
Am Fam Physician. 2009;80(11):1289-1290
Author disclosure: Nothing to disclose.
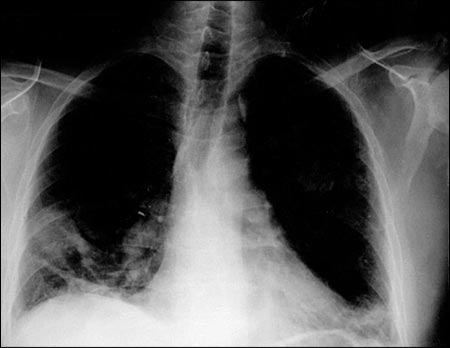
A 53-year-old man presented to the emergency department with dyspnea and a nonproductive cough. He had undergone an ophthalmologic procedure two months prior. Six weeks after surgery, he developed the nonproductive cough with pleuritic chest pain localized to his anterior right chest. Chest radiography was performed (see accompanying figure), and he was treated with a seven-day course of levofloxacin (Levaquin), azithromycin (Zithromax), and anti-inflammatory agents. After initial moderate improvement, his symptoms worsened.
On examination, he had a body temperature of 100° F (37.8° C), heart rate of 103 beats per minute, respiratory rate of 20 breaths per minute, and oxygen saturation of 92 percent. His pulmonary examination showed decreased breath sounds, decreased tactile fremitus, dullness to percussion, and egophony in the right basilar area. Testing of his arterial blood gases showed a pH of 7.46, partial pressure of carbon dioxide of 35.7, and partial pressure of oxygen of 63.2.
Question
Discussion
The correct answer is D: pulmonary embolism. The patient's radiograph shows a focal opacity in the right lung, which is a classic presentation of the lung infarction caused by a pulmonary embolism (Hampton hump). A timely diagnosis is important because the overall risk of mortality in persons with untreated pulmonary embolism is 30 percent, compared with 2 to 8 percent in treated patients.1 Diagnosis requires a high clinical suspicion in a patient with risk factors.
A Hampton hump appears as a wedge-shaped infarction in a segment of the lung that is in contact with the pleural surface.1 Additional radiographic signs of a pulmonary embolus include the Westermark sign (area of focal decreased blood) and Palla sign (enlarged pulmonary artery). These signs are rarely noted, however, and the primary value of chest radiography is exclusion of other diagnoses. Although radiography in patients with pulmonary embolism may be unremarkable, common findings include cardiac enlargement, elevated hemi-diaphragm, and pleural effusion.2,3
Symptoms of a pulmonary embolism are often nonspecific. Dyspnea, pleuritic pain, and cough are the most common presenting symptoms.4 Other common symptoms include hemoptysis, syncope, palpitations, apprehension, and sweating. Classic signs of pulmonary embolism are tachycardia, tachypnea, and a fever greater than 100° F.4 Other common signs include rales, lower extremity edema, heart murmur, and a loud second heart sound. Arterial blood gas testing may show respiratory alkalosis and hypoxemia in spite of hyperventilation. Pulmonary angiography is the first-line diagnostic test. However, the less invasive computed tomography angiography has become a common mode of emergency diagnosis and has a positive predictive value of 96 percent.5
Adenocarcinoma appears as a density of any shape on radiography, usually without calcification.
The patient's radiography findings may be consistent with pneumonia; however, the patient did not respond to antibiotics and had risk factors for pulmonary embolism.
Pulmonary abscess commonly appears as cavitation, which may contain air-fluid levels.
Although the patient recently had eye surgery, episcleritis, scleritis, conjunctivitis, and uveitis are the typical ocular manifestations of Wegener granulomatosis. Lesions associated with the condition are coin-shaped.
| Condition | Radiography findings |
|---|---|
| Adenocarcinoma | Density of any shape, usually without calcification |
| Pneumonia | Tissue consolidation confined by the pleural borders |
| Pulmonary abscess | Lung cavitation, which may contain an air-fluid level |
| Pulmonary embolism | Wedge-shaped opacity of the lung tissue |
| Wegener granulomatosis | Multiple, bilateral, nodular cavitary infiltrates; coin-shaped lesions |