
Am Fam Physician. 2013;87(7):486-490
A more recent article on management of chronic tendon injuries is available.
Author disclosure: No relevant financial affiliations.
Chronic tendon injuries present unique management challenges. The assumption that these injuries result from ongoing inflammation has caused physicians to rely on treatments demonstrated to be ineffective in the long term. Nonsteroidal anti-inflammatory drugs should be limited in the treatment of these injuries. Corticosteroid injections should be considered for temporizing pain relief only for rotator cuff tendinopathy. For chronic Achilles tendinopathy (symptoms lasting longer than six weeks), an intense eccentric strengthening program of the gastrocnemius/soleus complex improved pain and function between 60 and 90 percent in randomized trials. Evidence also supports eccentric exercise as a first-line option for chronic patellar tendon injuries. Other modalities such as prolotherapy, topical nitroglycerin, iontophoresis, phonophoresis, therapeutic ultrasound, extracorporeal shock wave therapy, and low-level laser therapy have less evidence of effectiveness but are reasonable second-line alternatives to surgery for patients who have persistent pain despite appropriate rehabilitative exercise.
Chronic tendon injuries are commonly presented to the primary care physician,1,2 and have a significant impact on the ability of patients to work, exercise, and perform routine daily activities. Because most of these conditions are attributable to overuse, patients may improve with rest, appropriate protection, and activity modification. However, patients with chronic symptoms (lasting longer than six weeks) often require further care for a return to full, pain-free function. Although general approaches may be helpful, the location and precise anatomic diagnosis determine specific management of chronic tendon injuries.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Eccentric exercise should be the first-line treatment for chronic midsubstance Achilles tendinopathy. | A | 14, 15, 19 |
| Corticosteroid injections, bracing, and nonsteroidal anti-inflammatory drugs are not effective in providing long-term relief for chronic degenerative tendon injuries. | B | 25, 31 |
| Rehabilitative exercise is an effective therapy for chronic tendon injuries. | B | 14, 15, 19 |
Pathophysiology
Bleeding and subsequent inflammation play an integral role in the acute response to many soft tissue injuries, but not in chronic tendon injuries. Overuse or chronic tendon injuries classically occur in tissues with poor blood supply and feature collagen separation and collagen degeneration rather than the typical cellular and protein responses related to the classical inflammatory cascade.3 Neovascularity is seen consistently in symptomatic portions of the tendon structure.4 Chronic pain in the tendon and surrounding tissue appears to be mediated by glutamate and other non-prostaglandin pathways.5,6 These tissue changes and pain generation pathways are not well described by traditional clinical terms such as “tendonitis” and “epicondylitis.” More importantly, these terms may promulgate a fundamental misunderstanding of the pathology underlying chronic tendon injury. These conditions are more accurately referred to as “tendinosis” or “tendinopathy.”
General Principles for Steroid and NSAID Use
Despite widespread use, there is little evidence to support the use of nonsteroidal anti-inflammatory drugs (NSAIDs) to treat chronic tendon injuries.7 Many patients are unaware of the risks of long-term NSAID use, including gastrointestinal toxicity, renal damage, and increased cardiovascular risk.8 The long durations of chronic tendon injuries may result in higher rates of adverse effects from NSAIDs.9
For noninflammatory degenerative tendon injuries such as rotator cuff tendinopathy 10and wrist extensor tendinopathy at the elbow (lateral epicondylitis),11 corticosteroid injections may provide short-term pain relief. However, the evidence is inconsistent for longer-term relief and ultimate restoration of pain-free function resulting from steroid injections.12 Additionally, case reports suggest that steroid injections may predispose tendons to rupturing, particularly the tendons of the hands and in weight-bearing joints such as the patellar tendon and the Achilles tendon.13 Therefore, in cases of noninflammatory chronic tendinopathy, steroids should be used sparingly and primarily to provide short-term windows of pain relief to allow patients to engage in curative rehabilitative therapy.
Achilles Tendinopathy
Achilles tendinopathy classically presents with pain during and after prolonged walking or running, typically in the area directly between the myotendinous junction and the insertion on the calcaneus. To distinguish this more common presentation from insertional Achilles injury, these injuries are referred to as midsubstance Achilles tendinopathies (Figure 1).

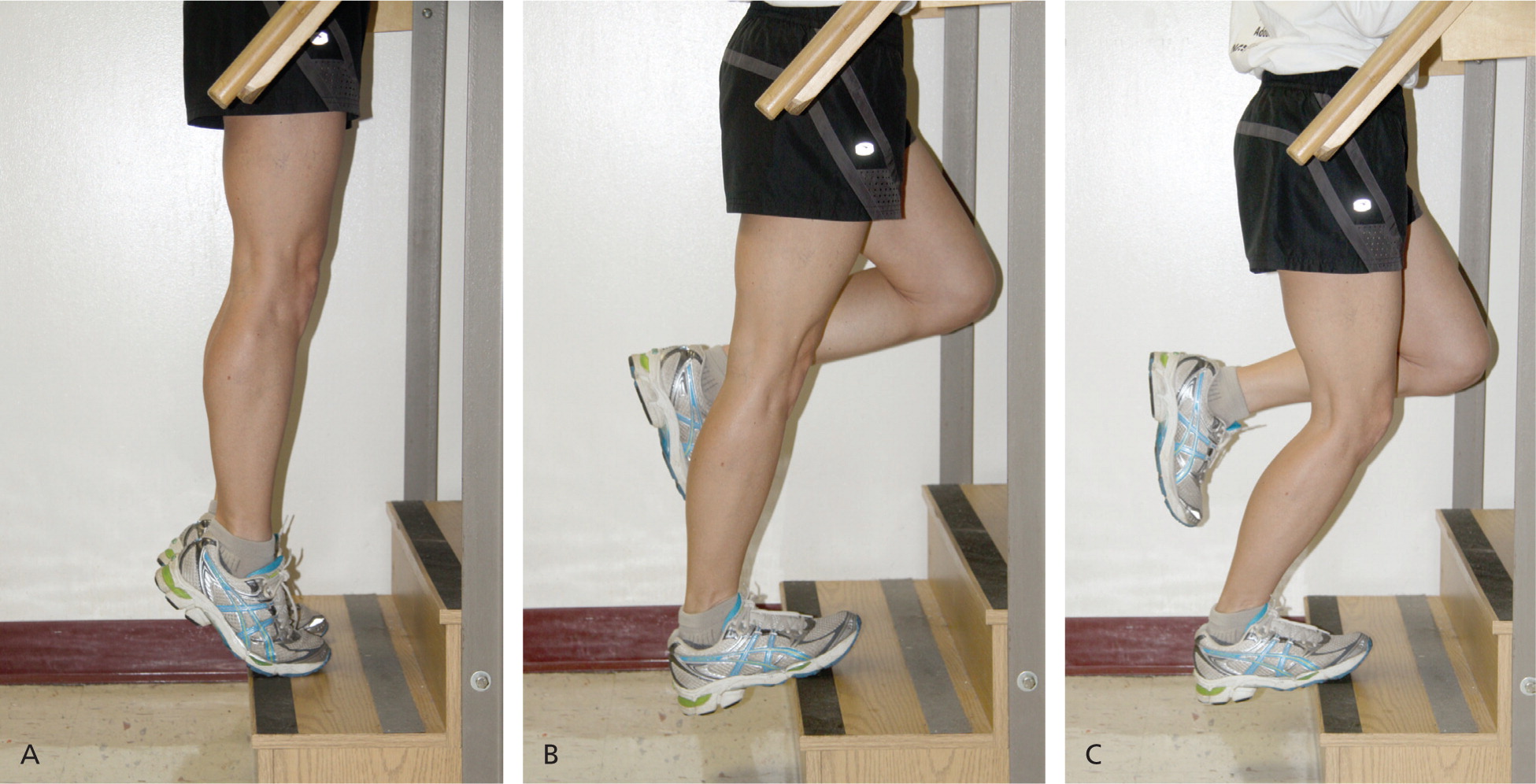
Midsubstance Achilles tendinopathy exemplifies the shift away from traditional treatment such as NSAIDs, ice, and stretching. For chronic midsubstance Achilles tendinopathy (symptoms lasting longer than six weeks) the preferred first-line treatment is an intense eccentric strengthening program of the gastrocnemius/soleus complex.14 Good-quality randomized controlled trials indicate that eccentric strengthening programs provide 60 to 90 percent improvement in pain and function.15 The basic protocol for eccentric rehabilitation of the Achilles tendon is detailed in Table 116 and is demonstrated in Figure 2.
| Frequency | Progression | Duration |
|---|---|---|
| Three sets of 15 exercises, twice daily (total of 90 repetitions) | Use same weight for first 1 to 2 weeks to achieve relative comfort with recommended daily frequency, then add weight (e.g., loaded backpacks, weighted vests) as comfort allows | Typical regimens last 12 weeks |
| Goal is a return to pain-free function with provocative activities, such as running |
Therapeutic modalities such as ultrasound, electrical stimulation, iontophoresis, and massage and stretching are inconsistent in helping patients achieve long-term return to function.17 Surgical techniques exist for severe or recalcitrant cases,18 but are inconsistently successful and carry additional risk.
Insertional Achilles tendon injuries are distinct from and less common than midsubstance tendinopathies. Typically, insertional Achilles tendon pain is more difficult to treat. Eccentric rehabilitation may be helpful, but this type of therapy does not show the same degree of utility as in midsubstance injuries, with rates of improvement closer to 30 percent for insertional injuries.19 Shock wave therapy is another option for insertional Achilles tendon injuries, but further studies are needed to establish benefit.20 Because cure rates are similar and eccentric exercise is much less expensive than shock wave therapy, the preferred initial therapy for chronic insertional Achilles tendon pain is eccentric strengthening following four to six weeks of immobilization in a walking boot.
Patellar Tendinopathy
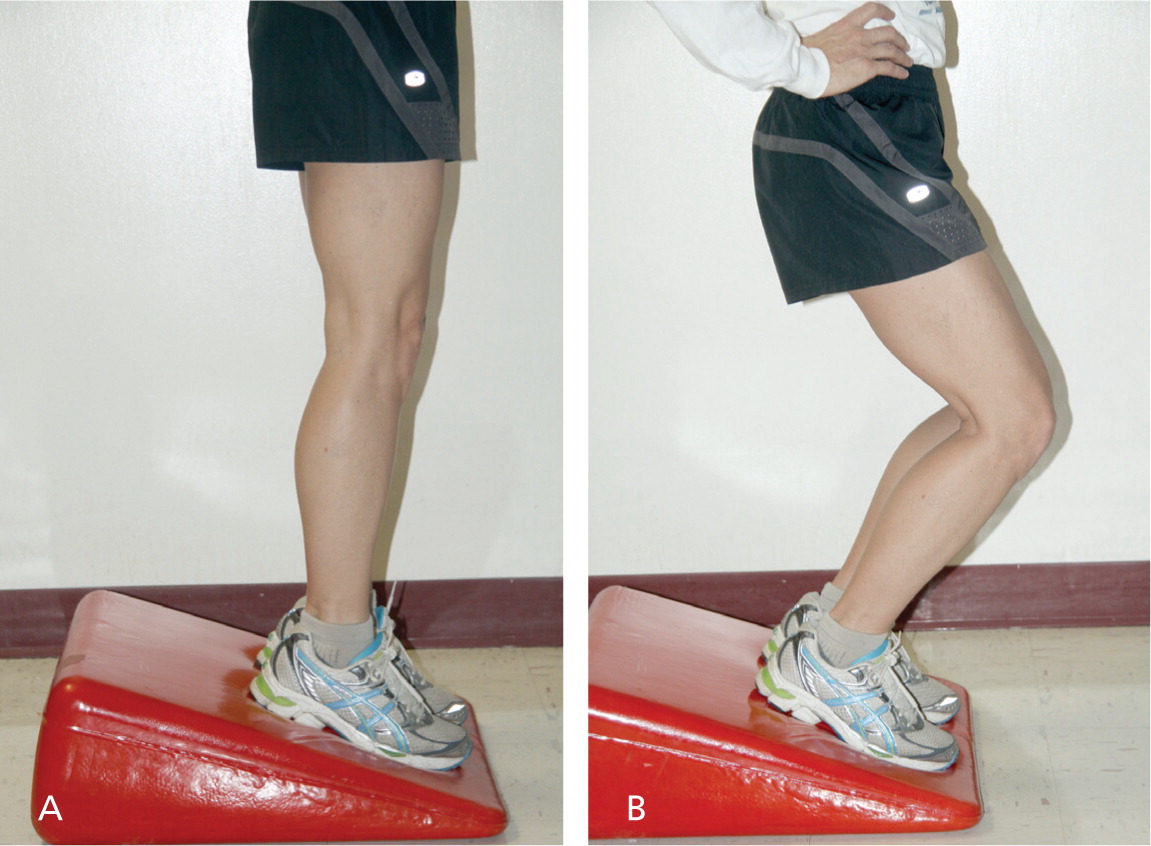
Patellar tendinopathy, or jumper's knee, can persist for years without a reliable response to conservative therapies.21 Evidence supports the use of eccentric exercise as a first-line option for chronic patellar tendon injuries. Several specific protocols have been published for these exercises; most show positive effects in long-term studies.22 Figure 3 demonstrates a typical eccentric exercise regimen. Exercise protocols vary but are generally similar to those for Achilles tendinopathy (Table 116 ).
Surgery has been the traditional option for recalcitrant cases. However, a recent study showed that eccentric exercise resulted in greater improvement than surgery.23 Sclerosing agents such as polidocanol have been used to diminish the pain based on the presence of neovascularity in injured tissue. Although injections of sclerosing agents may diminish pain, the pain relief is no greater than that achieved with arthroscopic techniques.24
Lateral Epicondylitis
Lateral epicondylitis, or tennis elbow, is characterized by pain in the lateral elbow which is exacerbated by attempts to extend and supinate the wrist and hand against resistance. The injury involves the origin of the common extensor tendon on the lateral epicondyle of the humerus. The multiplicity of possible treatments is indicative of the often contradictory and constantly changing evidence regarding the treatments' relative effectiveness.
Physical therapy that emphasizes stretching and strengthening consistently demonstrates superior symptom relief over rest, NSAID use, steroid injections, or bracing alone at six weeks to one year after treatment initiation.25 Given its simplicity, proven effectiveness, and minimal potential to cause harm, physical therapy emphasizing wrist extensor strengthening and stretching is the cornerstone of lateral epicondylitis treatment. However, it is unclear if physical therapy or any other lateral epicondylitis treatment provides superior outcomes to simple rest and activity modification after one year.26,27
Local steroid injections provide short-term pain relief for chronic lateral epicondylitis; however, the improvements seen with steroid injections do not last. Moreover, a recent large randomized trial showed poorer long-term cure rates with steroid injections than with physical therapy or rest.27 In the absence of steroid injections, patients appear to have similar long-term improvement in pain regardless of treatment.
Numerous studies have suggested that autologous blood and platelet-rich plasma injections can be helpful.28,29 Additionally, a single study showed improved outcomes with the application of a nitroglycerin patch in patients with persistent lateral epicondyle pain who were undergoing continued physical therapy.30 Further study is needed to better identify a role for these treatments. Counterforce bracing near the elbow and extension block splinting at the wrist may provide short-term improvements in pain and function, but have limited evidence for long-term relief.31 Surgery is an option for recalcitrant cases, despite a lack of controlled evidence of its effectiveness.32
Rotator Cuff Tendinopathy
Rotator cuff tendinopathy is characterized by pain with lifting, pain with overhead motions, and discomfort at night. Most cases are not the result of trauma, but can often be traced to provocative activities such as throwing, lifting, and repeated overhead motions. Patients with significant trauma or the onset of functional weakness with mechanical loss of motion warrant further evaluation for full thickness rotator cuff tear or adhesive capsulitis. Physical therapy that focuses on achieving a full range of motion, strengthening the rotator cuff, and stabilizing the scapula is the mainstay of treatment.33
Steroid injections are commonly used to treat rotator cuff tendinopathy, but controlled studies have demonstrated modest benefit, particularly in the long term.34 Steroid injections should be reserved for patients who have discomfort that would limit them from engaging in rehabilitative exercises. Injections into the gluteal muscle versus guided injections into the subacromial bursa have demonstrated similar levels of pain relief.35 Surgical options are available for patients with persistent symptoms, or for patients in whom function cannot be maintained.
Additional Therapies
Local injections of dextrose, autologous blood, and platelet-rich plasma represent forms of prolotherapy, in which irritants or proinflammatory substances are injected into degenerative or damaged tissue in an attempt to induce a further healing response. The evidence for these methods varies broadly based on the target tissues and the substances being injected into the body.36 Other modalities include topical nitroglycerin, iontophoresis, phonophoresis, therapeutic ultrasound, extracorporeal shock wave therapy, and low-level laser therapy. Current data on the effectiveness of these modalities are mixed, and generally consist of small or poorly controlled studies.17,37–39 After confirming the diagnosis of chronic tendon pain, these interventions may be considered as less invasive and less costly alternatives to surgery for patients who have persistent pain despite appropriate rehabilitative exercise. However, the evidence does not currently support the use of these modalities as first-line treatments for any type of chronic tendinopathy.
Data Sources: A PubMed search was completed in Clinical Queries using the key terms chronic tendon, tendinosis, tendinopathy, tendinitis, tendon and NSAID, tendon and steroid, Achilles tendinitis, patellar tendinitis, lateral epicondylitis, and rotator cuff. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. We also searched Essential Evidence Plus, the Agency for Healthcare Research and Quality evidence reports, Bandolier, Clinical Evidence, the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effects, the Institute for Clinical Systems Improvement, the National Guideline Clearinghouse database, and UpToDate. Search date: May 1, 2011.
