
Am Fam Physician. 2007;75(3):315-316
Author disclosure: Nothing to disclose.
Chronic obstructive pulmonary disease (COPD) is very different today, in both magnitude and character, than a mere two decades ago. The clinical presentation of COPD has evolved, and the prevalence of this syndrome has grown substantially. COPD was not among the leading causes of death a generation ago, but it is now ranked fourth. Fortunately, the means for physicians to help their patients with COPD also have improved significantly in recent years. With the new face of COPD, there is also an opportunity to make a fresh start at controlling this condition.
To effectively translate new research advances into clinical practice, the National Heart, Lung, and Blood Institute (NHLBI) and the American Academy of Family Physicians (AAFP), with other partners, have launched a new public awareness campaign, “COPD: Learn More, Breathe Better.” The goal of this campaign is to educate persons at risk of COPD about the disease and encourage them to seek medical advice if they experience symptoms. The campaign also will help physicians identify patients with COPD and will ultimately reduce the significant public health burden of COPD.
COPD originally was defined in terms of two more specific diagnoses: chronic bronchitis and emphysema.1 The collective term acknowledged that chronic bronchitis and emphysema were associated with cigarette smoking and airway obstruction, that both were “irreversible” and resistant to treatment, and that they often coexisted. Scientists now appreciate that COPD is more than the sum of chronic bronchitis and emphysema. Chronic lung inflammation and remodeling of small airways can produce COPD, even in the absence of bronchitic symptoms or radiographic evidence of emphysema. For this reason, the disease is now defined simply in terms of persistent airflow obstruction that is not fully reversible with inhaled bronchodilators.
COPD has become a common condition. Deaths attributed to COPD now total 5 percent of all mortality in the United States, and that percentage continues to increase. Unlike lung cancer and pneumonia, the other major respiratory causes of death, COPD also causes prolonged disability in millions of patients. The annual costs of COPD are considerable: $37.2 billion for health care, loss of work, and mortality. In addition to the 12 million persons in the United States who have been diagnosed with COPD, an estimated 12 million persons with the syndrome are not yet diagnosed,2 despite the easily recognizable risk factors, symptoms, and signs of the disease and the simplicity of confirming the diagnosis by office spirometry.
COPD is now recognized as a systemic disease. Its manifestations extend beyond the respiratory system and involve the cardiovascular, muscular, and immune systems.3 Heart disease is actually the most common cause of death in persons with COPD.4 An important aspect of caring for patients with COPD is preemptive management of the infections, weakness, weight loss, and heart disease that are likely to develop.
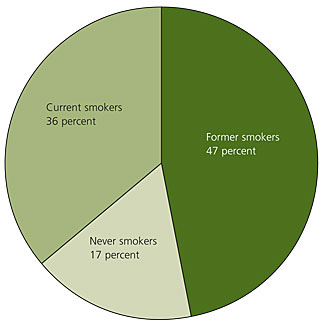
Risk factors other than cigarette smoking are important (Figure 15). Epidemiologic data indicate that approximately one out of every six patients with COPD has never smoked5,6; these patients represent 2 to 4 million cases of COPD in the United States. Occupational and environmental exposures may contribute to the development of disease in this group of never smokers,7 and genetic factors, including α1-antitrypsin deficiency, also may be important determinants of susceptibility.8 In addition, physicians are now recognizing many new cases of COPD among patients who quit smoking years before, suggesting that the effects of cigarettes can be persistent. Given the importance of risk factors other than cigarette smoking, and the fact that there are nearly 50 million former smokers in the United States,9 physicians must be alert to the possibility of COPD in non-smokers with symptoms of airflow limitation.
Women are affected as much as men. In 1959, men dying of COPD outnumbered women five to one, but now the ratio is approximately equal. In 2003, women accounted for 51 percent of all COPD-related deaths.10
Because patients with COPD typically are older, it is not surprising that they often have multiple medical diagnoses.4 The systemic nature of inflammation in COPD may even contribute to the development of other medical conditions. As a result, physicians face an increasing challenge in caring for patients with COPD because they often must manage a complex set of interacting diseases and drugs.
Recognition of the heavily addictive nature of nicotine has led to effective pharmacologic and behavioral interventions for smoking cessation. Furthermore, smoking cessation in patients with early COPD has been proven to decrease mortality rates and the rate of decline in forced expiratory volume in one second.11
Clinical trials have proved that inhaled bronchodilators and pulmonary rehabilitation improve functional capacity and quality of life and may reduce mortality rates.12,13 The benefit of oxygen supplementation has been proven in persons with severe resting hypoxemia, and lung volume reduction surgery is recommended for a subgroup of emphysematous patients.12–14 The availability of effective treatments makes early intervention increasingly important.
Scientific research is advancing rapidly. After decades of modest progress, researchers currently are making rapid advances using modern methods of genetics, genomics, and molecular pathology to better understand COPD.12,13 New theories of pathogenesis have been generated and are being tested in humans. The renewed interest in COPD research provides hope that novel therapies with the potential for modifying the disease process will soon be identified.
There recently has been a surge of interest in COPD among patient advocates, professional organizations, and the U.S. government. A COPD coalition and a Congressional caucus have been formed, and an international group, the Global Initiative for Chronic Obstructive Lung Disease, has developed updated guidelines for diagnosis and management.13
The NHLBI recognizes that family physicians, who provide care for most of the patients with COPD,13,15 have a greater opportunity than any other group to educate the public about the disease, correct outdated attitudes, obtain spirometric testing when appropriate, encourage smoking prevention and cessation, and prescribe effective medical management. Cooperation of the AAFP and other partners in the NHLBI campaign is a critical step in confronting the new face of COPD and working to make it less frightening and less prominent in years to come. By working together, we will achieve that goal.