
Am Fam Physician. 2011;83(6):755-756
Author disclosure: Nothing to disclose.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Navy Medical Dept. or the U.S. Navy Service at large.
The authors thank Avery Bevin, MD, Robert Sidbury, MD, and Greg Patterson for their assistance in the preparation of the manuscript.
A male infant was born via uncomplicated vaginal delivery at 42 weeks' gestation after a normal pregnancy. Linear, skin-colored plaques were noted at birth (Figures 1 and 2). The plaques followed the embryologic clonal expansion lines (Blaschko lines) and were most prominent on the left hand, arm, axilla, and trunk.
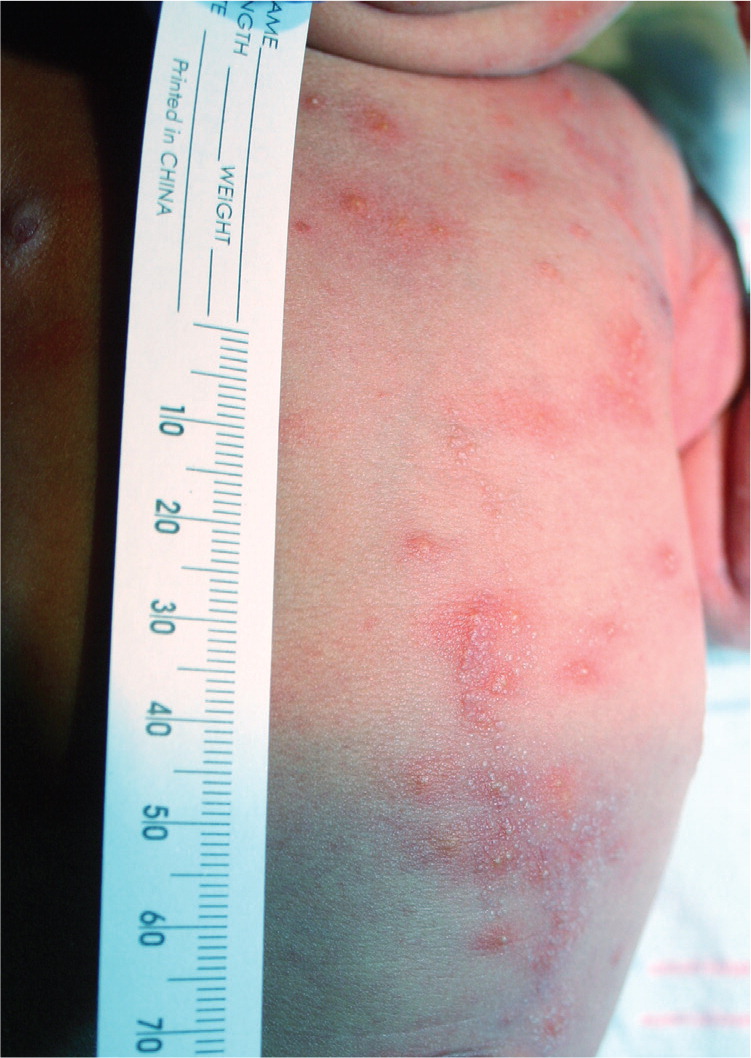

The child was large for gestational age, but physical examination findings were otherwise normal. Two days after birth, a vesicular component developed more diffusely. Results of a Tzanck smear and complete blood count with differential were normal. The vesicles resolved by one week of age, with the lesions returning to their original state.
Question
Discussion
The correct answer is A: epidermal nevi. Epidermal nevi are hamartomatous proliferations of the epidermis and papillary dermis, thought to originate from pluripotent cells in the basal layer of the embryonic epidermis. The condition includes verrucous, sebaceous, pilosebaceous, and eccrine subtypes. Epidermal nevi occur in one out of 1,000 live births, and 80 percent of cases appear in the first year of life.1,2 The nevi are generally unilateral, following Blaschko lines in linear configurations on the limbs. The condition can be associated with syndromes that manifest with developmental abnormalities of the nervous, cardiovascular, urogenital, or skeletal systems. Children born with more extensive lesions should be monitored closely early in life. Treatment consists of full-thickness surgical excision or ablation. Topical treatments, such as steroids, retinoids, tars, and fluorouracil, have only limited benefit.
Incontinentia pigmenti is an X-linked dominant disease and is often fatal in male fetuses. It almost always occurs in female infants and is associated with cutaneous lesions that appear in four phases: vesicular, verrucous, hyperpigmented, and atrophic.3 Lesions appear in the first three weeks of life and follow Blaschko lines. During the vesicular phase, the rash is predominantly located on the lower extremities, and histology demonstrates eosinophilic spongiosis. The condition is often associated with extracutaneous findings, including dental, central nervous system, and ocular abnormalities. Infants with incontinentia pigmenti require baseline ophthalmologic examination, and periodic dental and neurodevelopmental evaluation.
Infantile acropustulosis typically occurs between three and six months of age, and occasionally at birth. It is associated with recurrent crops of pruritic vesicopustular lesions, primarily on the palms and soles. The condition can be misdiagnosed as scabies infection. The lesions begin as pinpoint papules, progressing into vesicles over the course of a day, and then disappear in a variable amount of time. Recurrences usually stop around three or four years of age.
Neonatal herpes simplex virus (HSV) is usually transmitted during vaginal birth, presenting as a vesicular rash on the face or scalp in the first seven to 10 days of life.4 Lesions that appear in the first 24 hours of life suggest an in utero infection, which more often causes erosions than vesicles. Tzanck smear has 79 percent sensitivity and 100 percent specificity for the diagnosis of HSV infection.5 Cultures of skin lesions, nasopharynx, eyes, and cerebrospinal fluid should be obtained, as well as polymerase chain reaction testing if available. Disseminated neonatal HSV infection may not lead to skin lesions and has a 57 percent mortality rate.6
| Condition | Characteristics |
|---|---|
| Epidermal nevi | Lesions are generally unilateral, following Blaschko lines in a linear configuration; may be related to developmental abnormalities |
| Incontinentia pigmenti | X-linked dominant disease almost always occurring in female infants, usually in the first three weeks of life; lesions follow Blaschko lines; associated with dental, central nervous system, and ocular abnormalities |
| Infantile acropustulosis | Recurrent crops of pruritic vesicopustular lesions that usually resolve by three or four years of age; lesions primarily appear on the palms and soles and look similar to scabies |
| Lichen striatus | Rare, idiopathic linear eruption on the extremities that are self-limited and sometimes pruritic; lesions appear between four months and 15 years of age, usually in girls; associated with atopic dermatitis |
| Linear psoriasis | Erythematous, scaly papules and plaques; linear distribution; typically occur on the extremities |
| Neonatal herpes simplex virus infection | Vesicular rash often appears on the face or scalp in first seven to 10 days of life; usually transmitted during vaginal birth; risk of disseminated infection |
