislocations. Distal phalanx fractures are treated conservatively, and middle phalanx fractures can be treated if reduction is stable. Physicians usually can reduce metacarpal bone fractures, even if there is a large degree of angulation. An orthopedic or hand surgeon should treat finger injuries that are unstable or that have rotation. Collateral ligament injuries of the thumb should be examined with radiography before physical examination. Stable joint injuries can be treated with splinting or casting, although an orthopedic or hand surgeon should treat unstable joints.
This article discusses the evaluation, diagnosis, and treatment of common finger fractures and dislocations and thumb injuries. Part I1of this two-part article covers tendon and ligament injuries of the finger.
Physicians can treat most finger fractures and dislocations, although knowing when to refer a patient to an orthopedic or hand surgeon is important to ensure maximal future functionality. Examination of finger injuries includes radiography (oblique, anteroposterior, and true lateral views) and physical examination to detect fractures.2 Management of dislocations begins with reduction and then focuses on treating soft tissue damage.3 Fractures should be reduced if no rotation is present and then immobilized using splints or casts. Treatment of ligament injuries of the thumb depends on the presence or absence of fracture fragments and on the degree of joint stability. Anesthesia may be necessary to facilitate reduction.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Finger injuries should be evaluated with radiography (oblique, anteroposterior, and true lateral views). | C | 2 |
| Proximal phalanx and articular surface fractures involving more than 30 percent of the joint should be managed in consultation with an orthopedic or hand surgeon. | C | 10 |
| Fifth metacarpal bone fracture (boxer’s fracture) with angulations of 70 degrees or less heal with or without reduction and splinting. This should not dissuade physicians from attempting reduction, however. | B | 11 |
| An ulnar collateral ligament injury should be considered when a patient presents with traumatic thumb pain, and fracture should be ruled out with radiography before a stress test is performed. | C | 10,14 |
After an immobilization period, rehabilitative exercises should be performed to regain strength and mobility and to minimize chronic pain and stiffness. Rehabilitation exercises are explained in the accompanying patient information handout. Physicians should tell patients that it is common for an injured finger to remain swollen for some time and perhaps permanently. Table 1 summarizes the evaluation and treatment of common dislocation and fracture injuries of the finger and ulnar collateral ligament injuries of the thumb.
| Injury | Examination | Treatment | Referral criteria |
|---|---|---|---|
| Joint dislocations (dorsal PIP joint dislocation is most common) | Tenderness at volar plate with an obvious deformity |
| Avulsion fracture involving more than one third of the joint or irreducible injury |
| Check neurovascular status. | |||
| Radiography before and after reduction* | |||
| Metacarpal bone fracture (boxer’s fracture; most common above the fifth digit) | Determine extent of angulation and evaluate for rotation. |
| Rotation or angulation of more than 70 degrees |
| Middle phalanx fractures | Radiography to assess angulation, displacement, and rotation |
| Inability to maintain proper alignment or irreducible injury |
| Disruption of UCL at the thumb (skier’s thumb) | Pain at UCL |
| Fracture or unstable joint Stener lesion |
| Test for joint stability only if fracture is ruled out (anesthesia may be required). |
Dislocations
The most commonly dislocated joint in the body is the proximal interphalangeal (PIP) joint of the finger (“coach’s finger”).4 The severity of this injury often is underestimated and improper treatment can cause long-term morbidity. The direction of dislocation is usually dorsal, but lateral and volar dislocations sometimes occur.
PIP JOINT
Dorsal PIP joint dislocation can injure the volar plate or cause an avulsion fracture of the middle phalanx (Figure 1). A patient with a dorsally dislocated PIP joint will have tenderness at the volar plate and an obvious deformity. When evaluating a patient during an athletic event, the physician can attempt reduction without radiography. If reduction is successful, the PIP joint should be splinted (e.g., buddy taping the injured PIP joint in slight flexion) and the patient may continue to participate in the athletic event.5 The injury must be reevaluated in the office, including radiography.
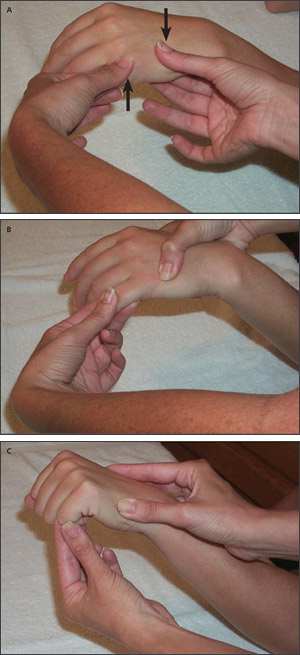
Reduction of a dorsal PIP joint dislocation may be achieved by gently applying distal traction to the injured finger while applying volarly directed pressure to the middle phalanx (Figure 2). Reduction is obvious when it occurs. If traction and volarly directed pressure is ineffective, the physician should hyperextend the distal portion to “unlock” the joint and continue applying traction and volarly directed pressure. If reduction is performed immediately, anesthesia is not needed. However, a digital block is usually needed for pain if presentation is delayed for more than one hour.6 For a digital block, 1 to 2% lidocaine (Xylocaine) without epinephrine is placed along both sides of the affected digit just distal to the MCP joint. A small-gauge needle (27 or 30 gauge) should be used.6 If radiography shows a large fracture fragment, or if reduction is unsuccessful, referral to an orthopedic or hand surgeon is necessary.
Radiographs should be obtained after reduction to evaluate joint congruity.3,7 The collateral ligaments should be examined, and active flexion and extension should be evaluated to ensure the integrity of tendons. The PIP joint should be splinted in 30 degrees of flexion, and the physician should follow up with radiography after one week to evaluate the healing progress (Figure 3). A stable joint should be splinted in flexion for two to four more weeks, depending on injury severity, followed by buddy taping.
Reduction of a lateral PIP joint dislocation is accomplished by applying reducing pressure to the deviated distal portion (middle phalanx) while stabilizing the proximal portion (proximal phalanx). Treatment should focus on soft tissue damage and include follow-up radiography.
Volar dislocation of the PIP joint is rare. This injury may cause a tear in the central slip of the extensor tendon or “button holing” of the proximal phalanx through the central slip. The physician may attempt reduction by hyperflexing the distal segment (middle phalanx) to “unlock” the joint and then applying traction. This should only be attempted once. If successful, the joint should be splinted in full extension for six weeks. If reduction is unsuccessful, or if avulsion involves more than one third of the joint, referral to an orthopedic or hand surgeon is needed.
DIP JOINT
Dislocation of the distal interphalangeal (DIP) joint usually is caused by a crushing injury, and associated trauma may complicate treatment.8 Uncomplicated DIP joint dislocations are reduced and treated the same as PIP joint dislocations. After one week, a stable joint should be splinted in flexion for two to four weeks followed by buddy taping and follow-up radiography.
MCP JOINT
The metacarpophalangeal (MCP) joint most commonly dislocated is that of the thumb. A simple dislocation involves no soft tissue obstruction, and reduction should be attempted. A complex dislocation involves intervening soft tissue (i.e., ligaments, musculature, or fascia) and requires surgical reduction. Reduction is the same as for PIP and DIP dislocations. Splinting depends on the direction of the dislocation. A reduced dorsal MCP joint dislocation will have injured volar structures, as does a PIP dislocation. Therefore, a splint that does not allow full extension is necessary, as it is with a PIP dislocation. The opposite is true for a volar dislocation; there will be injured dorsal structures, and splinting should be initiated to maintain extension.
Fractures
Fractures should be reduced and then assessed using radiography. Treatment depends on rotation and extent of the fracture fragment.
PHALANX FRACTURE
A physician can treat middle phalanx fractures if proper alignment is achieved through reduction. This may be difficult because of the tension created by the extensor and flexor tendons.
A digital or hematoma block should be used to facilitate reduction. To accomplish a hematoma block, clean the area and inject 5 to 10 mL of 1 to 2% lidocaine without epinephrine directly into the fracture site. The goal is to aspirate blood after initial injection, to inject again, then to repeat this procedure until all of the anesthesia has dispersed into the fracture (i.e., the volume of blood in the syringe is equal to the amount of anesthesia that was initially administered).9 After adequate anesthesia has been administered, gently manipulate the fragments until correct alignment is achieved. Do not perform this procedure in patients with grossly contaminated skin (because of osteomyelitis risk) or open fractures, or in small children.
Subtle rotation can be detected with radiography or by evaluating the patient’s fist or semiflexed fingers. If no rotation is present, all of the fingernails will be on the same plane and will be pointing towards the scaphoid bone9 (Figure 4). A patient should be referred to an orthopedic or hand surgeon if reduction is unsuccessful or if rotation is detected.
If reduction is successful, the PIP joint should be splinted in extension using a dorsal aluminum splint for six weeks followed by buddy taping for another six weeks. Proximal phalanx and articular surface fractures that involve more than 30 percent of the joint should be treated by an orthopedic or hand surgeon.10
A fracture at the DIP joint usually is caused by a crushing injury. Unless severe angulation or displacement is present, these fractures should be reduced, treated by splinting the DIP joint in full extension using a stack or aluminum splint for four to six weeks, and reevaluated. Many injuries will be stable but may require protection if athletic participation continues.8
METACARPAL BONE FRACTURE
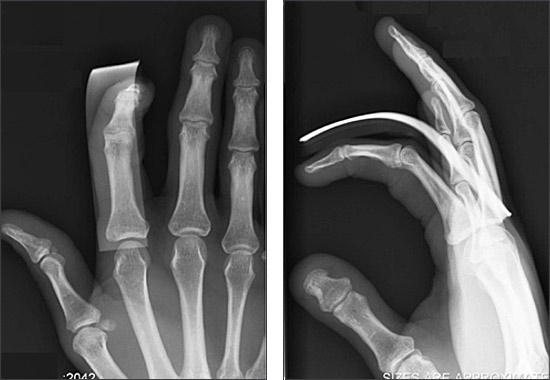
Fracture at the neck of the fifth metacarpal bone (boxer’s fracture), often caused by a missed punch during a boxing match, is the most common metacarpal bone fracture. Although not truly a finger fracture, this injury is included in this article because of its prevalence. The distal fracture fragment usually displaces at a volar angle because of the action of the interosseous muscles (Figure 5).
Most patients require anesthesia with an ulnar or hematoma block before reduction is attempted. To accomplish an ulnar block, inject 5 to 7 mL of anesthetic, 1 to 2 cm deep between the flexor carpi ulnaris tendon and the ulnar artery to block the palmar branch of the ulnar nerve. To block the distal branch, 3 to 4 mL of anesthetic should be infiltrated subcutaneously in the area distal to the ulnar styloid.9 To achieve reduction of a metacarpal bone fracture, flex the MCP joint to 90 degrees, applying dorsally directed pressure to the volarly displaced metacarpal head and volarly directed pressure to the proximal fracture fragment. Alternatively, the proximal phalanx or PIP joint can be used as a lever arm to move the metacarpal head upward while counterpressure is applied to the proximal fracture fragment (Figure 6).
If reduction is successful, the finger should be splinted in 70 to 90 degrees of flexion for six weeks to avoid significant stiffness using an ulnar gutter splint or cast or a ready-made orthotic splint. A “glove” cast (i.e., a cast starting slightly distal to the palmar crease and ending just proximal to the MCP joint) can create some immobilization and protection while maximizing function.4
A randomized trial11 compared outcomes of metacarpal bone fractures after reduction and ulnar gutter splinting with no reduction and splinting. The trial showed that the treatments are equally effective if the fracture is not angulated more than 70 degrees.11 This result should not dissuade physicians from attempting reduction; it should provide reassurance that the fracture should heal well unless severely angulated or rotated. Complications from excessive angulation after a metacarpal bone fracture include a stiff MCP joint, a prominent metacarpal head in the palm, pain, and pseudoclawing. The patient should be warned that a permanent bump might be present regardless of treatment.13
Radiography should be performed seven to 10 days after treatment to ensure proper healing and then every two weeks during the six-week splinting period.3 Rehabilitative exercises should begin after the splinting period. Patients may participate in athletic events when strength and range of motion are equal to the contralateral side. Some physicians allow participation while the finger is in a protective splint.
Ulnar Collateral Ligament Injury
Disruption of the ulnar collateral ligament (UCL), also known as skier’s thumb, is usually caused by forced abduction of the MCP joint. The UCL may be partially or completely torn with or without an avulsion fracture. If left untreated, the joint will be unstable causing a weak pinch grip. A UCL injury should be considered when a patient presents with traumatic thumb pain.10,14
If tenderness is present at the UCL, radiography should be performed to rule out fracture before further evaluation. If a fracture is present, consultation with an orthopedic or hand surgeon is appropriate.10,14 Generally, nondisplaced fractures can be treated closed, whereas displaced fractures require surgery.
If no fracture is present, the joint should be stressed in full flexion to maximally isolate the ligament. Most data7 suggest referral to an orthopedic or hand surgeon if there is 35 to 40 degrees of joint opening or if there is no clear endpoint. The most practical way to measure this is to compare the amount of laxity of the injured hand with the uninjured hand (Figure 7). Physicians may provide local anesthesia or a digital block to facilitate the stress examination if needed.
UCL injuries may cause Stener lesions. Normally the UCL is underneath the adductor aponeurosis. Some injuries cause the proximal end of the UCL to become trapped outside of the adductor aponeurosis (Figure 8). This injury must be corrected with surgery. Stener lesions usually present as joint instability and a tender mass. If a Stener lesion is suspected, consultation with an orthopedic or hand surgeon is necessary.
Stable UCL injuries are treated with splinting using a thumb spica cast or splint (Figure 9) for six weeks. Commercial splints are an alternative to casting if patient compliance can be ensured. Patients may continue to participate in athletic events during the splinting period depending on their sports and positions. After six weeks of continuous splinting, most experts recommend dynamic splinting (i.e., splinting while participating in an athletic event) for another six weeks if the patient is an athlete.15,16

Injury to the UCL also can occur on the opposite side of the thumb at the radial collateral ligament. The injuries are treated similarly, but there is no risk of Stener lesion with radial collateral ligament injuries.