
Am Fam Physician. 2007;76(7):943-947
to the editor: The article, “Common Spider Bites,”1 in the March 15, 2007, issue of American Family Physician, should have been titled “Spider Bites: A Rare Occurrence.”
Spider bites do occur, but they are the exception, not the rule. Overdiagnosis of brown recluse spider bites has led to harmful sequelae and misdiagnosis of other common and uncommon dermonecrotic wounds.2 Many patients currently present with a “spider bite,” but on investigation they have community-acquired methicillin-resistant Staphylococcus aureus (MRSA).
Identification of spiders is difficult and requires an arachnologist; most entomologists cannot properly identify spiders. Just because a spider is brown and has a mark on it does not make it a brown recluse spider. In the United States, brown recluse spiders are endemic only in the Southwest and Midwest.2 Bites from these spiders do not occur outside these areas. Patients and physicians often blame spiders when they did not see what bit them.
to the editor: Although I enjoyed your article on spider bites,1 I wanted to highlight the inclusion of furuncles and boils in your list of differential diagnoses and to suggest that physicians prominently consider community-acquired methicillin-resistant Staphylococcus aureus (MRSA) as the etiologic agent when patients present with a possible spider bite.
In recent years, many patients have presented to my office with the chief concern of a spider bite. After further questioning, I have often found that the patient did not see a spider, but rather a spider bite was assumed because of “how bad it looks.” “A working diagnosis of ‘spider bite’ or publishing a case history should be considered only when a spider is caught in the act of biting or otherwise reliably associated with a lesion.”2 When cultured, my patients' “spider bites” invariably grow out as MRSA.
Vast regions of the country where Loxosceles reclusa (brown recluse spiders) are not present, such as the Pacific Northwest, are many of the same areas where it would be difficult to find a widow spider or a tarantula; this makes the diagnosis of a spider bite highly unlikely.3 It is duly noted that Drs. Diaz and LeBlanc reside in Louisiana and, therefore, practice in an area where venomous spiders are likely to be found; readers should be reminded that this region does not accurately represent the arachnid population of the entire United States.
Although risk factors for community-acquired MRSA include day care attendance, recent incarceration, and contact with an individual with a history of community-acquired MRSA, these factors do not need to be present, and often are not.4–6 The incidence of community-acquired MRSA is on the rise in our community and in many others throughout the country; I urge providers to consider community-acquired MRSA, with its own diagnostic and treatment challenges, when presented with a purported spider bite.
in reply: I greatly appreciate the comments from Drs. Kemerer and Reitz about our recent article on spider bites. I completely agree that spider bites are rare and frequently overdiagnosed, even in communities where the purported biting spiders are not endemic (Figure 11).2 In addition, we are now experiencing an epidemic of skin lesions infected with community-acquired methicillin-resistant Staphylococcus aureus (MRSA), many of which may have originated in pruritic bites and stings, or in other puncture wounds that eventually necrose and can mimic necrotic arachnidism.3 A retrospective, descriptive analysis of 422 patients presenting to U.S. emergency departments with skin and soft-tissue infections, many following insect bites and stings, has now identifiedS. aureus, predominantly community-acquired MRSA, as the most frequently identified causative infectious organism (S. aureus in 320 of 422 cases; prevalence = 76 percent; MRSA prevalence = 59 percent).3
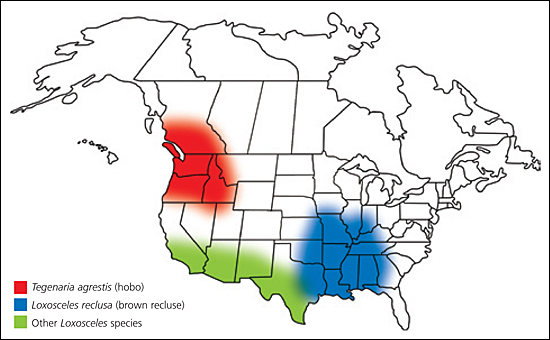
The differential diagnosis of necrotic arachnidism, often incorrectly ascribed to recluse orLoxosceles species spider bites in the United States, is extensive and includes most dermonecrotic lesions, from boils and furuncles to tick bites to topical medication reactions (see related Photo Quiz in the June 15, 2007, issue of American Family Physician4). Two reports have found that the diagnosis of brown recluse(Loxosceles reclusa) bites is widely overused.5,6 In a retrospective analysis of spider bites in the Pacific Northwest from 1988 to 1996, the Centers for Disease Control and Prevention (CDC) reported that a non-native species, Tegenaria agrestis (the hobo spider), introduced into the area from Western Europe in the 1930s, was most likely responsible for an increasing number of unidentified spider bites with extensive dermal necrosis and permanent scarring (Figure 1).1 Hobo spiders, also known as aggressive house spiders, have never been conclusively identified as causes of necrotic arachnidism in the Pacific Northwest because the CDC report was based solely on retrospective telephone reports of suspected bites without expert identification of biting spiders.
In conclusion, the epidemiologic analysis of spider bites is confounded by several factors including: the extensive differential diagnosis of dermonecrotic bite-like lesions, many now infected with community-acquired MRSA; suspected versus definite spider bites; and precise identification of biting spiders by arachnologists.2 To date, most studies of spider bites have been retrospective; bites have not been confirmed by eyewitnesses; and spiders have not been kept alive for later identification, or were identified incorrectly.2 Only prospective studies of definitely confirmed spider bites with expert identification of the envenoming species will contribute to the development of evidence-based methods to precisely describe venomous spiders and the outcomes of their bites.2