
Am Fam Physician. 2013;88(3):199-200
Author disclosure: No relevant financial affiliations.
An 88-year-old nursing home resident was admitted to the hospital with nausea, vomiting, diarrhea, and fever. At presentation she had type 2 diabetes mellitus, stroke, colovesical fistula, atrial fibrillation, and Alzheimer's dementia. Four days after she was admitted, she developed shortness of breath with an oxygen saturation of 90%. She was given 2 L of supplemental oxygen via nasal cannula, which raised her oxygen saturation to 98%.
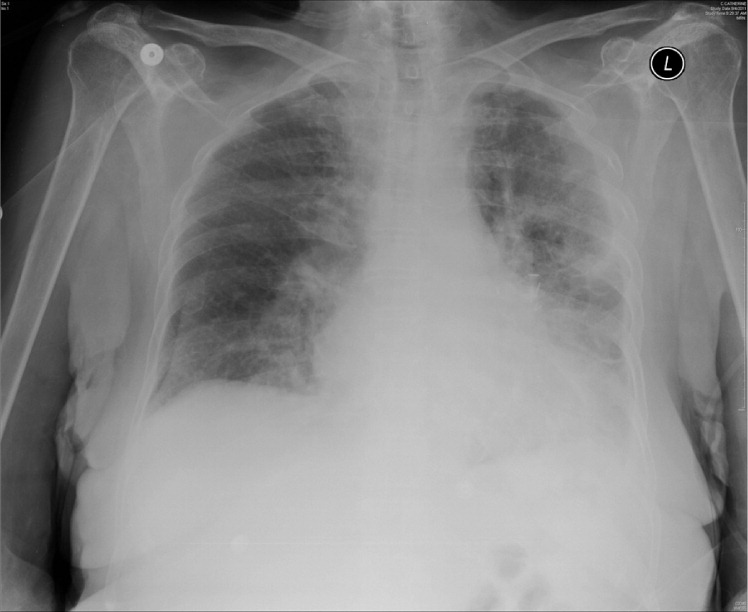
The patient was stable, and all other vital signs were normal. She had no respiratory distress, increased work of breathing, tachycardia, tachypnea, or fever. The lung examination revealed equal breath sounds and good air movement bilaterally in all lung fields. Chest radiography was performed (Figure 1).
Question
Discussion
The correct answer is A: continue current management for her admitted diagnoses, because the radiograph shows a pseudopneumothorax. A pseudopneumothorax can be identified on chest radiography by following the lung markings throughout the chest cavity. In a pseudopneumothorax, the periphery of the lung field will have lung markings. A true pneumothorax will not have lung markings beyond the edge of the pneumothorax. This patient's radiograph shows a fold of skin that is mimicking a pneumothorax (Figure 2). Other findings that may mimic pneumothorax include rib or scapular borders, lung blebs, an elevated hemidiaphragm, and colonic interposition. External agents, such as oxygen reservoir masks, clothing, and bedsheet folds may also look similar to a pneumothorax.1,2
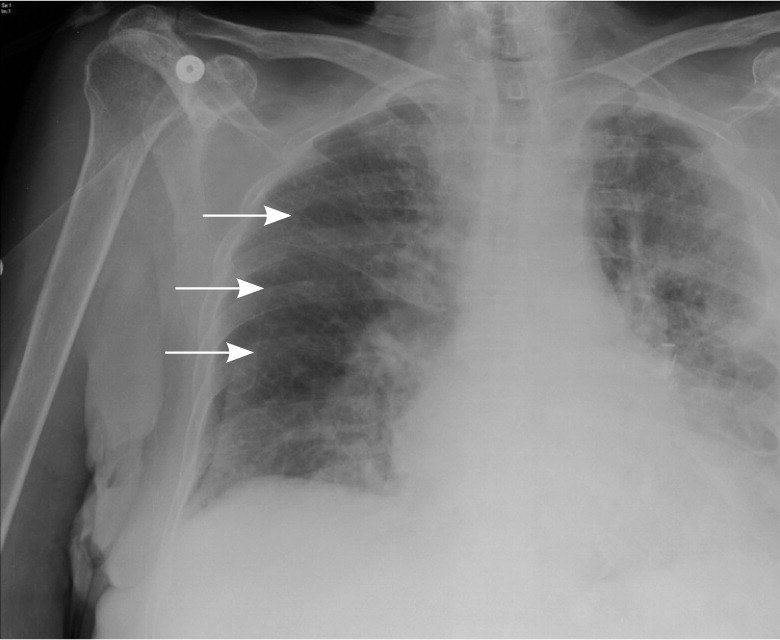
On chest radiography, a pseudopneumothorax may be described as a curvilinear shadow that overlies the lung parenchyma.4 A pneumothorax will have a clear, sharp line demarcating the diminished lung space. Because this patient is stable, there is no need for urgent invasive measures. The correct course of action is to observe and evaluate for other reasons for her change in respiratory status.
The goal is not to have 100% oxygen saturation. The patient is stable and oxygenating appropriately with supplemental oxygen via nasal cannula.
There is no need for a chest tube because the patient does not have a true pneumothorax, responded well to supplemental oxygen, and has no evidence of respiratory distress.
Immediate needle decompression is necessary only for a tension pneumothorax. Patients with a tension pneumothorax are usually unstable and will decompensate quickly.
| Condition | Characteristics |
|---|---|
| Pneumonia | Fever, cough, tachypnea, shortness of breath; radiograph may show pleural effusions, pulmonary infiltrates |
| Pneumothorax | No pulmonary marking visible beyond the edge of the pneumothorax, visceral and parietal pleura are separated; decreased oxygen saturation with tachypnea in most cases |
| Pseudopneumothorax | Lung markings extend beyond the line of demarcation, mainly seen on supine views, patient is stable and not in respiratory distress |
| Pulmonary embolism | Patient may have history of recent operation, immobility, coagulopathy; radiograph usually appears normal, but wedge-shaped infiltrate and atelectasis may be seen |
| Tension pneumothorax | Rapid respiratory compromise, radiograph may show tracheal deviation along with pneumothorax |
