
Am Fam Physician. 2006;74(8):1377-1378
A 50-year-old white man with a history of hypertension and gout presented with a complaint that his kneecaps had started to hurt earlier that day. Physical examination revealed an antalgic gait, bilateral knee effusions without warmth, tenderness on palpation at the midpoint over the left patella, and a normal range of motion without ligamentous instability.
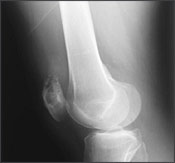
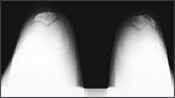
Laboratory evaluations included a complete blood count, serum electrolyte levels, liver function tests, and urinalysis, all of which were within normal limits. The calcium level was 8.4 mg per dL (2.10 mmol per L); protein level, 7.4 g per dL (74 g per L); albumin level, 5.1 g per dL (51 g per L); and alkaline phosphatase level, 69 units per L (1.16 μkat per L). The uric acid level was 8.1 mg per dL (480 μmol per L; reference: 2.0 to 7.0 mg per dL [120 to 420 μmol per L]), the erythrocyte sedimentation rate was 26 mm per hour, and the prostate-specific antigen was 1.94 ng per mL (1.9 mcg per L). Results of knee radiography are shown in the accompanying figures.

Question
Discussion
The answer is C: pathologic fracture secondary to gout. The radiographic images show bilateral osteolytic lesions within the patella, worse on the left, with bilateral pathologic fractures. The left patella has a vertical fracture on its lateral portion with a lytic lesion at the insertion of the quadriceps tendon (Figures 1 and 2). The right patella is fractured horizontally along its inferior margin (Figure 3).
Gouty tophi are masses resulting from soft tissue deposition of urate crystals. Intraosseous crystal deposition occurs in rare cases. In the patella, this can lead to destructive tophus formation. Fracture secondary to gout is rare, with descriptions limited to case reports.1–3 The mainstay of treatment for tophaceous gout is pharmacologic control of the hyperuricemia. Treatment can lead to shrinkage or resolution of the tophi.
Most skeletal lesions affecting the patella are nonmalignant and are associated with conditions such as chondroblastoma, giant cell tumor, osteomyelitis, and gout. Malignant processes involving the patella are unusual. Isolated occurrences of plasmacytoma, osteosarcoma, hemangiosarcoma, malignant lymphoma, and metastatic disease have been reported.4 Most of these lesions are unilateral.
Osteosarcoma is a malignant bone tumor that occurs primarily in the metaphyses of adolescents with open physes or in young adults.5
Pigmented villonodular synovitis is a benign process that affects the synovial lining of joints. Unilateral involvement of the knee is the most common finding and occurs in about 80 percent of patients. The diffuse form of this condition involves the entire synovium and may extend to a mass effect, invasion of surrounding bone, and bony erosion.6
Bipartite patella is caused by failure of patellar ossification resulting in incomplete patellar fusion. Pain may occur; it most often affects adolescents. However, there are case reports of gouty tophi forming within the fibrous tissue joining the patellar fragments.7
Calcific tendinopathy involves hydroxyapatite crystal deposition in the tendons. It can result in chronic pain and is more common in the Achilles’ or rotator cuff tendons.
| Condition | Characteristics |
|---|---|
| Bipartite patella | Incomplete fusion of patellar components caused by failed ossification |
| Calcific tendinopathy | Hydroxyapatite crystal deposition in tendon |
| Osteosarcoma | Malignant tumor in long bone metaphyses |
| Pathologic fracture secondary to gout | Soft tissue deposition of uric acid; rarely, bony deposition and erosion |
| Pigmented villonodular synovitis | Benign synovitis; bony erosion in diffuse disease |