
Am Fam Physician. 2012;85(5):447-454
A more recent article on pain management in labor is available.
Patient information: See related handout on options for managing pain during labor, written by the authors of this article.
Author disclosure: No relevant financial affiliations to disclose.
Regional analgesia has become the most common method of pain relief used during labor in the United States. Epidural and spinal analgesia are two types of regional analgesia. With epidural analgesia, an indwelling catheter is directed into the epidural space, and the patient receives a continuous infusion or multiple injections of local anesthetic. Spinal injections are usually single injections into the intrathecal space. A combination of epidural and spinal analgesia, known as a walking epidural, also is available. This technique combines the rapid pain relief from the spinal regional block with the constant and consistent effects from the epidural block. It allows sufficient motor function for patients to ambulate. Complications with regional analgesia are uncommon, but may include postdural puncture headache. Rare serious complications include neurologic injury, epidural hematoma, or deep epidural infection. Regional analgesia increases the risk of instrument-assisted vaginal delivery, and family physicians should understand the contraindications and risks of complications. Continuous labor support (e.g., doula), systemic opioid analgesia, pudendal blocks, water immersion, sterile water injections into the lumbosacral spine, self-taught hypnosis, and acupuncture are other options for pain management during labor.
Pain management is a universal concern for women during labor. A woman's confidence in her ability to cope with labor best predicts pain perception during the first stage of labor.1 Pain relief plays only a limited role in overall maternal satisfaction with the childbirth experience.2 The relationship between the patient and the physician, and being more involved in decision making improve maternal satisfaction.2,3 Therefore, physicians should talk with patients about labor analgesia options, concerns, and birth experience expectations throughout the prenatal period.
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Regional analgesia provides better pain relief than opioid analgesia, but increases the risk of vacuum- or forceps-assisted vaginal delivery. | A | 7 | Meta-analysis |
| Early use of regional analgesia does not increase the duration of labor or the likelihood of cesarean delivery in near-term to term nulliparous patients undergoing induced labor. | B | 22 | Single randomized controlled trial |
| Continuous support during labor increases the likelihood of a spontaneous vaginal birth and has no identifiable adverse effects. | A | 6 | Meta-analysis |
| Women receiving continuous labor support have been shown to be more satisfied with their childbirth experience and less likely to receive intrapartum analgesia. | A | 6 | Meta-analysis |
Analgesia refers to the relief of pain without the loss of consciousness. Modalities of analgesia during childbirth include regional analgesia, systemic opioid analgesia, continuous labor support, pudendal blocks, immersion in water during the first stage of labor, sterile water injections in the lumbosacral spine, hypnosis, and acupuncture (Table 1).4–11
| Method | Example | When to use | Contraindications | Potential complications | Evidence supporting method? | Caveats |
|---|---|---|---|---|---|---|
| Acupuncture or acupressure | Multiple anatomic sites have been studied with varying protocols | First stage of labor | None | None | Limited4,5 | More research needed |
| Continuous labor support | Doula | All stages of labor | None | None | Yes6 | — |
| Epidural analgesia | 16- to 18-gauge needle into epidural space, catheter inserted through needle, and the needle is removed | First and second stages of labor | Coagulopathy, skin infection at injection site, hypovolemia | Hypotension, allergy to local anesthetics, high spinal or total spinal anesthesia, paralysis, nerve injury, spinal headache, back pain, fever, increase in instrument-assisted vaginal delivery rates | Yes7,8 | Combined spinal-epidural technique allows patients to ambulate during labor |
| Pudendal block | 5 to 10 mL of 1% lidocaine (Xylocaine) using Iowa trumpet and 20-gauge needle | Late first stage through perineal repair to alleviate pain radiated to sacral nerves | None | Monitor local anesthetic toxicity, especially in combination with perineal and labial infiltration | Yes9 | Large vessels proximal to injection site; important to aspirate before injecting |
| Spinal analgesia | 25 to 50 mg of hyperbaric lidocaine into subarachnoid space with 24- to 27-gauge needle | First and second stages of labor | Coagulopathy, skin infection at injection site, hypovolemia | Hypotension, allergy to medications used, increase in instrument-assisted vaginal delivery rates | Yes7,8 | Fentanyl (Duragesic; 10 to 25 mcg) may be added as a spinal anesthetic, often used in combination with epidural analgesia |
| Sterile water injections | 0.1 mL of sterile water with a 25-gauge needle | First stage of labor, or if patient has prominent back pain | None | None | Limited; decreased pain reported after injection but no overall decrease in use of other pain relieving methods4,10 | Effectiveness limited to two hours |
| Systemic opioid analgesia | Butorphanol | First stage of labor | Based on the patient and the medication used | Nausea, respiratory depression, decreased variability, neonatal depression, hypoventilation | Yes | Varying routes of administration (e.g., intramuscular, intravenous) |
| Fentanyl | ||||||
| Nalbuphine | All cross the placenta | |||||
| Water baths | Water immersion | Active labor | Active infections | None | Yes4,11 | Must maintain OSHA infection transmission standards in hospitals |
| Temperature of water above body temperature |
Regional Analgesia
Since 2000, regional analgesia has become the most widely used analgesia for labor pain in the United States.12 Regional analgesia leads to reversible loss of pain over an affected area by blocking the afferent conduction of its innervations with a local anesthetic agent. Epidural and spinal analgesia are two types of regional analgesia used to diminish labor pain. With epidural analgesia, an indwelling catheter is directed into the epidural space, and the patient receives a continuous infusion or multiple injections of local anesthetic. Unlike epidural injections, spinal injections usually are single injections into the intrathecal space. The epidural potential space is relatively large and requires more anesthetic volume than a spinal injection.
The onset of action of spinal analgesia is almost instantaneous, and one dose of medication can provide pain relief for several hours. Conversely, epidural analgesia requires at least 15 minutes until the patient's perception of pain is diminished. Spinal injections need to be placed below L1–L2, otherwise the spinal cord can be injured. Also, traditional spinal injections are more likely to affect motor as well as sensory fibers, which can limit the woman's participation in the second stage of labor.
Regional analgesia in laboring patients increases the risk of vacuum- or forceps-assisted vaginal delivery (relative risk [RR] = 1.42; 95% confidence interval [CI], 1.28 to 1.57; 23 trials; n = 7,935).7 Some physicians try to reduce this risk by discontinuing epidural analgesia late in the second stage of labor. However, a meta-analysis found no statistical reduction in instrumental vaginal deliveries with this method.13 Discontinuing epidural analgesia late in the second stage resulted in inadequate pain relief for 22 percent of study participants versus 6 percent of participants reporting inadequate pain relief when the epidural was continued throughout the second stage of labor (P < .05).13
Multiple randomized controlled trials (RCTs) have examined the effects of regional analgesia on other delivery outcomes. When comparing regional analgesia with no analgesia in a meta-analysis, no statistically significant impact was found in the risk of cesarean delivery, maternal satisfaction with pain relief, long-term backache, or immediate effect on neonatal status as determined by Apgar scores.7 The effect of epidural analgesia on long-term neonatal outcome needs further study but appears to be safer than the use of opioids.7,14
COMBINATION REGIONAL ANALGESIA
Numerous centers now use a combination of epidural and spinal analgesia to provide pain control15 (Figure 1). This combination often is referred to as a walking epidural. This technique combines the positive effects of rapid pain relief from the spinal regional block with the constant and consistent effects from the epidural block. This technique also allows sufficient motor function for patients to ambulate. Combined spinal-epidural analgesia is usually composed of low-dose opioids (e.g., fentanyl [Duragesic]) in combination with a lower-than-usual dose of local anesthetic (e.g., bupivacaine [Marcaine], ropivacaine [Naropin]). The opioids affect the pain receptors without markedly affecting the motor neurons. The combined technique reduces the need for instrumental vaginal deliveries (absolute risk reduction = 8.6 percent; number needed to treat = 12); however, it may increase the likelihood that a newborn needs resuscitation (absolute risk increase = 1.6 percent; number needed to harm = 63).14
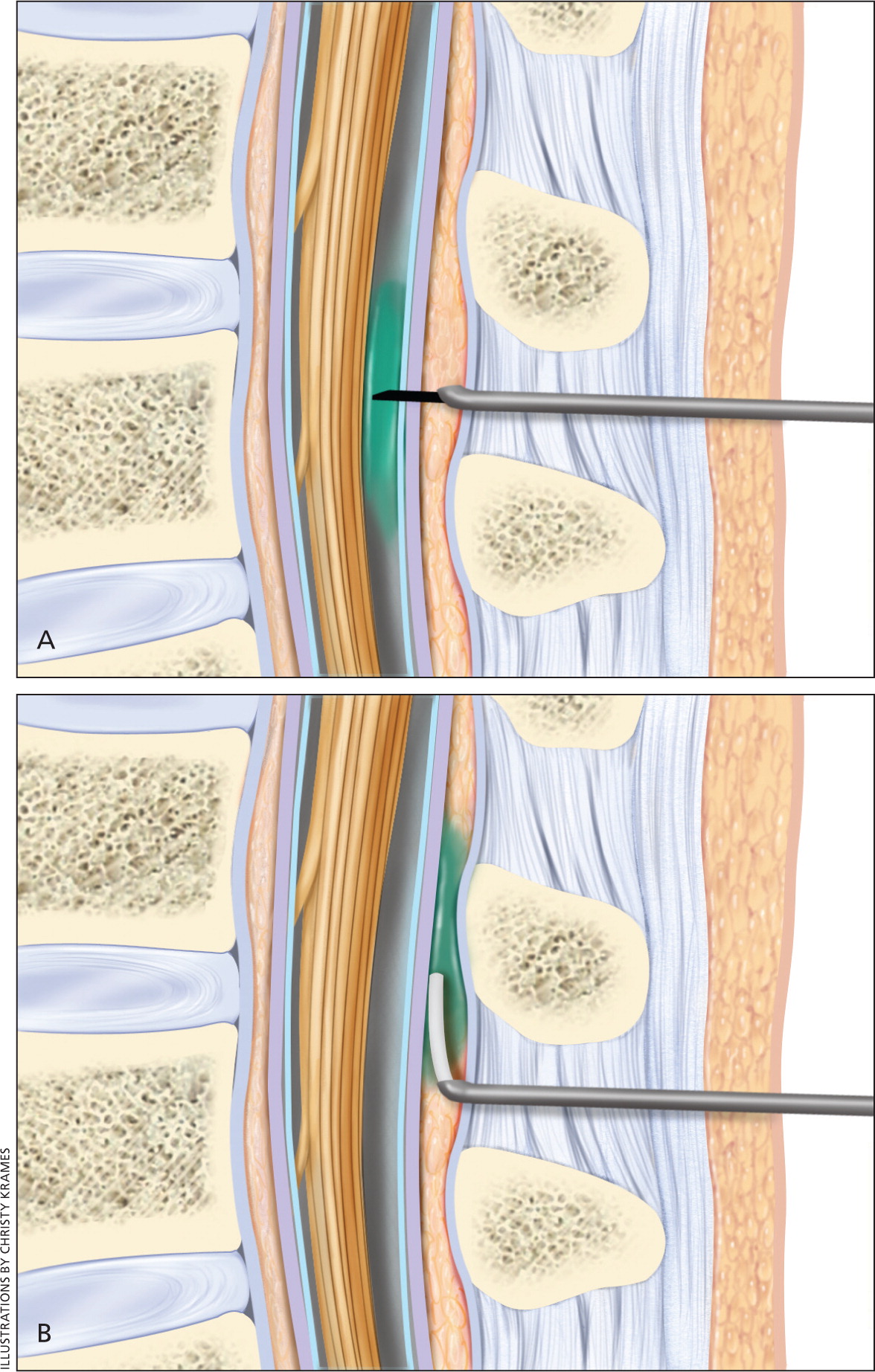
Labor progress and outcome are similar among women receiving combined analgesia or epidural analgesia. The combined technique is not associated with an increased risk of anesthetic complications, and no differences in obstetric or long-term neonatal outcomes can be explained by choice of anesthetic technique. Both techniques can safely provide effective labor analgesia.14
PATIENT-CONTROLLED ANALGESIA
Some institutions allow patients to adjust their medication with a patient-controlled analgesia pump. This technique may decrease the overall amount of local analgesia and opioid used. In some studies, rescue doses of medication were used more often in usual epidural techniques compared with low-dose combination regimens.8
POTENTIAL COMPLICATIONS
Understanding the contraindications, risks, and treatments for potential complications with regional analgesia is essential. Absolute contraindications to spinal analgesia include patient refusal, infection at the site of injection, hypovolemia, indeterminate neurologic disease, coagulopathy, and increased intracranial pressure (except in cases of pseudotumor cerebri). Relative contraindications include sepsis distinct from the anatomic site of puncture (e.g., chorioamnionitis, lower extremity infection).
Absolute contraindications to regional analgesia are rare, but hypotension, which occurs in 15 to 33 percent of patients, is a common risk of regional analgesia.16 Initially, after receiving an epidural or spinal block, eliminating painful stimuli and the onset of peripheral vasodilation may reduce maternal blood pressure. A limited decrease in maternal blood pressure of a healthy patient typically is benign. However, severe hypotension may reduce uteroplacental blood flow, which could limit perfusion in a fetus already struggling to maintain oxygenation.17 Preloading (i.e., administering 500 to 1,000 mL of a crystalloid solution before traditional high-dose local epidural analgesia) may have some beneficial fetal and maternal effects in healthy women by decreasing hypotension (RR = 0.07; 95% CI, 0.01 to 0.53).18
Research does not support the benefit of preloading in low-dose epidural or combined spinal-epidural regional analgesia in labor.18 Therefore, physicians must understand the medications, dosages, and routes of administration at their local institution. Physicians should continue to treat hypotension related to regional analgesia with additional intravenous boluses of crystalloid solution or administration of small intravenous doses of a vasopressor (e.g., 5 to 10 mg of ephedrine).
Epidural or spinal complications are uncommon, but a postdural puncture headache is the most common complication following either procedure. Because most physicians now use fine spinal needles, these headaches have become less common. Patients usually describe headache symptoms that worsen after sitting or standing from a recumbent position. Most spinal or epidural headaches (usually caused by accidental dural puncture) will present within the first 24 hours after the procedure, and can be managed by watchful waiting until the headache resolves. If the headache does not resolve, an autologous epidural blood patch usually provides relief. This consists of a small amount of the patient's blood injected into the epidural space near the original puncture site to produce a clot, blocking the meningeal leak.17
Although infrequent, serious complications may occur from placement of regional analgesia. These may include persistent or transient neurologic injury, epidural hematoma, or deep epidural infections. Transient postpartum paresthesias, motor dysfunction, and epidural infections occur in less than 1 percent of procedures. Physicians can minimize these risks by performing the procedure with sterile technique and by first administering a test dose of lidocaine (Xylocaine) and epinephrine to detect intravenous or subarachnoid placement of the catheter.19,20
Systemic Opioid Analgesia
Systemic opioid analgesia is a commonly used adjunct with subsequent initiation of regional analgesia or an independent method of pain control used early in the first stage of labor. However, repeated maternal administration of opioids results in considerable fetal exposure and increases the potential for neonatal respiratory depression. Patient-controlled analgesia with synthetic opioids such as fentanyl, alfentanil (Alfenta), and the new ultra-short–acting remifentanil (Ultiva) may be used for labor analgesia.21
One RCT demonstrated that early epidural analgesia (i.e., before the onset of labor) resulted in better pain control than systemic opioid analgesia during induction of labor (a score of 2 versus 6 on a 0-to-10 scale; P < .001). This finding was evident in nulliparous women admitted for induction of labor at more than 36 weeks' gestation with intact membranes and cervical dilation of less than 4 cm.22 Cesarean delivery rates were similar between the group receiving early epidural analgesia and the group receiving systemic opioid analgesia (33 versus 32 percent, respectively). Duration of labor was slightly shorter in the early epidural analgesia group (median: 528 versus 569 minutes). There were no differences in mode of vaginal delivery or in newborn Apgar scores.22
Early use of regional analgesia decreased the use of sedatives and systemic opioids, leading to less neonatal exposure and subsequently less risk of neonatal depression.22 These results challenge the widely held notion that early regional analgesia increases the duration of labor and likelihood of cesarean delivery in near-term to term nulliparous patients undergoing induced labor. Because the results are from a single RCT, more research is needed.
Other Approaches to Analgesia
Women with short labors, black women, older women without private insurance, and women with no prenatal care are more likely to decline regional analgesia.23 Some patients decline analgesia altogether to undergo a natural birth experience. Whatever the reason, it is important for physicians to become acquainted with other forms of analgesia in labor. Studies have shown that continuous labor support, pudendal blocks, water immersion, sterile water injections into the lumbosacral spine, self-taught hypnosis, and acupuncture also relieve pain during labor.
CONTINUOUS LABOR SUPPORT
Continuous support during labor, such as from a doula, increases the likelihood of a spontaneous vaginal birth and has no identifiable adverse effects.6 A Cochrane analysis found that women who received continuous labor support were less likely to report dissatisfaction with or give a negative rating of the childbirth experience (six trials; n = 9,824; RR = 0.73; 95% CI, 0.65 to 0.83), and also were less likely to receive intrapartum analgesia (12 trials; n = 11,651; RR = 0.89; 95% CI, 0.82 to 0.96).6 In general, the beneficial effects were greater when the support provider was not a member of the hospital staff, when intrapartum analgesia began early in labor, and when epidural analgesia was not routinely available. Anxiety and fear of pain correlate with a higher reported experience of pain, and continuous labor support remains an effective form of pain relief.3,24
PUDENDAL BLOCK
A pudendal block may be used for analgesia in the late stages of labor. The block may provide pain relief of the vaginal introitus and the perineum, but provides no relief from the pain of contractions. Because it is given close to the time of delivery, there is often little systemic absorption. Large doses of anesthetic that may be required have the potential for local anesthetic toxicity, and there is also the potential for hematoma or abscess formation.
The pudendal block is performed via a transvaginal approach where an Iowa trumpet is used to inject approximately 5 to 10 mL of local anesthetic into the pudendal canals bilaterally 25 (Figure 2). The procedure is relatively simple and may provide up to one hour of pain relief. Lidocaine 1% and chloroprocaine 2% (Nesacaine) are the most commonly used agents. To avoid the risk of intravascular injection, aspiration of the syringe should occur before injecting the local anesthetic.26
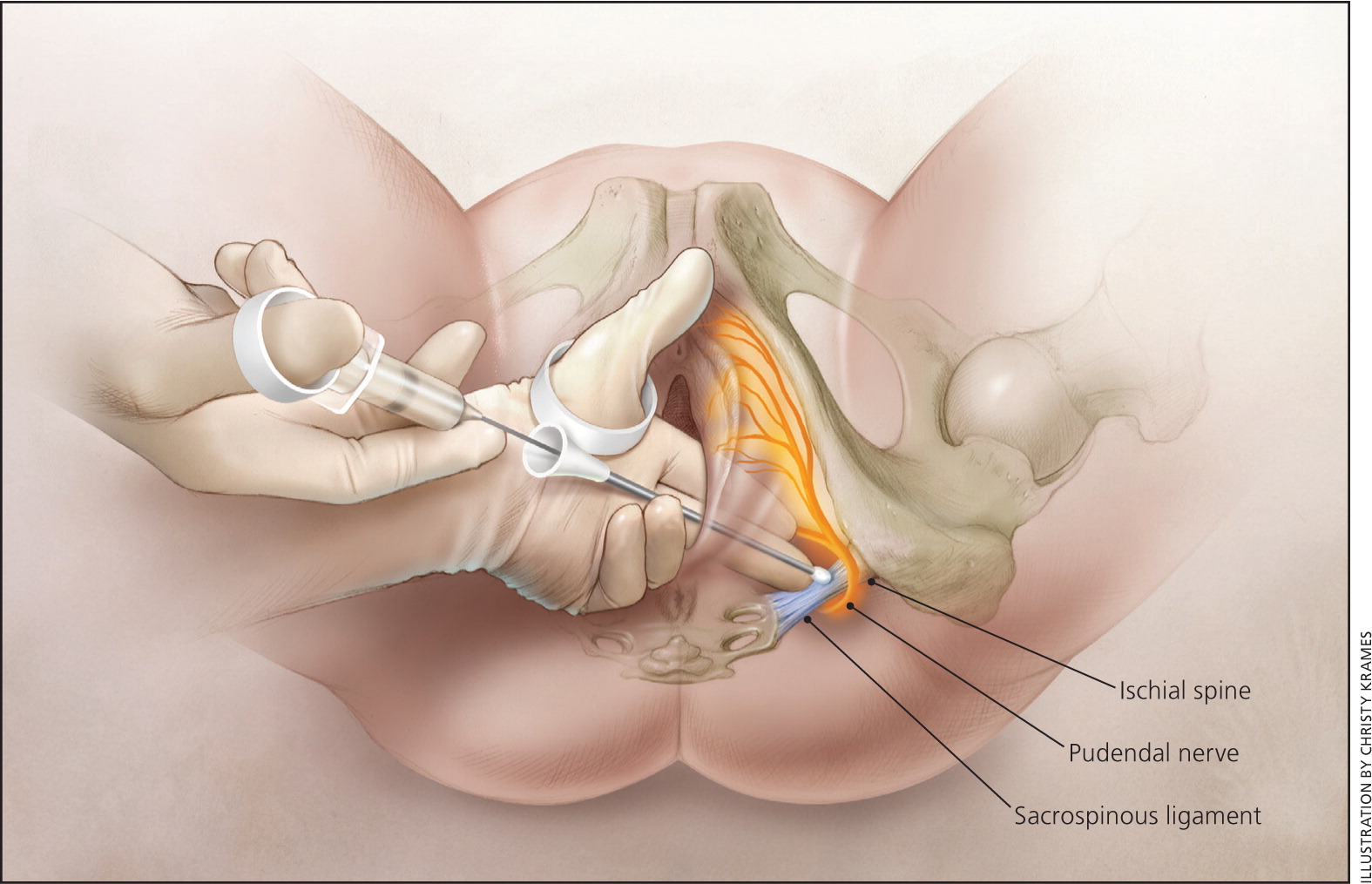
In an RCT of 111 patients, 56 received pudendal block and 55 received subarachnoid block at 7 cm or greater. Of the patients who received subarachnoid block, all but one reported satisfaction in pain relief, whereas 40 patients who received pudendal block reported no improvement in pain with contractions.9
IMMERSION IN WATER
Immersion in water during the first stage of labor significantly reduces the patient's perception of pain and decreases the use of epidural or spinal analgesia without affecting the rates of assisted vaginal deliveries, cesarean deliveries, maternal infection, Apgar scores, neonatal unit admissions, or neonatal infections.27 A 2004 study found that water immersion resulted in a decrease in time to delivery in patients with slow labor progress.11
OTHER TECHNIQUES
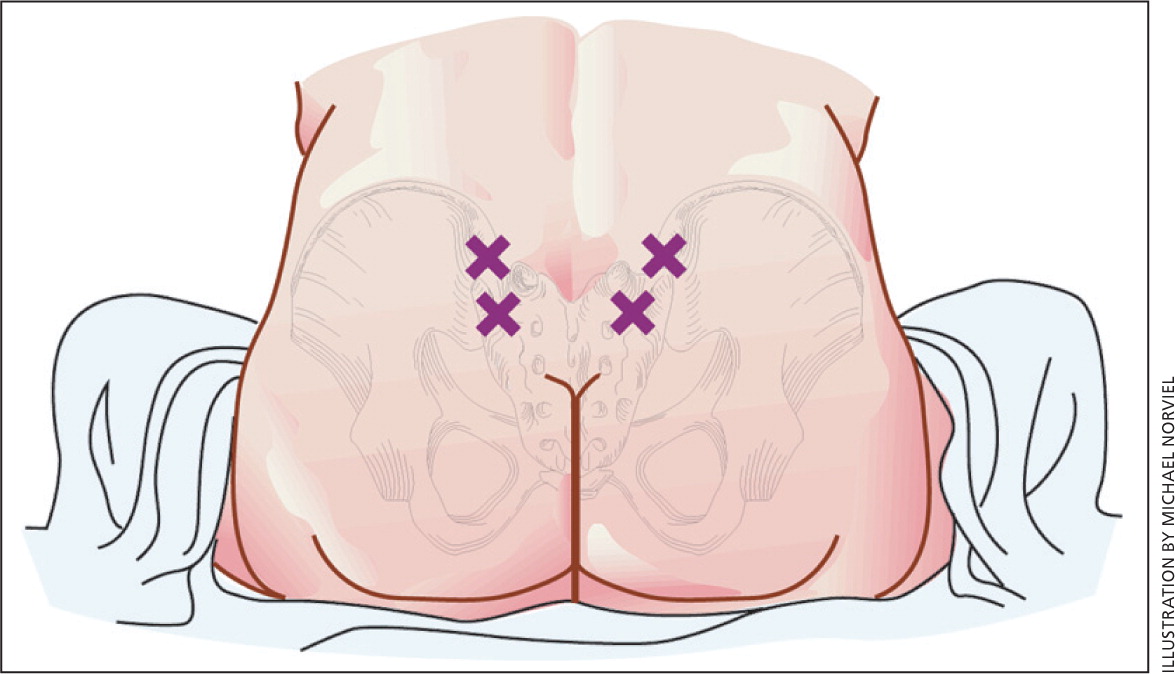
Sterile water injections into the lumbosacral spine (Figure 3) may limit some labor-related back pain for up to two to three hours, and have a rapid onset of action10; however, this technique has not been shown to affect the overall use of pain medications.4 Women using self-taught hypnosis required less pharmacologic analgesia (RR = 0.53; 95% CI, 0.36 to 0.79; n = 749), including epidural analgesia, and were more satisfied with their pain management in labor compared with the control group.5 Similarly, acupuncture decreased the need for medicated pain relief (RR = 0.70; 95% CI, 0.49 to 1.00; n = 288). These results were not replicated in women who used aromatherapy (i.e., essential oils) or audio analgesia (i.e., white sound set at 120 dB).4 These two modalities were evaluated in only a small number of patients (22 and 24, respectively).
Helping Patients Decide
Even though there are multiple options for labor pain management, women often experience pain during childbirth in accordance with their expectations.28 Analgesia options should be explored early in the prenatal period. Encouraging patients' participation in pain management may help reduce pain and increase their satisfaction in the childbirth experience. Physicians should know which analgesia options are available at the delivering institution, the patient's desire for regional analgesia, the availability of continuous labor support, and the potential for complications related to specific interventions.
Data Sources: A PubMed search was completed in Clinical Queries using the key terms regional anesthesia, labor, and pain management. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Agency for Healthcare Research and Quality, and the Cochrane Database of Systematic Reviews and POEMs critical appraisals from Essential Evidence Plus. Additionally, references from within those sources, as well as from within UpToDate, were searched. Search dates: December 1 to 10, 2010.
