
Am Fam Physician. 2008;78(8):981-983
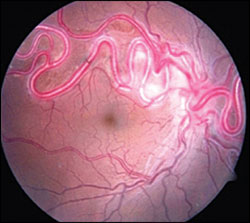
A 39-year-old woman presented with a 10-year history of impaired vision in her right eye. Her best corrected visual acuity was 20/50 and 20/20 in the right and left eyes, respectively. Ophthalmic examination revealed a moderate nuclear sclerotic cataract in her right eye. Ophthalmoscopic findings included multiple dilated, tortuous vessels emerging from the right optic disc, affecting the nasal and superotemporal retina (see accompanying figure). No retinal thickening, exudates, hemorrhages, or relative afferent pupillary defects were noted. Findings in the left eye were normal. Magnetic resonance imaging of the brain and orbits was also unremarkable.
Question
Discussion
The answer is C: retinal arteriovenous malformation (AVM). A retinal AVM is a rare, unilateral developmental anomaly.1 The presentation ranges from subtle arteriovenous communications that are scarcely visible on retinal examination to pronounced dilation of the entire retinal vascular system, in which identification of arterial and venous components is difficult because of arterialization of the involved veins. Retinal AVMs are often detected during a routine eye examination, and usually do not cause visual impairment. Men and women are affected equally. It is most common in the papillomacular area and the superotemporal retina.2 Single or multiple vascular anomalies may be present in the fundus. Retinal AVMs are classified into three groups (Table 1), depending on the presence or absence of the intervening vascular system, the caliber of the connecting vessel, and the number and location of the malformations within the retina.3
| Variant | Characteristics | Associations |
|---|---|---|
| I | Localized, well-compensated, intervening arteriolar or abnormal capillary plexus between the communicating vessels | Ocular or systemic malformations unusual |
| II | Direct arteriovenous malformation without intervening vascular components that may decompensate, leading to leakage of fluid (from slight leakage to extensive retinal edema, exudates, and hemorrhages) | Usually not associated with intracranial vascular malformations |
| III | Large and diffuse anastomosing channels, leading to difficulty in recognizing arterial and venous components; degenerative changes in the retina and poor vision | Intracranial involvement more likely than with other variants |
Retinal AVMs have been associated with intracranial1 and central nervous system (CNS)4 AVMs. A congenital vascular abnormality in which AVMs of the visual pathway, face, and CNS coexist is called Wyburn-Mason syndrome; however, involvement of all three systems is not required for the diagnosis.5,6 Visceral and skeletal anomalies have also been reported in patients with Wyburn-Mason syndrome.1,2 Ophthalmic manifestations such as the characteristic retinal picture of dilated, tortuous, and convoluted AVMs; visual impairment; and proptosis may suggest the presence of the syndrome.
Visual impairment in patients with retinal AVMs is usually caused by cystic degeneration in the retina, macular edema, macular hemorrhage, retinal venous occlusive disease, retinal ischemia, neovascular glaucoma from the isolated retinal AVM,2,7 or AVMs in the visual pathway.5 AVMs typically occur in the midbrain, and neurologic manifestations (e.g., cerebral or subarachnoid hemorrhage) depend on the size and location of the malformations. Patients may present with signs of a midbrain lesion, hemiparesis or hemiplegia, cerebellar dysfunction, or hydrocephalus; intellectual disturbances have also been reported.8 Seizures occur in only 5 percent of patients with retinal AVMs.9 Facial or oral vascular nevi1 and angiomas of the mandible, maxilla, palate, pharynx, and buccal mucosa may occur.9
Retinal AVMs usually are not treated because most are static. Laser therapy may be considered in patients with retinal edema and hard exudates in the fovea. Because of the potential for intracranial involvement, magnetic resonance imaging of the brain and orbit should be performed in patients with retinal AVMs. Neurosurgical consultation may be warranted if an intracranial AVM is identified; however, those AVMs are often inoperable because of their location deep in the midbrain. Embolization may be effective in some patients.
Congenital retinal macrovessel is a rare condition in which a large aberrant blood vessel extends into the macula. Vision usually is not affected unless hemorrhage or foveolar cysts occur.
Congenital vascular tortuosity is benign and may occur in retinal arterioles. The condition tends to worsen with age.
Retinal capillary hemangiomas are well-circumscribed, pinkish lesions supplied and drained by prominent, dilated retinal blood vessels. If untreated, the condition may lead to intraretinal exudates and retinal detachment.
Retinal cavernous hemangiomas are congenital vascular hamartomas comprised of multiple venous aneurysms. They appear as globular, reddish-blue lesions and usually do not require treatment.
| Condition | Characteristics |
|---|---|
| Congenital retinal macrovessel | Enlarged aberrant branch of a retinal artery or vein; may cross horizontal raphe; supplies or drains the macula; capillary bed usually is normal |
| Congenital vascular tortuosity | Benign condition affecting the arterioles; autosomal dominant inheritance; tends to worsen with age |
| Retinal arteriovenous malformation | Uniformly large, dilated, and tortuous retinal arteries and veins with arteriovenous communications |
| Retinal capillary hemangioma | Well-circumscribed, pinkish retinal lesion; supplied by a dilated arteriole and drained by a dilated venule, usually in the periphery; progressive; if untreated, intraretinal exudates and retinal detachment are possible |
| Retinal cavernous hemangioma | Cluster of intraretinal venous aneurysms; globular, reddish-blue lesion located along a retinal vein that often resembles a cluster of grapes; no feeding artery |