
Am Fam Physician. 2008;77(4):453-460
This is part I of a two-part article on chronic shoulder pain. Part II, “Treatment,” appears in this issue of AFP on page 493.
Author disclosure: Nothing to disclose.
Shoulder pain is defined as chronic when it has been present for longer than six months. Common conditions that can result in chronic shoulder pain include rotator cuff disorders, adhesive capsulitis, shoulder instability, and shoulder arthritis. Rotator cuff disorders include tendinopathy, partial tears, and complete tears. A clinical decision rule that is helpful in the diagnosis of rotator cuff tears includes pain with overhead activity, weakness on empty can and external rotation tests, and a positive impingement sign. Adhesive capsulitis can be associated with diabetes and thyroid disorders. Clinical presentation includes diffuse shoulder pain with restricted passive range of motion on examination. Acromioclavicular osteoarthritis presents with superior shoulder pain, acromioclavicular joint tenderness, and a painful cross-body adduction test. In patients who are older than 50 years, glenohumeral osteoarthritis usually presents as gradual pain and loss of motion. In patients younger than 40 years, glenohumeral instability generally presents with a history of dislocation or subluxation events. Positive apprehension and relocation are consistent with the diagnosis. Imaging studies, indicated when diagnosis remains unclear or management would be altered, include plain radiographs, magnetic resonance imaging, ultrasonography, and computed tomography scans. Plain radiographs may help diagnose massive rotator cuff tears, shoulder instability, and shoulder arthritis. Magnetic resonance imaging and ultrasonography are preferred for rotator cuff disorders. For shoulder instability, magnetic resonance imaging arthrogram is preferred over magnetic resonance imaging.
Shoulder pain is responsible for approximately 16 percent of all musculoskeletal complaints,1 with a yearly incidence of 15 new episodes per 1,000 patients seen in the primary care setting.2 Part I of this two-part article will provide the primary care physician with a simple, effective approach to the diagnosis of chronic shoulder disorders such as rotator cuff pathology, adhesive capsulitis, acromioclavicular osteoarthritis, glenohumeral osteoarthritis, and instability. Part II, which appears in this issue of AFP, discusses the treatments of chronic shoulder pain that are consistent with recent evidence-based guidelines.3,4 Shoulder pain is defined as chronic when it has been present for longer than six months, regardless of whether the patient has previously sought treatment. It can be divided into six diagnostic categories: (1) rotator cuff disorders, including tendinosis, full or partial thickness tears, or calcific tendinitis; (2) adhesive capsulitis; (3) glenohumeral osteoarthritis; (4) glenohumeral instability; (5) acromioclavicular joint pathology; and (6) other chronic pain, including less common shoulder problems and non-shoulder problems.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| All patients should receive radiographs as part of the initial work-up for chronic shoulder pain. | C | 23 |
| Further testing of chronic shoulder pain, using imaging*, should be performed when the diagnosis remains unclear or the outcome would change management. | C | 23, 24 |
| If acromioclavicular osteoarthritis is suspected, the acromioclavicular joint should be assessed for tenderness, and a cross-body adduction test should be performed to help confirm the diagnosis. | C | 16, 18 |
| When rotator cuff injury is suspected, assess for night pain and pain with overhead activity. | C | 10 |
| When the patient has a painful shoulder with severely limited active and passive ranges of motion, a diagnosis of adhesive capsulitis should be considered. | C | 8, 9 |
Clinical Diagnosis
MEDICAL HISTORY
Table 15–11 summarizes the history and potentially associated shoulder conditions for patients with chronic shoulder pain. The age of the patient is an important initial consideration. Patients younger than 40 years are more likely to present with shoulder instability or mild rotator cuff disease (impingement, tendinopathy), whereas patients older than 40 years are at an increased risk for advanced, chronic rotator cuff disease (partial or complete tear), adhesive capsulitis, or glenohumeral osteoarthritis.3–5, 12–14
| History | Associated condition |
|---|---|
| Age5,6,7 | If younger than 40 years: instability, rotator cuff tendinopathy |
| If older than 40 years: rotator cuff tears, adhesive capsulitis, glenohumeral osteoarthritis | |
| Diabetes or thyroid disorders8,9 | Adhesive capsulitis |
| History of trauma10 | If younger than 40 years: shoulder dislocation/subluxation |
| If older than 40 years: rotator cuff tears | |
| Loss of range of motion | Adhesive capsulitis, glenohumeral osteoarthritis |
| Night pain10 | Rotator cuff disorders, adhesive capsulitis |
| Numbness, tingling, pain radiating past elbow | Cervical etiology |
| Pain location | Anterior-superior shoulder pain associated with acromioclavicular joint pathology |
| Diffuse shoulder pain in deltoid region associated with rotator cuff disorders, adhesive capsulitis, or glenohumeral osteoarthritis | |
| Pain with overhead activity10 | Rotator cuff disorders |
| Sports participation11 | Shoulder instability associated with overhead sports (e.g., baseball, softball, tennis), and collision sports (e.g., football, hockey) |
| Acromioclavicular joint pathology associated with weight lifting | |
| Weakness | Rotator cuff disorders, glenohumeral osteoarthritis |
The occupational and recreational interests of the patient are also important in the evaluation of shoulder pain. A history of collision sports or weight lifting might make instability or acromioclavicular osteoarthritis more likely, whereas overhead sports or work activities might make rotator cuff pathology more likely.
The location of the pain can be helpful for diagnosis. Anterior-superior pain often can be localized to the acromioclavicular joint, whereas lateral deltoid pain is often correlated with rotator cuff pathology. Neck pain and radiating symptoms should be explored because cervical pathology can mimic shoulder pain. Typically, pain that radiates past the elbow to the hand is not related to shoulder pathology. However, it is not uncommon to have pain that radiates into the neck because the trapezius muscle often spasms in patients with underlying chronic shoulder pathology. The presence of both is more likely to be related to cervical pathology. Dull, achy night pain is often associated with rotator cuff tears or severe glenohumeral osteoarthritis.
Previous treatments and factors that aggravate or alleviate the pain can be important clues to the diagnosis. Night pain from sleeping on the affected shoulder, as well as a history of trauma, has been associated with rotator cuff tears.10 A painful arc, noted by pain with overhead activity, is associated with mild rotator cuff disease and tendinopathy as well as rotator cuff tears.10,15 A history of previous shoulder surgery is important because adhesive capsulitis and glenohumeral osteoarthritis can be early or late complications of surgery.
The patient's medical history, including joint problems, can help to narrow the differential diagnosis. Autoimmune diseases and inflammatory arthritis can affect the shoulder, resulting in erosions and wear in the glenohumeral joint, whereas diabetes and thyroid disorders can be associated with adhesive capsulitis.8,9
PHYSICAL EXAMINATION
| Examination maneuver | Associated condition | Sensitivity (%) | Specificity (%) | LR+ | LR− |
|---|---|---|---|---|---|
| Inspection | |||||
| Supraspinatus or infraspinatus atrophy10 | Chronic rotator cuff tear | 56 | 73 | 2.07 | 0.60 |
| Palpation | |||||
| Acromioclavicular tenderness16 | Acromioclavicular joint OA or chronic sprain | 96 | 10 | 1.07 | 0.4 |
| Range of motion | |||||
| Restrictive active10 | Rotator cuff disorder | 30 | 78 | 1.36 | 0.90 |
| Provocative tests | |||||
| Hawkins' impingement15 | Impingement/rotator cuff disorder | 72 | 66 | 2.1 | 0.42 |
| Drop-arm15 | Large rotator cuff tear | 27 | 88 | 2.25 | 0.83 |
| Empty-can supraspinatus15 | Rotator cuff disorder involving supraspinatus | 44 | 90 | 4.4 | 0.62 |
| Lift-off subscapularis17 | Rotator cuff disorder involving subscapularis | 62 | 100 | > 25 | 0.38 |
| External rotation/infraspinatus strength15 | Rotator cuff disorder involving infraspinatus | 42 | 90 | 4.2 | 0.64 |
| Cross-body adduction18 | Acromioclavicular joint OA or chronic sprain | 77 | 79 | 3.50 | 0.29 |
| Apprehension19 | Glenohumeral instability | 72 | 96 | 20.22 | 0.29 |
| Relocation19 | Glenohumeral instability | 81 | 92 | 10.35 | 0.2 |
Inspection should involve the entire shoulder, with proper exposure of the anterior, lateral, and posterior shoulder. A scar can indicate previous surgery or trauma. The presence of deformity, particularly of the acromioclavicular joint, often indicates an old trauma. Atrophy of the supraspinatus, and less commonly the infraspinatus, may be present with a chronic rotator cuff tear.
Palpation can identify areas of pathology, especially with the acromioclavicular joint. Isolated tenderness that is localized to the acromioclavicular joint is often indicative of acromioclavicular osteoarthritis. Subacromial tenderness may suggest rotator cuff pathology. Multiple trigger points around the shoulder may indicate non-shoulder pathology such as fibromyalgia. It is important to palpate both shoulders because certain structures can be painful (e.g., coracoid process, long head of biceps tendon), even in a healthy shoulder. The presence of a disproportionate amount of discomfort is helpful for diagnosis.
Range of motion should be evaluated in flexion, abduction, internal rotation, and external rotation. If the patient has a full active range of motion, a passive range of motion need not be assessed. Loss of active and passive ranges of motion is the hallmark of adhesive capsulitis, but it also can be found with moderate to severe osteoarthritis of the glenohumeral joint. Loss of an active range of motion, with a relatively preserved passive range of motion, is often present in patients with rotator cuff pathology. Pain with an active range of motion between 60 and 100 degrees of abduction is known as the “painful arc” and is associated with rotator cuff disease.20
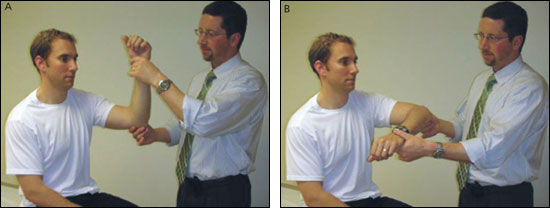
There are numerous provocative tests for the shoulder. Although knowledge of all the tests can be helpful to diagnose pathology, the primary care physician should be familiar with a standard set of tests that should be performed on every shoulder. The Hawkins' test is used to determine impingement (Figures 1a and 1b). Tests for rotator cuff pathology are the drop-arm rotator cuff test (Figures 2a and 2b); the empty-can supraspinatus test (Figure 3); the lift-off subscapularis test (Figure 4); and the external rotation test (Figure 5). The cross-body adduction test (Figure 6) is used to determine symptomatic acromioclavicular joint osteoarthritis, and the apprehension and relocation tests (Figure 7) are used to determine shoulder instability.






CLINICAL DECISION RULES
Clinical decision rules have been developed to determine if a patient has a rotator cuff tear.21 A prospective analysis of 400 patients found that the triad of weakness found with the empty-can supraspinatus and external rotation tests, along with a positive impingement test (e.g., Hawkins' impingement test), had a 98 percent probability of being a rotator cuff tear (partial or complete).5 Patients older than 60 years who had two out of three findings also had a 98 percent probability of a rotator cuff tear. A retrospective analysis of 191 persons found that the combination of being older than 65 years, having weakness on external rotation testing, and experiencing night pain resulted in a 91 percent probability of having a rotator cuff tear (partial or complete).10 However, 54 percent of asymptomatic persons older than 60 years have been shown to have a partial or full thickness rotator cuff tear by magnetic resonance imaging (MRI).22
Diagnostic Imaging
INITIAL IMAGING
Radiographs are indicated as part of the initial work-up for all chronic shoulder pain. The standard series includes anteroposterior, scapular Y, and axillary views. Plain radiographs are the tests of choice to assess osteoarthritis of the acromioclavicular and glenohumeral joints. Secondary signs of a large rotator cuff tear may be observed with superior migration of the humeral head. Cystic changes of the humeral head and sclerosis of the inferior acromion can indicate chronic rotator cuff disease. Plain radiographs can also diagnose calcific tendinitis. A large Hill-Sachs lesion (an indentation into the posterior aspect of the humeral head that occurs when the shoulder dislocates anteriorly and the back of the humeral head contacts the anterior edge of the glenoid) or an avulsion fracture off the inferior glenoid may indicate previous instability.
FURTHER IMAGING
Further testing of chronic shoulder pain should be utilized when the diagnosis remains unclear or the outcome would change management. Imaging options include MRI, arthrography, computed tomography (CT), and ultrasonography. The preferred test for diagnosing rotator cuff disorders is MRI, which can assess rotator cuff tendinopathy, partial tears, and complete tears.23 MRI arthrography has become the preferred test for the imaging of suspected labral pathology that may be found in chronic shoulder instability.24
Ultrasonography is emerging as a cost-effective alternative to MRI, with advantages over MRI23 that include better patient tolerance, dynamic assessment, and improved resolution in the face of previous surgery. Ultrasonography is technician-dependent and, therefore, has not yet gained widespread acceptance. Table 323 summarizes the sensitivity, specificity, and positive and negative likelihood ratios for MRI and ultrasonography in the diagnosis of rotator cuff tears.
| Imaging test | Finding | Sensitivity (%) | Specificity (%) | LR+ | LR− |
|---|---|---|---|---|---|
| MRI | Any rotator cuff tear | 83 | 86 | 4.85 | 0.22 |
| Partial thickness rotator cuff tear | 44 | 90 | 3.99 | 0.66 | |
| Full thickness rotator cuff tear | 89 | 93 | 10.63 | 0.16 | |
| Ultrasonography | Any rotator cuff tear | 80 | 85 | 5.09 | 0.27 |
| Partial thickness rotator cuff tear | 67 | 94 | 8.90 | 0.36 | |
| Full thickness rotator cuff tear | 97 | 96 | 13.16 | 0.16 |
The CT scan is the preferred imaging study for bony disorders of the shoulder, including arthritis with significant erosion; instability with significant bone loss of the humeral head or the glenoid; tumors; and occult fractures. CT arthrography may play a role for patients with suspected rotator cuff tears who cannot undergo an MRI.
Diagnostic Approach
Applying the findings from the patient's history, physical examination, and radiographs should enable the physician to formulate a diagnosis (Table 4). Potential problem diagnoses include patients with more than one underlying problem (such as a rotator cuff tear and symptomatic acromioclavicular osteoarthritis) or a less common cause of the pain. The typical presentations for the most common causes of chronic shoulder pain are discussed below.
| Diagnosis | Findings consistent with diagnosis | Findings inconsistent with diagnosis | Imaging |
|---|---|---|---|
| Acromioclavicular joint osteoarthritis | Pain at acromioclavicular joint; positive cross-body adduction test; may have history of trauma | No pain with palpation at acromioclavicular joint; negative cross-body adduction | Radiography shows osteoarthritis at acromioclavicular joint, some evidence of acromioclavicular separation |
| Adhesive capsulitis | Age older than 40 years; decreased active and passive range of motion; history of diabetes or thyroid disease | Full passive range of motion; no pain with movements | Radiography usually normal |
| Glenohumeral instability | Age usually younger than 40 years; history of subluxation or dislocation, or generalized ligamentous laxity; positive apprehension test | Negative apprehension test | Radiography usually normal |
| Glenohumeral osteoarthritis | Age older than 50 years; progressive pain; crepitus with range of motion | Age younger than 50 years; normal radiography | Radiography shows narrowing of joint space, spurring, and osteophytes |
| Rotator cuff pathology | Age usually older than 40 years; pain with overhead activity; night pain; weakness; positive Hawkins' impingement test; and rotator cuff weakness | No pain with overhead activities; no arm pain; no weakness with lift-off, external rotation, or empty-can tests | Radiography may show humeral head sclerosis or cyst, loss of acromial-humeral interval; acromial spur |
ACROMIOCLAVICULAR OSTEOARTHRITIS
Acromioclavicular joint pathology is usually well localized. A history of an injury to the joint (shoulder separation), heavy weight lifting, tenderness to palpation at the acromioclavicular joint, pain with cross-body adduction testing, extreme internal rotation, and forward flexion are consistent with the diagnosis.3,4,14 Radiographs may be difficult to interpret because most patients have acromioclavicular osteoarthritis by the age of 40 to 50 years.3,4,14 A distal clavicle lysis or an elevated distal clavicle supports the diagnosis, whereas the absence of tenderness to palpation at the acromioclavicular joint is inconsistent with the diagnosis.3,4,14
ADHESIVE CAPSULITIS
Adhesive capsulitis refers to a painful shoulder in which the active and passive ranges of motion are severely limited. Gradual onset of pain and stiffness, loss of motion in all planes with increased pain at the extremes of motion, and a history of diabetes or thyroid disease are consistent with the diagnosis.3,4,14 Radiographs are typically negative, and osteoarthritis on radiography is inconsistent with the diagnosis. A normal range of motion is antithetic to the diagnosis.3,4,14
GLENOHUMERAL INSTABILITY
Glenohumeral instability refers to disorders affecting the capsulolabral complex, including dislocation and subluxation. The patients are usually younger than 40 years and have a history of dislocation or subluxation events, which is often involved with collision or overhead sports.3 A “dead arm,” numbness over the lateral deltoid, and a positive apprehension test are consistent with the diagnosis.20 Examination findings inconsistent with the diagnosis are no history of dislocation or subluxation and a negative apprehension test. Positive radiographs are helpful for diagnosing Hill-Sachs lesion, dislocation, and inferior glenoid avulsion fracture, but are nondiagnostic if negative.
GLENOHUMERAL OSTEOARTHRITIS
Glenohumeral osteoarthritis usually presents as gradual pain and loss of motion in patients older than 50 years.3,4,14 A history of arthritis, previous shoulder surgery, pain, crepitus, and decreased motion is consistent with the diagnosis.3,4,14 Radiographs are diagnostic. Normal radiographs and a normal range of motion are inconsistent with the diagnosis.
ROTATOR CUFF PATHOLOGY
Rotator cuff disorders that affect the function of the rotator cuff include a partial or complete tear, tendinitis or tendinosis, and calcific tendinitis. Initially, it is more important to differentiate this group of disorders from the other groups than it is to identify the specific diagnosis. Typically, the patients are older than 40 years and complain of pain in the lateral aspect of the arm with radiation no farther than the elbow. Weakness, a painful arc of motion, night pain, and a positive impingement sign are components of the history and physical examination that are consistent with this diagnosis.14 Findings that are inconsistent with this diagnosis include being younger than 30 years, having no weakness, and presenting no impingement signs. Positive radiographs can be helpful to diagnose calcific tendinitis, acromial spur, humeral head cysts, or superior migration of the humeral head, but are typically normal.3,4,14
OTHER CONDITIONS
Numerous other problems that can affect the shoulder are somewhat less common, such as biceps and labral pathology (e.g., SLAP tear—superior labrum anterior to posterior tear—an avulsion injury to the root of the long head of the biceps tendon) and multidirectional instability. Other conditions are extremely uncommon, such as a suprascapular nerve injury, Parsonage Turner syndrome (brachial plexus neuritis), and a neuropathic shoulder from syringomyelia. The shoulder can also be the area of perceived pain for many non-shoulder problems, including fibromyalgia, cervical radiculopathy, and thoracic outlet syndrome. Fibromyalgia is notable for classic areas of tender points. Cervical radiculopathy pain is generally posterior, with radiation to the neck and down the arm below the elbow. Thoracic outlet syndrome, like cervical radiculopathy, is notable for symptoms that extend past the elbow and often into the hand. There can be neurologic or vascular symptoms based on the subtype. Positive radiographs are helpful for diagnosing severe cervical osteoarthritis, but are typically negative. Positive provocative shoulder testing (e.g., Hawkins' impingement test, empty-can test, external rotation test) that disappears after a subacromial lidocaine (Xylocaine) injection is inconsistent with the diagnosis of fibromyalgia, cervical radiculopathy, or thoracic outlet syndrome.3,4,14