
Am Fam Physician. 2007;76(2):237-244
Patient information: See related handouts on running and overuse injuries, plantar fasciitis and heel pain, and patellofemoral pain syndrome.
Author disclosure: Nothing to disclose.
Endurance athletes alternate periods of intensive physical training with periods of rest and recovery to improve performance. An imbalance caused by overly intensive training and inadequate recovery leads to a breakdown in tissue reparative mechanisms and eventually to overuse injuries. Tendon overuse injury is degenerative rather than inflammatory. Tendinopathy is often slow to resolve and responds inconsistently to anti-inflammatory agents. Common overuse injuries in runners and other endurance athletes include patellofemoral pain syndrome, iliotibial band friction syndrome, medial tibial stress syndrome, Achilles tendinopathy, plantar fasciitis, and lower extremity stress fractures. These injuries are treated with relative rest, usually accompanied by a rehabilitative exercise program. Cyclists may benefit from evaluation on their bicycles and subsequent adjustment of seat height, cycling position, or pedal system. Endurance athletes also are susceptible to exercise-associated medical conditions, including exercise-induced asthma, exercise-associated collapse, and overtraining syndrome. These conditions are treatable or preventable with appropriate medical intervention. Dilutional hyponatremia is increasingly encountered in athletes participating in marathons and triathlons. This condition is related to overhydration with hypotonic fluids and may be preventable with guidance on appropriate fluid intake during competition.
Participants in endurance sports span all ages, and although elite-level endurance athletes are typically in their 20s or 30s, the largest group of participants in many races are master-level athletes in the 35- to 50-year age group. These athletes have the time and inclination to pursue an intensive training regimen and consequently are at risk for overuse injuries or exercise-related medical conditions.
Clinical Assessment
Most injuries in endurance athletes are the result of overuse. The medical history should be used to develop a good understanding of the physical demands of the athlete's chosen sport, whether it is running, cycling, rowing, or cross-country skiing.
RUNNING
Running is the prototypical endurance sport. Evaluation of the injured runner should include details of how and when the symptoms began, the timing of symptoms (i.e., during and after exercise, or only afterward), the specific location of the pain (e.g., anterior knee, lateral knee), any previous similar injury, and any treatments that the athlete has already attempted.1 Overuse injuries can often be traced to a training error, such as overzealous escalation in weekly mileage or too much running overall. Known predictors for lower-extremity injury in runners include a history of previous lower-extremity injury and running more than 20 miles per week.2 The medical history should therefore include details about weekly running mileage, any changes in duration or intensity of training, changes in the type of running surface and surface grade, the age of footwear, and any recent changes in gait, shoes, or orthotics.1
Biomechanic and anatomic factors also may contribute to injury. Physical examination should include a careful evaluation of the injured area and may also require observation of gait and inspection for patellar malalignment, leg length discrepancy, foot morphology (e.g., for pes planus, pes cavus), and foot biomechanics (e.g., for hyperpronation.)
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Relative rest and activity modification are recommended for most overuse injuries. These interventions should be individualized based on duration and severity of symptoms as well as patient response to treatment. | C | 8 |
| Patellofemoral knee pain and iliotibial band friction syndrome in cyclists may be related to improper seat height or bicycle position, or pedal systems that are improperly adjusted. Examination of the cyclist on the bicycle can lead to appropriate intervention (e.g., change in seat height, stem length, or pedals). | C | 4, 5, 10, 18 |
| There is some evidence for the role of exercise therapy for the treatment of patellofemoral pain syndrome. Knee sleeves and taping may be helpful, but these therapies should be individualized. | B | 11, 12, 14, 15 |
| Progressive eccentric exercises are effective for the treatment of Achilles tendinopathy when combined with relative rest and stretching. | B | 23–26 |
| There is limited evidence that prefabricated silicone inserts and stretching are effective treatments for plantar fasciitis. Tension night splints were shown to be helpful in two clinical trials. | B | 27, 28, 30, 31 |
| To help prevent exercise-associated collapse in long distance runners who overzealously hydrate with hypotonic fluid, runners should be counseled to replace fluid losses judiciously, with a goal of 400 to 800 mL per hour. | C | 41,43 |
CYCLING
If the athlete is a cyclist, it is important to inquire about any recent changes in equipment (including saddle, shoes, or cleats), in position on the bicycle or saddle height, and in training habits or terrain.3 Observation of the athlete on the bicycle (using a trainer stand) is often the single best diagnostic tool. A concise illustrated reference on bicycle fit is available in the medical literature.4
Common Overuse Injuries and Tendinopathies
Endurance athletes alternate periods of intensive physical training with periods of rest and recovery. An imbalance caused by overly intensive training and inadequate recovery leads to a breakdown of cellular reparative mechanisms and eventual tissue breakdown. It has been postulated that subclinical tissue damage may accumulate for some time before an athlete experiences pain or other symptoms.5
Physicians have historically referred to overuse injuries of tendons as “tendinitis,” suggesting that the underlying process is inflammatory. Although acute injury can lead to a true tendinitis (i.e., acute inflammation) or a tenosynovitis (i.e., inflammation of the tendon sheath, manifested clinically as crepitus and pain), it is apparent from histopathologic studies that most overuse tendon injuries are degenerative, not inflammatory.6 Microscopically, there is a notable absence of inflammatory cells. Instead, these tendon injuries are characterized by collagen fiber degeneration and disorganization, an increased number of tenocytes, and an apparent “stalled” healing response.6 These findings have led many researchers to advocate use of the term “tendinopathy” as the preferred generic descriptor of tendon overuse injuries, and they further suggest that the terms “tendinitis” and “tendinosis” (i.e., chronic degeneration) be reserved for precise histopathologic diagnoses.7 The recognition that overuse tendinopathies are degenerative rather than inflammatory has important clinical implications. Many patients with these disorders are slow to recover, often require significant activity modification and rest, and may or may not respond favorably to nonsteroidal anti-inflammatory drugs (NSAIDs) or injected corticosteroids.6
Relative rest is a fundamental component of the treatment of tendinopathy, as well as all other overuse injuries. The duration and extent of rest are dictated by the severity of the symptoms, the nature of the injury, and the sport itself. To maintain fitness while the injury resolves, the athlete generally should avoid activities that are painful and substitute an alternative exercise (e.g., cycling instead of running). A gradual return to sport-specific activity is essential to avoid reexacerbation. Common overuse injuries are summarized in Tables 1 and 2.
| Clinical condition | History | Physical examination | Diagnostic imaging |
|---|---|---|---|
| Patellofemoral pain syndrome |
|
|
|
| Iliotibial band friction syndrome |
|
|
|
| Medial tibial stress syndrome (i.e., shin splints) |
|
|
|
| Achilles tendinopathy |
|
|
|
| Plantar fasciitis |
|
|
|
| Stress fracture |
|
|
|
| Clinical condition | Treatment |
|---|---|
| Patellofemoral pain syndrome | Relative rest and activity modification, icing, NSAIDs, patellar tracking exercise program (straight leg raises and short arc quad isometric exercises) |
| Consider use of knee sleeve or patellar taping (typically initiated by physical therapist) | |
| Cyclists should consider change in seat height, cycling position, or pedal/cleat system | |
| Iliotibial band friction syndrome | Relative rest and activity modification, icing, NSAIDs, Hip abductor strengthening, iliotibial band stretching, occasional need for corticosteroid injection |
| Cyclists should consider change in seat height, cycling position, or pedal/cleat system | |
| Medial tibial stress syndrome (i.e., shin splints) | Relative rest, icing, NSAIDs, stretching |
| Consider use of insoles or orthotics in patients with significant pes cavus or hyperpronation | |
| Achilles tendinopathy | Relative rest, icing, NSAIDs, stretching, heel lifts |
| Short-term walking boot for severe cases | |
| Eccentric strength training is key treatment | |
| Plantar fasciitis | Relative rest, ice massage, NSAIDs, prefabricated shoe inserts, heel cord and plantar fascia stretching, tension night splints, occasional need for corticosteroid injection |
| Stress fracture | Relative rest; additional treatment individualized for specific fractures |
| Metatarsal shaft fractures may be treated with stiff-soled shoe. Fractures of the femoral neck, anterior tibia, tarsals, and proximal fifth metatarsal require more specialized care and consultation |
PATELLOFEMORAL PAIN SYNDROME
Patellofemoral pain syndrome, often referred to as “runner's knee,” is a generic descriptor for anterior knee pain related to a spectrum of patellofemoral joint disorders. Athletes typically describe pain in the anterior knee that is related to repetitive loading of the joint while running, jumping, or cycling; that is aggravated by climbing or descending stairs or hills; and that is aggravated by prolonged sitting with the knees flexed (i.e., “theater sign”). Physical examination may reveal patellofemoral malalignment, tenderness at the patellofemoral facets, pain on patellofemoral compression test, crepitus on active extension, and a positive “J” sign. As with most overuse injuries, modification of the training schedule is useful.8 Cyclists may need to adjust their saddle height, cycling position, or pedal/cleat system.4,9,10 Other potential treatment strategies include rehabilitative exercise with attention to patellar tracking and vastus medialis strengthening,11,12 icing, NSAIDs,13 and taping or the use of orthotic devices (e.g., a rubber sleeve with patellar hole) to address possible patellar maltracking.14,15
ILIOTIBIAL BAND FRICTION SYNDROME
Iliotibial band friction syndrome is the most common cause of lateral knee pain in runners, with an incidence of up to 12 percent of all running-related injuries.16 This overuse injury is the result of microtrauma to the iliotibial band (ITB) as it slides repeatedly over the lateral femoral condyle. Athletes may present with sharp pain or burning at the lateral knee during running, cycling, or hiking. Physical examination reveals tenderness of the ITB overlying the lateral femoral condyle. Weakness in hip abduction may be a causative factor in runners,17 and athletes will often have a tight ITB. Treatment includes activity modification, icing, and NSAIDs, accompanied by a hip abductor strengthening program, ITB stretching, and, rarely, corticosteroid injections in recalcitrant cases.16,17 Cyclists may need to consider changing cycling position, saddle height, or pedal/cleat system.3,18
MEDIAL TIBIAL STRESS SYNDROME
Medial tibial stress syndrome (i.e., shin splints) refers to exercise-related pain at the posteromedial border of the mid- to distal tibia.19 This condition is likely part of a continuum of stress injuries to bone and may represent a periostitis, tibial stress reaction, or tendinopathy along the tibial origin of the tibialis posterior muscle.20 This syndrome is likely related to a variety of predisposing biomechanic issues, including hyperpronation.21 Mild shin splints are associated with pain only during exercise, whereas severe shin splints may cause pain even at rest. The differential diagnosis includes true tibial stress fracture and chronic exertional compartment syndrome.
Physical examination reveals tenderness along several centimeters at the posteromedial border of the tibia, whereas a more focal anterior tibial tenderness suggests a stress fracture. Treatment includes activity modification, stretching, icing, NSAIDs, and attention to biomechanic factors that might be correctable with insoles, orthotics, or antagonistic muscle strengthening, although there is little objective evidence to support these interventions.22
ACHILLES TENDINOPATHY
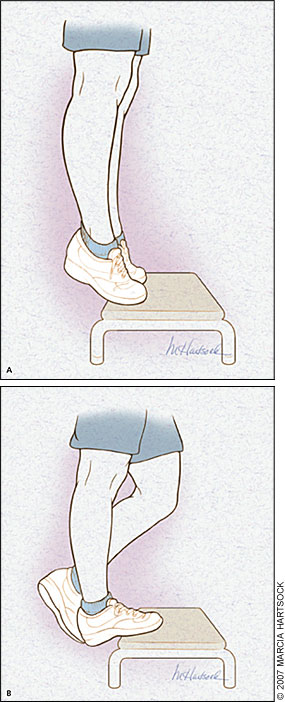
The usual history of Achilles tendinopathy is a gradual and insidious onset of pain in the Achilles tendon. In mild cases, symptoms may be present only during exercise, whereas in more severe cases, the pain will interfere with normal daily activities. Physical examination reveals tenderness several centimeters proximal to the tendon insertion, often with thickening or a palpable nodule. A more acute onset of pain, associated with crepitus on physical examination, suggests a true Achilles tenosynovitis. Although initial treatment may include activity modification, temporary use of a walking boot in severe cases, heel lifts, gentle stretching, icing, and NSAIDs, the most effective treatment is an eccentric strength training program (i.e., lengthening the muscle fibers as a load is applied).23–26 The calf muscles can be strengthened in such a manner by utilizing a stair or step (Figure 1).
PLANTAR FASCIITIS
Plantar fasciitis is thought to result from microscopic tearing of the plantar fascia secondary to traction and overuse. Athletes describe heel or arch pain that often is worse upon the first few steps in the morning or after prolonged sitting. Pes planus and pes cavus have been implicated as predisposing factors. Tenderness is elicited with palpation at the origin of the plantar fascia at the medial plantar calcaneal tubercle. Although there is limited evidence to support these treatments, appropriate strategies include relative rest, heel cord and plantar fascia stretching, icing, NSAIDs, prefabricated shoe inserts to provide arch support, and avoidance of flat shoes or going barefoot.27 In one prospective study, silicone inserts were more helpful than rubber heel cups, and both were more helpful than custom orthotics.28 The current evidence does not support the use of extracorporeal shockwave therapy.29 Tension night splints have been shown to be helpful in two randomized clinical trials but only of equivocal benefit in another.30–32 There is some evidence to support the judicious use of corticosteroid injections.27,33 Surgery with or without calcaneal spur excision should be reserved for patients with refractory symptoms of more than six to 12 months' duration who fail nonoperative treatment.
STRESS FRACTURE
Stress fracture is a common and potentially serious overuse injury in endurance athletes. Stress fracture develops when bone is subjected to repetitive loading (e.g., during running). Microtrauma of the bone accumulates, and bone remodeling cannot keep pace with the continued mechanical stress.5 Stress fracture may occur at the femoral neck, tibia, fibula, calcaneus, talus, tarsal navicular, metatarsals, and sesamoids. Stress fracture should be considered whenever an endurance athlete—particularly a runner—presents with focal musculoskeletal pain.34
Stress fracture is suggested clinically when physical examination reveals significant tenderness over a bony structure. In the case of femoral neck stress fracture, a progressive limp combined with pain on passive range of motion of the hip strongly suggests the diagnosis. Radiography is initially negative in 50 to 75 percent of patients with stress fracture; bone scan imaging or magnetic resonance imaging may reveal the diagnosis if it is not adequately suggested by history and physical examination alone.35 In many cases, stress fractures simply require relative rest and, possibly, short-term use of crutches or a walking boot. Patients with metatarsal fractures may be treated with a postoperative sandal or stiff-soled shoe. Stress fractures of the femoral neck, anterior tibial shaft, tarsals, and proximal fifth metatarsal require more individualized care, and consultation with a sports medicine specialist or orthopedist is usually indicated. Some studies have shown that the use of shock-absorbing inserts in footwear may reduce metatarsal stress fractures.36
Common Medical Conditions in Endurance Athletes
Endurance athletes are susceptible to a number of unique medical problems, all of which are preventable or treatable with appropriate medical intervention (Table 3).
| Clinical condition | Signs and symptoms | Treatment |
|---|---|---|
| Exercise-induced asthma |
|
|
| Exercise-associated collapse and hyponatremia |
|
|
| Overtraining syndrome |
|
|
EXERCISE-INDUCED ASTHMA
Exercise-induced asthma has a reported prevalence of 8 to 12 percent in the general population and may be more common in elite athletes.37 The condition is characterized by acute, reversible bronchospasm that occurs during or after strenuous exercise. Typical symptoms include breathlessness, although coughing or wheezing may occur. Some athletes may only have decreased performance during vigorous endurance training or competition. The more strenuous the effort, the more likely symptoms will occur. Among endurance activities, running is the most likely to precipitate exercise-induced asthma, whereas swimming is least likely and cycling is of intermediate likelihood. Cold, dry air is much more likely than warm, humid air to exacerbate symptoms. Air pollutants are also a contributing factor.38
Exercise-induced asthma is thought to result from the water loss and cooling in the airway that occurs with hyperventilation, and this is thought to secondarily trigger bronchospasm.39 The diagnosis is straightforward in patients with known asthma and in those with a classic history. These patients may be treated initially with an inhaled beta agonist before exercise. In some athletes, an exercise test in the field (preferably in cold, dry air) using a peak expiratory flow meter before and after vigorous, sustained exercise may reveal the diagnosis. Others may require formal laboratory evaluation with a methacholine challenge test.
Athletes with exercise-induced asthma can be highly successful in endurance sports and should be encouraged to continue. Nonpharmacologic strategies that may be helpful include optimization of physical conditioning, adequate warm-up, and induction of a refractory period by briefly precipitating symptoms with short vigorous bursts of exercise 15 to 20 minutes before the endurance activity.39 Pharmacologic therapy with inhaled beta agonists 15 to 20 minutes before exercise is the standard initial treatment in persons with mild symptoms, whereas more persistent cases may require a trial of one or more alternative medications, including cromolyn (Intal), inhaled corticosteroids, long-acting beta agonists, and leukotriene-receptor antagonists.
EXERCISE-ASSOCIATED COLLAPSE AND HYPONATREMIA
Exercise-associated collapse is a dramatic event that is becoming more common with the increased popularity of marathons and triathlons. Most cases are benign and occur after an athlete stops exercising. The most common form of collapse is related to transient hypotension resulting from pooling of blood in the legs after cessation of exercise; it is treated with elevation of the feet and legs.40 More serious causes include hyponatremia, heat-related illness, and cardiovascular events.
Collapse related to hyponatremia is a dilutional phenomenon caused by overvigorous replacement of hypertonic sweat with hypotonic fluids that contain little or no sodium. It is usually encountered in longer endurance events and is more common in women and in slower runners.40,41 Athletes with hyponatremia may gain significant body weight during the event. In contrast with athletes with heat illness, athletes who collapse from hyponatremia are not hyperthermic. Physicians should counsel athletes, particularly inexperienced and slower runners, not to overhydrate during their endurance events. Although commonly published recommendations have suggested 150 to 300 mL of fluid intake at 15- to 20-minute intervals (or approximately 1 L per hour), other experts suggest that it is more appropriate to drink as much as desired but no more than 400 to 800 mL per hour.42,43 This recommendation seems prudent for those participants expecting to require four or more hours to complete a marathon.
OVERTRAINING SYNDROME
Overtraining syndrome is an incompletely understood but well-recognized syndrome in which the athlete's training program overwhelms the body's ability to adapt.44 This condition can be considered a systemic overuse injury. The most notable symptoms from the athlete's perspective are decreased performance and generalized fatigue; other symptoms include mood disturbance, poor sleep, “heavy legs,” and increased rates of illness and injury.45 By definition, these symptoms persist despite more than two weeks of rest. An increased basal heart rate has been classically described as a sign of overtraining syndrome, but recent prospective studies have not confirmed this finding.46 There are no specific serologic markers for overtraining syndrome, but it is customary to exclude other medical causes of fatigue. If an athlete has had baseline exercise testing, a sports-specific exercise test, continued until exhaustion, usually will demonstrate a performance decrement and thus confirm the diagnosis. The treatment is rest for several weeks to months, followed by a gradual resumption of training.