A more recent article on acute shoulder injuries in adults is available.
Am Fam Physician. 2016;94(2):119-127
Author disclosure: No relevant financial affiliation.
Acute shoulder injuries in adults are often initially managed by family physicians. Common acute shoulder injuries include acromioclavicular joint injuries, clavicle fractures, glenohumeral dislocations, proximal humerus fractures, and rotator cuff tears. Acromioclavicular joint injuries and clavicle fractures mostly occur in young adults as the result of a sports injury or direct trauma. Most nondisplaced or minimally displaced injuries can be treated conservatively. Treatment includes pain management, short-term use of a sling for comfort, and physical therapy as needed. Glenohumeral dislocations can result from contact sports, falls, bicycle accidents, and similar high-impact trauma. Patients will usually hold the affected arm in their contralateral hand and have pain with motion and decreased motion at the shoulder. Physical findings may include a palpable humeral head in the axilla or a dimple inferior to the acromion laterally. Reduction maneuvers usually require intra-articular lidocaine or intravenous analgesia. Proximal humerus fractures often occur in older patients after a low-energy fall. Radiography of the shoulder should include a true anteroposterior view of the glenoid, scapular Y view, and axillary view. Most of these fractures can be managed nonoperatively, using a sling, early range-of-motion exercises, and strength training. Rotator cuff tears can cause difficulty with overhead activities or pain that awakens the patient from sleep. On physical examination, patients may be unable to hold the affected arm in an elevated position. It is important to recognize the sometimes subtle signs and symptoms of acute shoulder injuries to ensure proper management and timely referral if necessary.
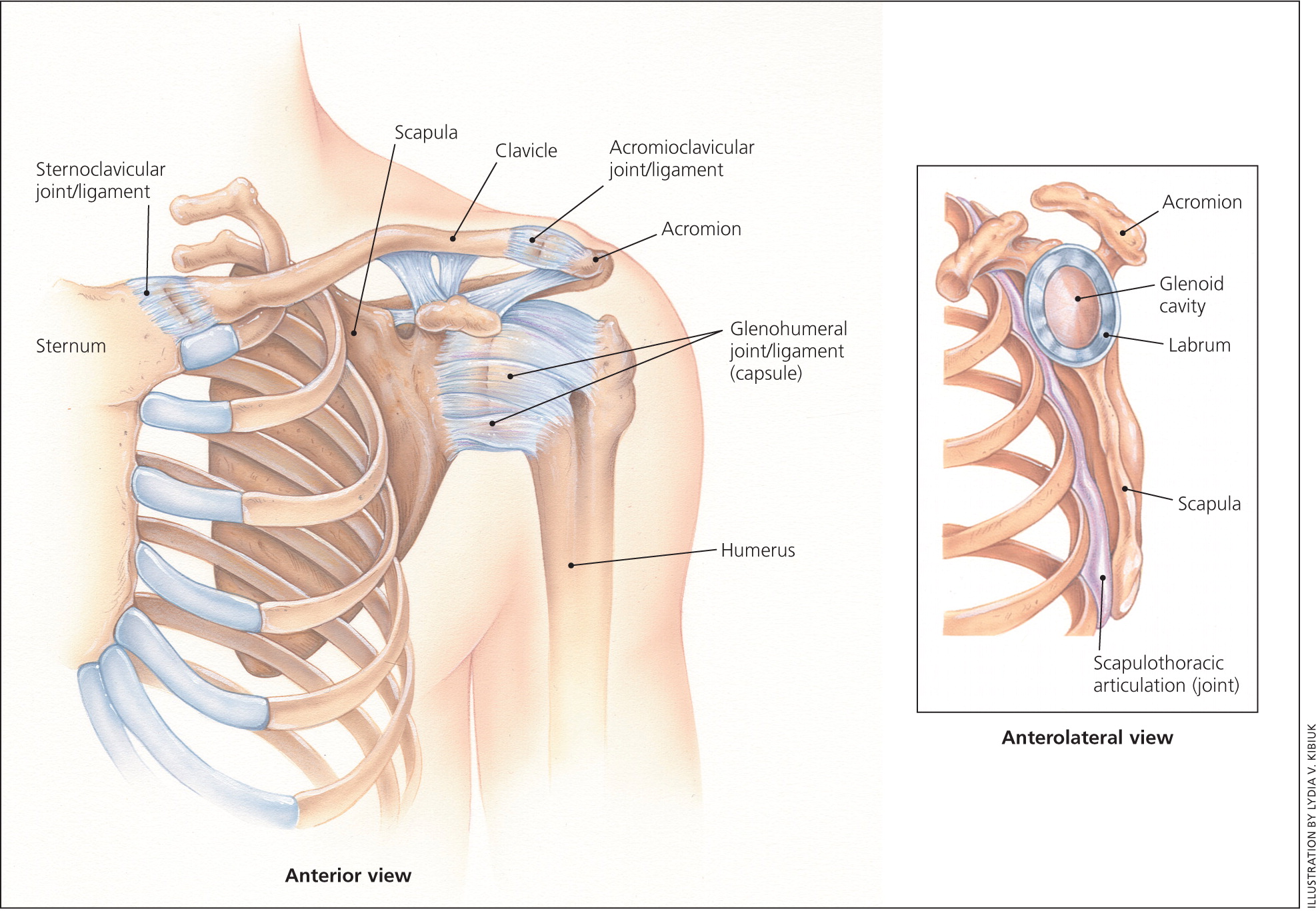
Acute shoulder injuries, such as proximal humerus fractures, acromioclavicular separations, clavicle fractures, shoulder dislocations, and rotator cuff tears, are often initially managed by family physicians. Understanding shoulder anatomy (Figure 11 ), the physical and radiographic evaluation, and treatment options are essential for a successful outcome. Most of these injuries can be managed without surgery by a knowledgeable family physician. However, it is important to know when to refer patients to an orthopedist. Table 1 summarizes the evaluation and management of different types of shoulder injuries.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Decisions about conservative vs. surgical treatment of acute middle one-third clavicle fractures should be individualized, considering the relative benefits and harms of each intervention and patient preferences. | B | 10, 14 |
| Surgery should be considered in young athletes with shoulder dislocations because of a high recurrence rate in these patients. | B | 18, 26 |
| Older patients with proximal humerus fractures can be treated nonoperatively because these patients have equivalent or better outcomes compared with those who have surgery. | B | 34–36 |
| The effectiveness and safety of surgery for chronic rotator cuff disease in older patients are unclear. | B | 17 |
| Injury | |||||
|---|---|---|---|---|---|
| Evaluation and management | Acromioclavicular joint injuries | Midshaft clavicle fractures | Glenohumeral joint dislocations | Proximal humerus fractures | Rotator cuff tears |
| Initial management | Sling for comfort | Sling for 2 to 6 weeks | Sling for 4 weeks | Sling for 6 to 8 weeks | Physical therapy for 6 weeks |
| Imaging | AP, axillary, and Zanca views | AP and serendipity views | AP, scapular Y, and axillary or Velpeau views to evaluate for associated fractures | AP view of the glenoid, scapular Y view, and axillary view | Magnetic resonance imaging without contrast media is preferred for diagnosing tears; radiography is usually not helpful but could be used to rule out other causes of shoulder pain or massive rotator cuff tears |
| Follow-up intervals | 2 weeks, start physical therapy when comfortable | 4 weeks, start physical therapy | 2 weeks for repeat radiography; start physical therapy at 2 to 4 weeks | 3 weeks for repeat radiography and to begin physical therapy | 6 weeks for clinical evaluation |
| Indications for referral | Rockwood types III to VI injuries | Displaced group I fractures and all group II fractures, persons participating in high performance sports, suspected posterior sternoclavicular dislocation | Young athletes, patients with their first dislocation or recurrent dislocations | Young or active patients with 2-, 3-, or 4-part proximal humerus fractures | Any patient with a suspected tear, especially young, active, healthy patients with a full-thickness tear |
Acromioclavicular Joint Injuries
Acromioclavicular joint injuries are common in young adults as the result of sports injury or direct trauma.2 The most common mechanism of injury is a fall onto a shoulder with the arm in an adducted position, which displaces the acromion medially and inferiorly relative to the clavicle, straining the surrounding structures.
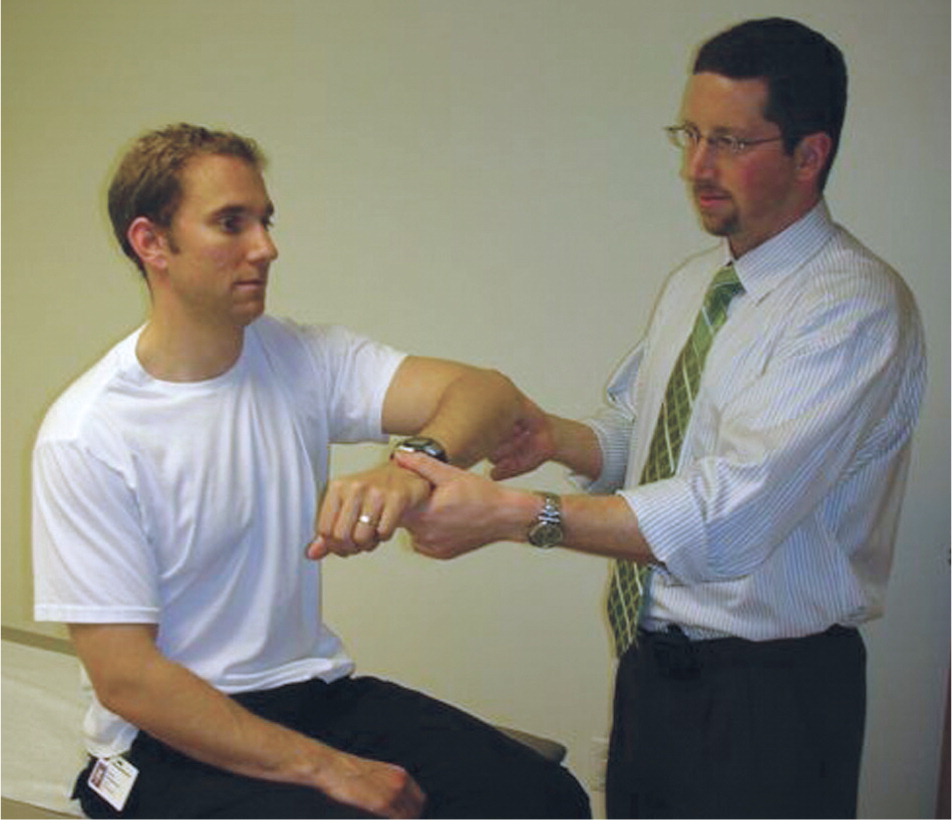
Physical examination focuses on the bony prominences and neurovascular status of the injured extremity. Depending on the severity of injury, there may be an obvious swelling or deformity from the displaced distal clavicle. The entire clavicle should be palpated to rule out an associated fracture or sternoclavicular dislocation. Rarely, displacement of the clavicle may injure the brachial plexus.3 With the patient seated and the injured extremity relaxed at the side, provocative maneuvers, such as the cross-body adduction test (Figure 24 ), can be used to isolate and assess the stability of the acromioclavicular joint. A video on the evaluation of the joint is available at https://www.youtube.com/watch?v=daPnkXo03yM.
Appropriate radiographs should be obtained to help classify the injury and rule out fracture. The ideal series to view the acromioclavicular joint includes a true anteroposterior view, Zanca view (10- to 15-degree cephalic tilt), and axillary view. The Rockwood system (Figure 31 ) is widely used to classify the six types of acromioclavicular joint injuries.5 Radiographs showing the injury types are available at http://radiopaedia.org/articles/acromioclavicular-joint-injury-rockwood-classification.
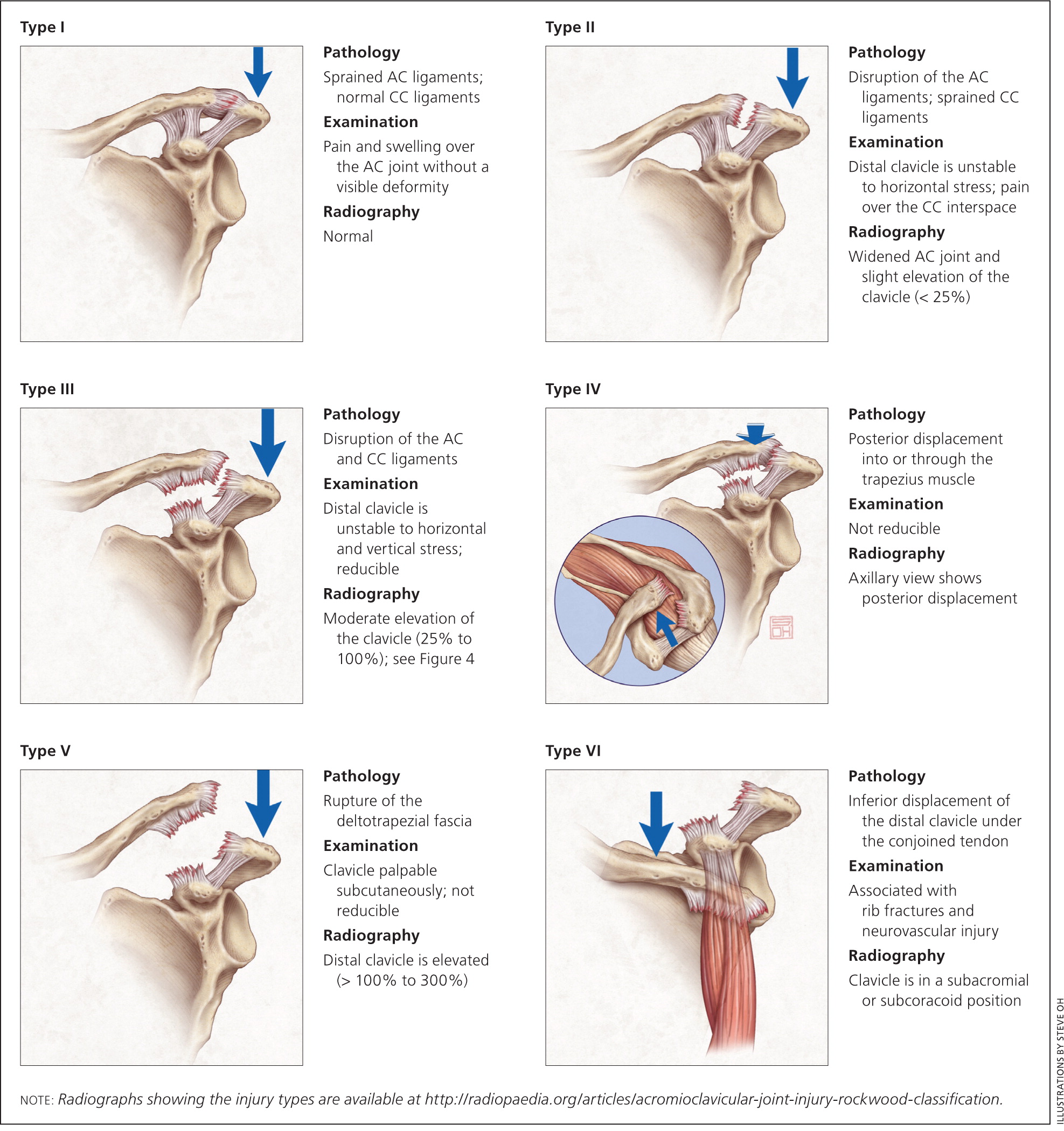
Acromioclavicular joint injury types I (no clavicle displacement) and II (slight elevation of the clavicle [less than 25%]) are treated nonoperatively. Patients may use a sling for comfort, ice application, and over-the-counter pain medication as needed. Symptom duration is generally one to three weeks for type I injuries and four to six weeks for type II injuries. Use of a sling should be limited to one to two weeks to minimize shoulder stiffness. The management of type III injuries (moderate elevation of the clavicle [25% to 100%]; Figure 41) is controversial, and patients with these injuries should be referred to an orthopedist.6 Younger, active patients may benefit from operative intervention.7 However, treatment is determined individually, with the initial management generally being nonoperative.8 Patients with type III injuries are symptomatic for up to three months. Types IV, V, and VI injuries are treated surgically and should be referred to an orthopedist in a timely manner.

Patients who do not undergo surgery should be encouraged to discontinue use of the sling and perform range-of-motion exercises as soon as pain allows. Physical therapy focuses on regaining motion, shoulder strength, and scapular stabilization. Active patients may return to sports when they are pain free, and strength and range of motion are equal to the uninjured side. Although most patients report good to excellent outcomes, some experience residual symptoms with activities and develop degenerative changes at the acromioclavicular joint.9
Clavicle Fractures
Clavicle fractures account for about 2.6% of all fractures10 and are usually caused by a fall onto the top of the shoulder. They are common in young adults as the result of sports injury or direct trauma. There is usually pain with palpation of the clavicle. It is important to perform a careful neurovascular examination of the affected extremity because the clavicle protects the great vessels, lungs, and brachial plexus. Although injuries to those structures are rare, they can be severe and require immediate referral. Urgent orthopedic evaluation is also required for open injuries or if the fracture is causing tenting of the skin. Radiography of the clavicle should include at least anteroposterior and serendipity views.
Nondisplaced clavicle fractures generally can be treated conservatively in a sling for two to six weeks. Passive range of motion of the shoulder should occur as early as pain allows to prevent shoulder stiffness. Multiple studies have shown no difference in outcomes using a sling vs. a figure-of-eight bandage. However, there is less patient discomfort and skin irritation with a sling.11,12
Clavicle fractures can be categorized using the Allman classification.13 Group I fractures are those in the middle one-third of the clavicle and account for 80% of fractures.10 Treatment of clavicle fractures that are displaced or overlapped more than 2 cm is becoming increasingly controversial. Studies show that patients who undergo surgery have an earlier return to activities and lower rate of nonunion, but more complications than those who do not have surgery; there is no difference in long-term function.10,14,15 Patients treated conservatively should also be aware of the possibility of a palpable callus once the fracture heals.
Group II fractures are those in the distal one-third of the clavicle. Certain subtypes tend to displace more often than others, and it is controversial whether operative fixation is necessary in these cases. If treated without surgery, nonunion of group II injuries ranges from 28% to 44%, but the functional and chronic pain outcomes are unclear.16 Referral to an orthopedist for further evaluation is important in patients with displaced group I fractures and all group II fractures, as well as individuals participating in high performance sports.
Group III fractures are those in the medial clavicle and are almost always treated nonoperatively using a sling. They are the least common clavicle fracture, and are most likely evaluated in the emergency department because they are often associated with multisystem trauma. Radiography can miss injuries to the medial one-third of the clavicle, including sternoclavicular dislocations. If a posterior sternoclavicular dislocation is suspected on physical examination (e.g., difficulty breathing, asymmetric upper extremity pulses, asymmetric medial clavicle prominences), the patient should be urgently referred to the emergency department for further evaluation, including computed tomography, because there is an increased risk of pulmonary and great vessel damage with this injury.
Glenohumeral Dislocation
The most commonly dislocated joint is the glenohumeral joint, with rates as high as 24 per 100,000 persons annually. This dislocation results from contact sports, falls, bicycle accidents, and similar high-impact trauma.17 A combined force of abduction, extension, and external rotation on the shoulder causes an anterior shoulder dislocation, which constitutes about 90% of dislocations.18 Posterior dislocations can also occur from a posteriorly directed force on a flexed shoulder, or from an electric shock or seizure injury. Inferior (luxatio erecta) and superior dislocations are less common.
On examination, patients with a glenohumeral dislocation usually hold the affected arm in their contralateral hand, and have pain with motion and decreased motion at the shoulder. Physical deformity may not be easily recognized, but some findings may include a palpable humeral head in the axilla or a dimple inferior to the acromion laterally. Axillary nerve injury is the most common associated nerve injury and thus sensation over the lateral aspect of the shoulder should be assessed; a motor examination of the deltoid may be limited because of pain. If deficits are present, electromyography should be performed to establish baseline values and assess recovery.19 Pulses should also be evaluated.
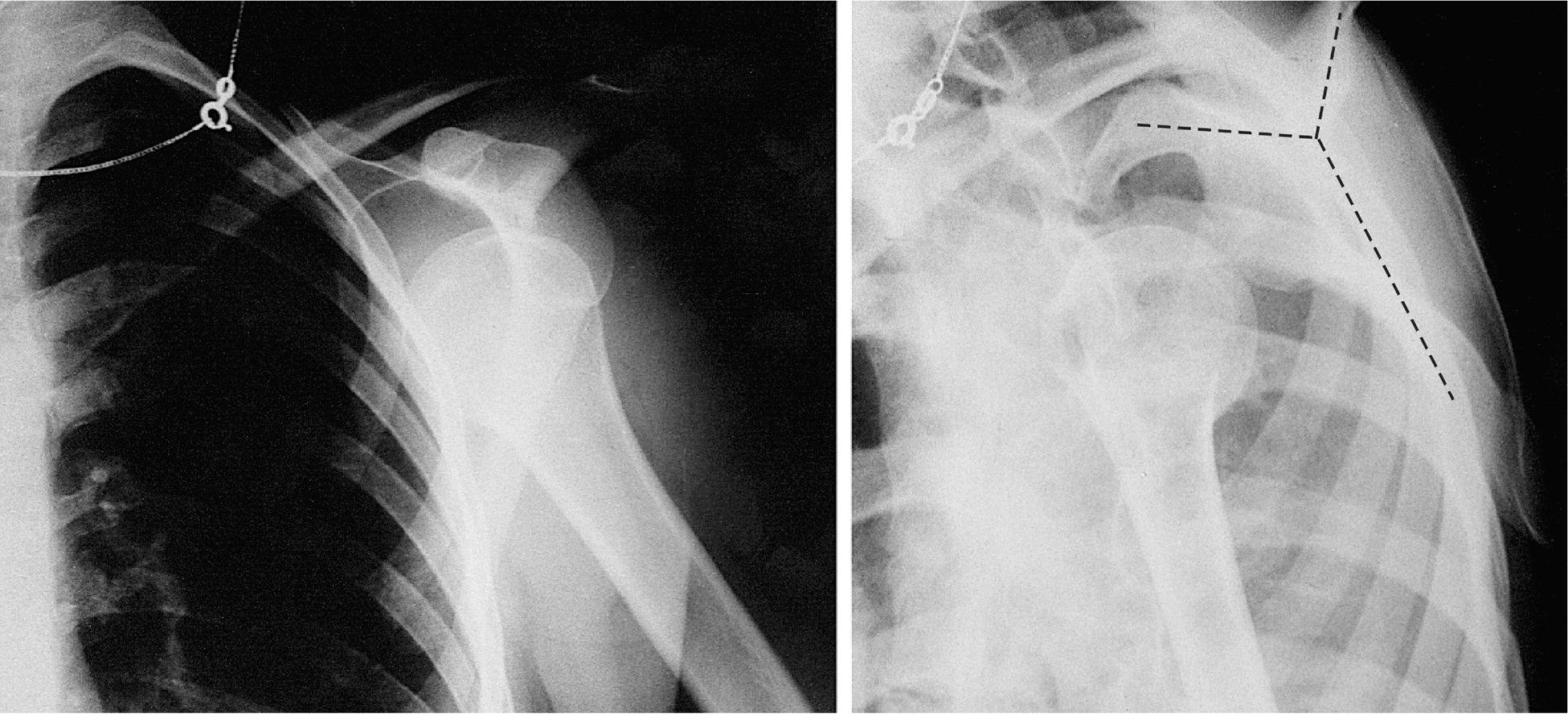
Associated rotator cuff injuries are more likely as patients age, and follow-up assessment of function is crucial once pain allows.20 The neurovascular examination is exceedingly important in patients with a rare inferior dislocation because these patients have an even higher risk of neurovascular and rotator cuff injury.21 In patients with a suspected shoulder dislocation, radiography should include three views of the shoulder: anteroposterior, scapular Y, and axillary or Velpeau (Figures 522 and 6). Additional examples of shoulder radiographs are available at http://eorif.com/shoulder-xray.

Multiple maneuvers have been used to reduce anterior shoulder dislocations with varying success.21 A video depicting shoulder reduction techniques is available at https://www.youtube.com/watch?v=8xibzOM7Hp0. If the dislocation is treated immediately, such as on an athletic field, reduction may be attempted without pain medication because spasms have not yet set in. A Cochrane review found that using intra-articular lidocaine is as effective as using intravenous analgesia, with or without sedation, in success of reduction and pain relief for acute shoulder dislocations.23 Using the intra-articular injection technique, the shoulder can be injected posteriorly with about 20 mL of lidocaine 1%, 1.5 cm distal and 1 to 2 cm medial to the posterolateral corner of the acromion. Alternatively, the joint could be injected laterally, aiming for the void in the glenoid fossa that the humeral head has dislocated from.
After reduction, repeat radiography is needed to confirm success, and a sling is placed. Physical therapy begins after two to four weeks, with passive range of motion and then progressive strengthening. Return to activities is delayed until there is equal strength and motion compared with the contralateral side. Most studies show that one week is the optimal duration of immobilization, and that there is no difference in outcomes between immobilization in internal or external rotation.24,25
In adults, the risk of repeat dislocation increases with younger age at the time of first dislocation.18,24 Multiple variables, such as bony, ligamentous, labral, and rotator cuff injuries, impact further treatment decisions, and thus patients should be referred to an orthopedist to have a personalized discussion about possible surgical management.26 Surgery should be considered in young athletes with a shoulder dislocation because of the high recurrence rate in these patients.18,26
Proximal Humerus Fractures
Most proximal humerus fractures occur in the older population as a result of a low-energy fall. In patients younger than 50 years, sports and motor vehicle crashes are the most common mechanisms of injury.2 All extremities should be examined to rule out distal radius and proximal femur fractures, which are the orthopedic injuries most commonly associated with proximal humerus fractures.27 Physical examination of the shoulder begins with inspection and palpation, which may reveal a lateral subacromial skin dimple or an anterior prominence suggestive of a dislocation. Rotator cuff injuries are common, although pain from acute trauma limits functional testing of the shoulder.28,29 Sensation laterally over the deltoid muscle representing the axillary nerve should be tested. Distally, the motor and sensory status of the median, radial, and ulnar nerves should be documented. The radial artery should be palpated as part of the vascular examination. A cool, pulseless extremity after reduction requires emergent evaluation by a vascular surgeon. Although rare, open injuries require urgent antibiotic administration and orthopedic surgical intervention.
Appropriate radiographs should be obtained to classify the fracture pattern. The ideal shoulder series includes a true anteroposterior view of the glenoid, scapular Y view, and axillary view. If an axillary view is not possible because of pain, it may be omitted if there is an adequate scapular Y view ruling out dislocation.30,31
Neer proposed the most commonly used classification system to evaluate these fractures. It is based on fracture lines that separate the four anatomic landmarks of the proximal humerus.32 The Neer classification also describes the total number of displaced fragments, which become termed two-, three-, or four-part fractures. Almost one-half of proximal humerus fractures are minimally displaced, and only 3% are either four-part fractures or fracture dislocations.2 The classification system is available at https://www.shoulderdoc.co.uk/images/uploaded/neers_fracture_class.jpg.
As a rule, minimally displaced fractures can be treated successfully without surgery.33 The role of surgical intervention on displaced fractures is controversial because there are high rates of complications and inconsistent evidence showing improved functional outcomes.34–36 Older patients with proximal humerus fractures can be treated nonoperatively because these patients have equivalent or better outcomes compared with those who have surgery.34–36 Young and active adults with two-, three-, or four-part fractures should be referred to an orthopedist for treatment.
Nonoperative treatment consists of sling immobilization for comfort followed by range-of-motion exercises and strength training. Patients should be advised to sleep in a semirecumbent position (e.g., 45-degree position in a recliner) for comfort. Early motion is critical to limit long-term stiffness and pain. Immediate range of motion should include the neck, elbow, wrist, and fingers on the affected side. A video of initial shoulder rehabilitation exercises is available at https://www.youtube.com/watch?v=zYVvWLZ1Unw. Within three weeks of injury, pendulum shoulder exercises should be initiated.37–39 These involve flexing at the waist while allowing the affected arm to hang forward with gravity and moving the arm in circles, gradually making the circles larger as pain subsides ( https://www.youtube.com/watch?v=sdl2f0Kb7vY). At around three weeks, patients begin flexion, abduction, and internal rotation exercises using the wall and contralateral extremity for assistance ( https://www.youtube.com/watch?v=I8U3HYtlSxY). After six to eight weeks and fracture union, the sling should be discontinued and active range-of-motion and light functional activities can be initiated. As pain subsides, it is important to assess for rotator cuff pathology by testing rotator cuff muscle strength. At 12 weeks, a more aggressive rotator cuff strengthening program can be initiated if needed40 ( https://www.youtube.com/watch?v=KfznK-Rc4vY and https://www.youtube.com/watch?v=ZbBXJej5ttM).
In the older population, the mortality rate at one year is 10%; independence before injury is the best predictor of outcome.41 Rehabilitation is complete when pain is controlled and shoulder function has been restored.
Rotator Cuff Tears
Rotator cuff disease encompasses a range of pathologies that affect the four muscles making up the rotator cuff (Figure 71 ). The incidence of full-thickness tears is between 5% and 40%, with some of those tears being chronic lesions and many being asymptomatic.42 Acute rotator cuff tears can be caused by a fairly minor injury to the shoulder in an older person or by a significant trauma, such as a shoulder dislocation or motor vehicle crash. Pain with overhead activities and pain that awakens the patient from sleep are typically reported, although a recent review shows that they may not be useful in diagnosing rotator cuff tears.43
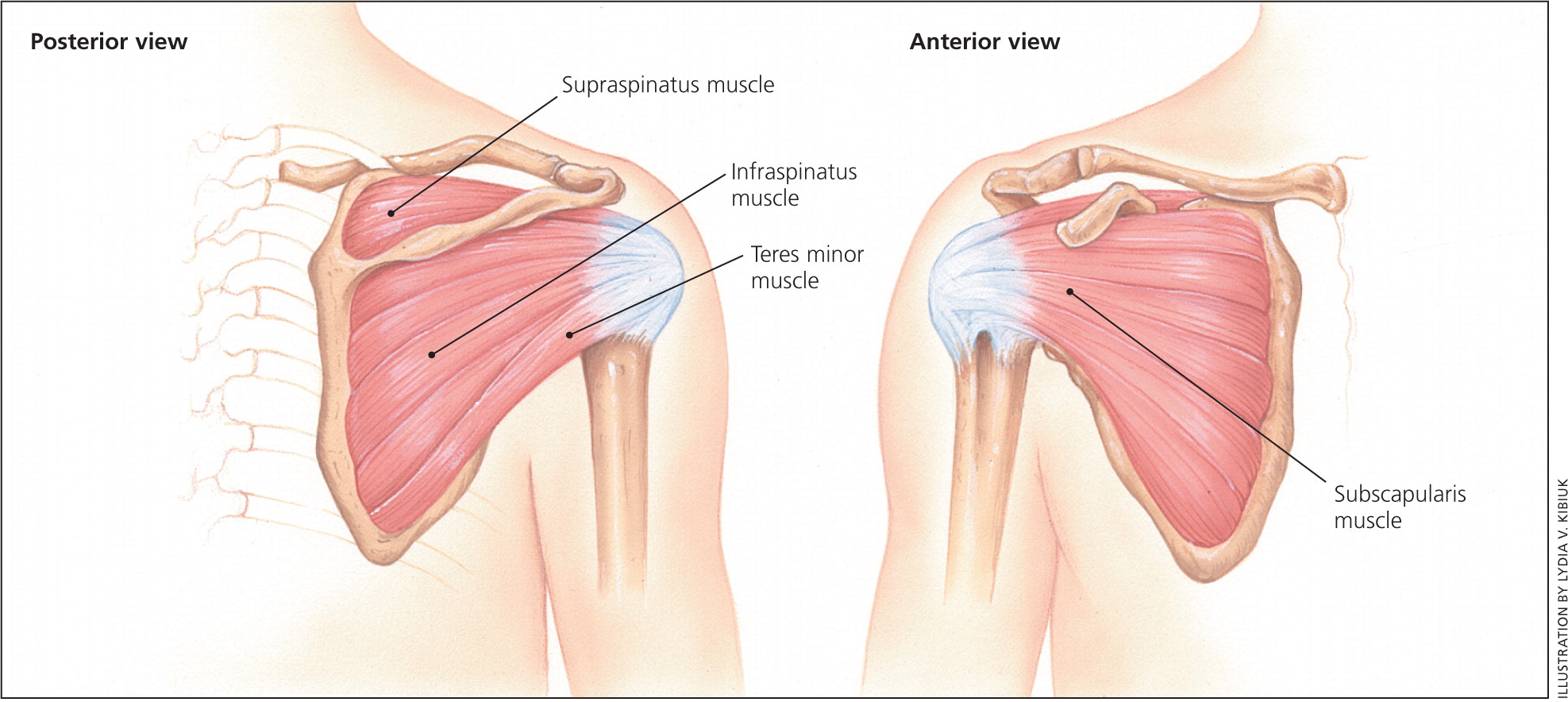
One test often used to assess the most commonly torn tendon, the supraspinatus, is the drop-arm test. With this test, the patient's arm is passively brought to 90 degrees abduction. The test result is positive if the patient is unable to hold the arm in the air as the examiner lets go ( https://www.youtube.com/watch?v=qvwYEoeHPaA). There are many physical examination maneuvers that test the rotator cuff's integrity, but reliably identifying a tear is difficult even for subspecialists.43 Radiography is usually not helpful in diagnosing rotator cuff pathology but could be used to rule out other causes of shoulder pain, such as calcific tendinopathy or subacromial spurring. Magnetic resonance imaging without contrast media is the imaging modality of choice for diagnosing tears.44 Recent studies have demonstrated that the effectiveness of ultrasonography is similar to that of MRI for the diagnosis of rotator cuff tears, and ultrasonography is more cost-effective.45 However, it should only be used if the physician is well trained in using ultrasonography and interpreting the results.
A concern with rotator cuff tears is the risk of progression, which can lead to atrophy of the rotator cuff and a tear that could have been repaired becoming irreversible.46 However, it is difficult to detect which tears will progress. Full-thickness tears and lesions in older patients are more likely to enlarge.
The effectiveness and safety of surgery for chronic rotator cuff disease in older patients are unclear.17 Patients with a suspected tear should be referred to an orthopedist for a discussion about the benefits of conservative vs. operative management. It is especially important to refer young, active, healthy patients with full-thickness tears to an orthopedist as soon as possible because early operative treatment may result in better outcomes.47,48
Data Sources: A PubMed search was completed in Clinical Queries using the key terms clavicle fractures, diagnosis, and treatment. This search included meta-analyses, randomized controlled trials, clinical trials, and reviews. A search was repeated for each section using the key terms proximal humerus fracture, glenohumeral dislocation, acromioclavicular sprains, and rotator cuff tears, respectively. We also searched the Cochrane Library, DynaMed, Essential Evidence Plus, ScienceDirect, Scopus, and Web of Science. Search date: May 1, 2015.