
Am Fam Physician. 2017;95(10):637-644
Patient information: See related handout on LASIK.
Author disclosure: No relevant financial affiliations.
A variety of refractive surgery techniques, which reshape the corneal stroma using laser energy, have been marketed as simple and safe alternatives to glasses or contact lenses. Laser-assisted in-situ keratomileusis (LASIK) is the most common of these procedures. Although there are few high-quality prospective studies of long-term outcomes, complications, or stability for refractive surgery procedures, there is at least general agreement that more than 90% of appropriately selected patients achieve excellent uncorrected distance vision. In addition to well-recognized contraindications (e.g., unstable refraction, pregnancy and lactation, chronic eye disease, systemic illness, corneal abnormalities), there are other conditions that warrant caution (e.g., excessively dry eyes, contact lens intolerance, chronic pain syndromes). Postoperative dry eye, which may in part represent a corneal neuropathy, usually resolves after six to 12 months but persists in up to 20% of patients. Up to 20% of patients may have new visual disturbances, particularly with night driving. Vision-threatening complications are rare. Intraocular lenses, implanted following cataract extraction, may be an alternative to LASIK in older patients. Although the overall dependence on corrective lenses is markedly reduced, many patients still require glasses or contact lenses after LASIK, particularly in low-light conditions and as they age. Most patients report satisfaction with the results. Family physicians can help patients make informed decisions by exploring their values, preferences, expectations, and tolerance of uncertainty and risk.
Over the past two decades, a variety of refractive surgery techniques have been developed and marketed as simple and safe alternatives to glasses or contact lenses. Laser-assisted in-situ keratomileusis (LASIK) is the best-known and most widely performed technique.
WHAT IS NEW ON THIS TOPIC: REFRACTIVE EYE SURGERY
In the Patient-Reported Outcomes with LASIK (PROWL) studies, excellent visual acuity was routinely achieved, with few highly bothersome, persistent symptoms and very rare vision-threatening complications. However, data are limited about the long-term stability of correction.
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Almost all appropriately selected patients achieve good vision with LASIK. | C | 3, 18 | Although most studies have been of limited quality, outcomes have been consistent over many years. |
| Caution individuals considering LASIK that dry eye symptoms affect up to 40% of patients following surgery. | B | 3, 18, 19 | Only 2% to 3% of patients consider dry eye symptoms to be bothersome. |
| Caution individuals with chronic pain syndromes (e.g., fibromyalgia, irritable bowel syndrome, migraine) or contact lens intolerance that patients with these conditions report more dry eye symptoms following LASIK. | C | 20, 21 | Dry eye symptoms are multifactorial, but some may be manifestations of corneal neuropathy. |
| Caution individuals considering LASIK that visual symptoms, such as a glare, halos, starbursts, and reduced contrast sensitivity, affect up to 20% of patients following surgery. | B | 3, 18, 22 | Less than 1% of patients reported “a lot of difficulty” in general with usual activities. |
| Ensure that individuals considering LASIK understand that they will still develop presbyopia and require reading glasses as they age. | C | 3, 11 | This must be thoroughly explained to patients. |
Approximately 600,000 individuals, usually in their 30s with discretionary income, undergo LASIK or similar procedures each year in the United States. Its popularity in this country has decreased from a peak of 1,400,000 procedures in 2006 for reasons that are not entirely clear, although millions of persons worldwide, particularly in Asia, still choose refractive surgery.1,2
There are few high-quality prospective studies of refractive surgery. Existing evidence is limited by small series, short follow-up, lack of standardized outcomes measures, lack of pre- and postoperative visual symptom comparisons, and continually changing technology. Overall, there is general agreement that refractive surgery is safe and effective.3 However, because of various persistent adverse effects, certain individuals should approach these procedures with caution. In addition, younger patients may not fully consider the possibility of long-term issues, such as changes in visual stability.
Although most patients are satisfied with the outcomes following LASIK surgery, a small number are not.3,4 The determinants of both satisfaction and dissatisfaction are highly subjective and unpredictable. Most studies reporting on subjective complaints lack objective data concerning persistently bothersome symptoms, and cannot distinguish between refractive error remaining after surgery and adverse effects of the surgery itself.3 This article updates a prior review5 and provides a framework to help patients make informed decisions.
Refractive Error and Options for Correction
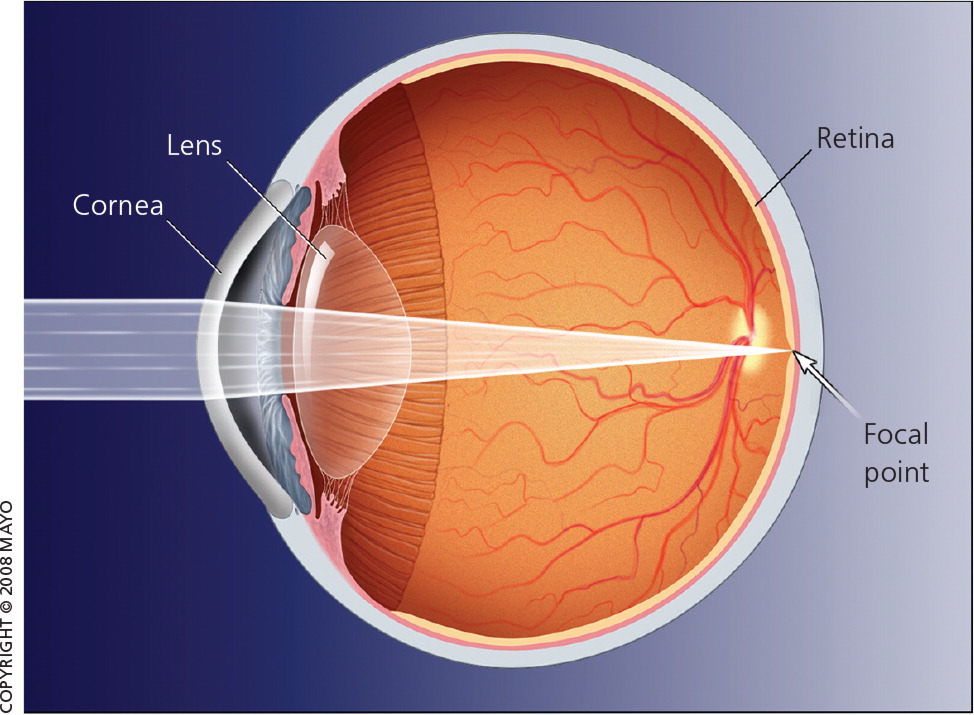
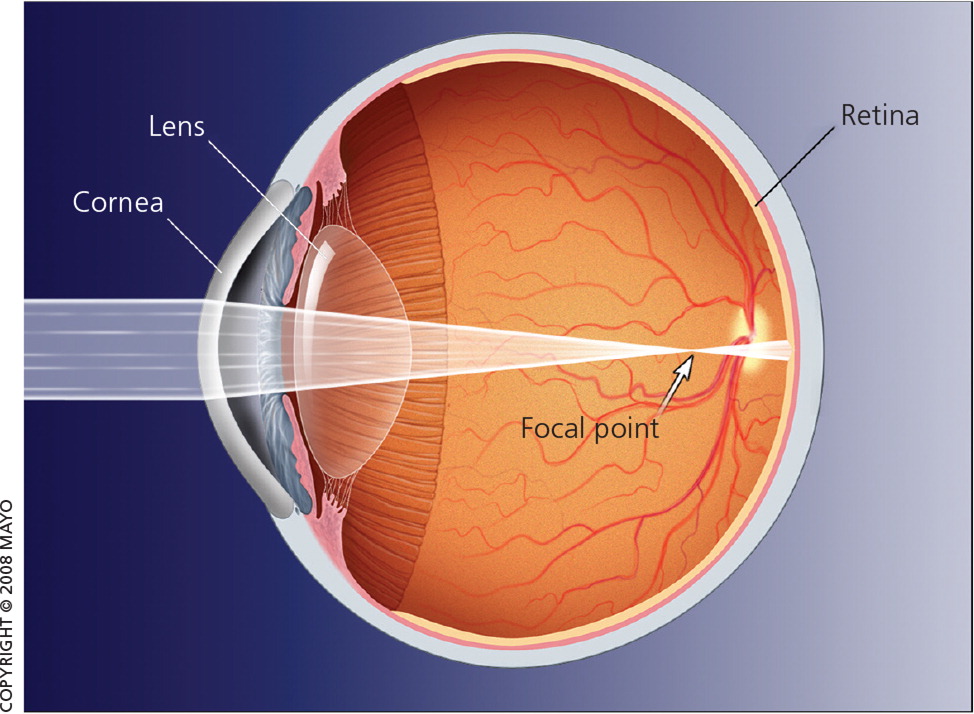
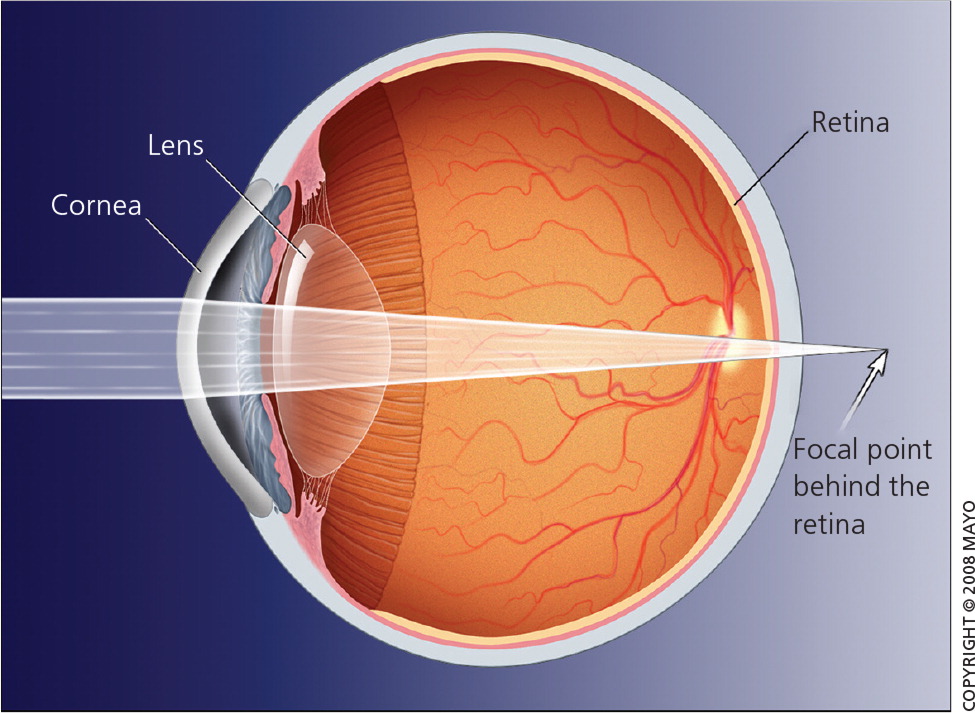
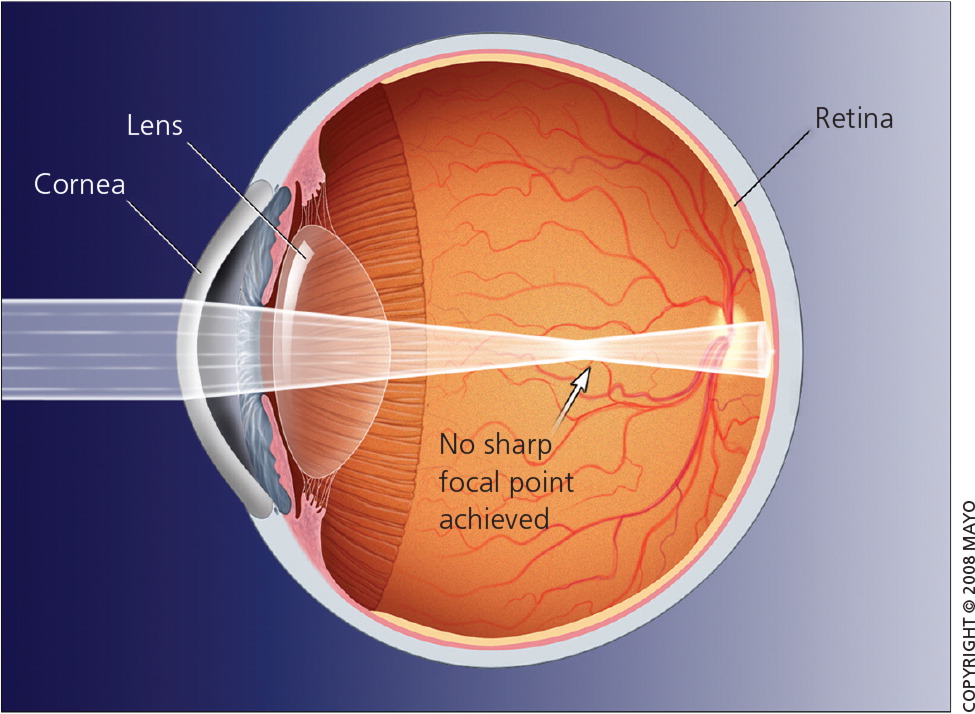
Most refractive errors are caused by a mismatch between the optics of the cornea and lens and the length of the globe. This results in images that are focused in front of the retina, causing myopia or nearsightedness, or focused behind the retina, causing hyperopia or farsightedness (Figures 1, 2, and 3).
The surface epithelium of the cornea is only a few cells thick and is continually regenerating; it maintains the tear film and provides a smooth refractive surface. The inner endothelium maintains the relative dehydration of the cornea, which is essential for clarity. The central stroma is made up of layers of collagen and accounts for 90% of overall corneal thickness. It also provides most of the structural integrity of the cornea.
Refractive surgery reshapes the cornea itself. Decreasing the curvature of the cornea by removing tissue from the center corrects for myopia. Increasing the curvature of the cornea by removing tissue from the periphery corrects for hyperopia (with somewhat less predictable results). Astigmatism (Figure 4) is caused by distortions on the corneal surface. It is corrected by removing variable amounts of tissue at different points.
In all types of refractive surgery, the thicker, structural, corneal stroma is reshaped, most commonly using a pulsatile (excimer) laser to remove a preprogrammed amount of tissue from the anterior surface. Variations in how the epithelium is managed distinguish the different procedures (Table 1).5–11
| Surface ablation | |
| PRK | |
| Epithelium is pushed or scraped aside and must regrow; moderately significant pain, tearing, photophobia, and blurred vision for the first three to four days | |
| Epithelial LASIK | |
| Epithelium is removed in a thin flap using a blade (epikeratome) and may be replaced or discarded; more corneal stroma to work with than LASIK; less pain than PRK | |
| LASEK | |
| Epithelium is removed using alcohol; more corneal stroma to work with than LASIK; less pain than PRK | |
| Stromal flap | |
| LASIK | |
| Epithelium supported by a thin layer of underlying stroma is removed in a flap (originally with a microkeratome) produced by a cutting laser (femtosecond); less pain than PRK | |
| Lenticule extraction | |
| FLEx | |
| Femtosecond laser cuts a lens-shaped segment (lenticule) within the corneal stroma, removed through a LASIK-like flap | |
| SMILE | |
| Similar to FLEx, but the lenticule is extracted through a small laser-cut incision on the edge of the cornea | |
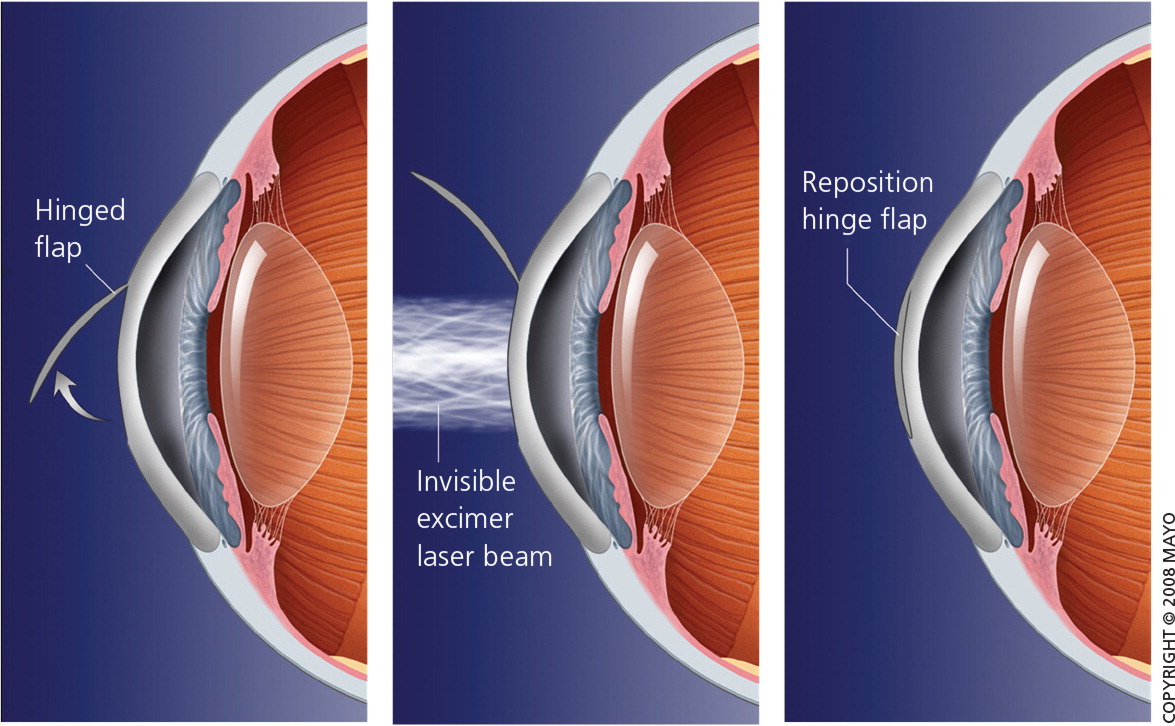
With LASIK (Figure 5), a flap about the size of a contact lens and consisting of epithelium supported by a thin layer of underlying stroma is formed using a special type of cutting laser (femtosecond laser). The flap is folded back into place and reattaches to the corneal surface spontaneously.
With photorefractive keratectomy, instead of forming a flap, the epithelium is scraped away to access the stroma. Essentially a large corneal abrasion is created; therefore, patients will have moderate pain and blurred vision for three to four days until it heals.
Compared with surface ablation procedures, LASIK results in less pain, less haze, and faster recovery and stabilization of vision, and is a better option for correcting high myopia.6 Because no flap is raised with photorefractive keratectomy, it is theoretically safer for individuals at risk of eye trauma (e.g., athletes, police officers), but no real advantages over LASIK have been demonstrated.6
Other procedures, including laser-assisted subepithelial keratomileusis, epithelial LASIK, femtosecond laser extraction, and small incision lenticule extraction, have been developed and are continually being refined. There is fair evidence that they have similar effectiveness, but specific differences and long-term outcomes are unclear.7,8,12
Intraocular lenses, which are routinely implanted following cataract extraction, have occasionally been used as an alternative to LASIK in patients with severe myopia, with the natural lens left in place. Although two published reviews concluded that this resulted in better outcomes, the evidence was of low quality, did not address long-term safety, and should not be generalized to routine practice.13,14
Patient Selection, Precautions, and Contraindications
Patients should have realistic expectations about the quality of vision that can be achieved with LASIK. For instance, vision after the procedure may not match the clear, crisp vision that rigid gas permeable contact lenses provide. Even though the overall dependence on corrective lenses will be markedly reduced, many patients still require glasses or contact lenses after LASIK, particularly in low-light conditions and as they age.3–5
Because eyesight continues to change at least into adolescence, patients must be 18 years of age (preferably older) with stable vision for at least one year to be a candidate for LASIK. Refraction may also change or fluctuate in patients who are pregnant and lactating, who have uncontrolled diabetes mellitus, or who are using high-dose steroids. Refractive surgery should be deferred in these patients. Patients with more extreme refractive errors, preexisting dry eye, or corneal irritation may have more postoperative symptoms. Table 2 includes the selection criteria for LASIK and photorefractive keratectomy.5,11,15
| Age 18 years or older |
| Stable refraction for at least one year |
| Astigmatism no worse than 5 D |
| Hyperopia no worse than +6 D |
| Myopia no worse than −12 D |
Although there are relatively few absolute contraindications to refractive surgery (mainly serious, uncontrolled eye diseases), there are many conditions that warrant caution (Table 3).5,11,15 It is not always possible to identify the occasional patient who might have poorer outcomes or unexpected complications.
| Absolute contraindications |
| Corneal abnormalities (e.g., keratoconus, thin cornea, corneal ulceration) |
| External eye disease (e.g., blepharitis, atopy/allergy, dry eye syndromes) |
| Pregnancy, lactation |
| Significant cataract |
| Uncontrolled diabetes mellitus |
| Uncontrolled glaucoma |
| Uncontrolled systemic autoimmune disease (e.g., sicca syndromes) |
| Unrealistic patient expectations |
| Possible contraindications (consider with caution) |
| Abnormal wound healing (e.g., keloids) |
| Controlled diabetes |
| Glaucoma |
| History of herpetic keratitis |
| Systemic autoimmune disease (e.g., sicca syndromes) |
Preoperative Evaluation
Use of contact lenses must be discontinued (one to two weeks for soft lenses, and three to four weeks for hard lenses) so that the corneal surface can stabilize, allowing for accurate preoperative measurements. The surgical team, led by an ophthalmologist, is responsible for the preoperative evaluation and measurements, patient selection, and counseling. Participating optometrists should not act individually but be well integrated into the team.16 A separate preoperative medical evaluation beyond the surgical team’s assessment is not necessary for refractive surgery or cataract surgery.17
Outcomes and Complications
A recent review, aggregating data from 97 major LASIK studies of the past decade, confirms excellent safety and effectiveness of refractive surgery, although there are still limited data about the long-term stability of correction.3 The FDA-initiated Patient-Reported Outcomes with LASIK (PROWL) studies provide the best data on subjective symptoms; although common in the first several months after surgery, relatively few patients considered them to be highly bothersome or persistent.18 Table 4 includes the frequency of potential LASIK complications.5,11,18
| Complication | Frequency (%) | Comment |
|---|---|---|
| Dry eye | 20 to 40 | Peaks at three months, resolves by six to 12 months |
| Persistent dry eye | 2 to 3 | Symptoms considered particularly bothersome |
| Visual symptoms (glare, halos, starbursts, reduced contrast sensitivity) | 20 | Less than 1% reported “a lot of difficulty” in general with usual activities |
| Diffuse lamellar keratitis | 2 to 4 | Epithelial disruption from debris at edge of flap; also called Sands of Sahara |
| Epithelial ingrowth | 1 to 3 | Self-limited; may need laser to treat ectopic cells |
| Flap wrinkles | 0.2 to 4 | — |
| Free cap | 0.1 to 1 | — |
| Infection (bacterial, fungal) | 0.1 | Usually resolves with treatment |
| Other vision-threatening conditions | 0.1 | — |
VISUAL ACUITY AFTER REFRACTIVE SURGERY
With current technology and appropriate patient selection, 98% of patients achieve at least 20/40 uncorrected visual acuity, which is adequate to pass a driver’s license eye examination without glasses. More than 90% achieve 20/20 uncorrected visual acuity.18
Outcomes are often reported in terms of diopters (D) within the intended, or target, correction. Corrections within 0.5 D are achieved in more than 90% of patients after LASIK, and almost all others achieve correction within at least 1 D.3,4 Patients are less likely to notice discrepancies of less than 0.5 D, although 1 D is noticeable in most situations (glasses are refracted to within 0.25 D). With current technologies, very few patients will require a second procedure to achieve satisfactory results.4,18 Table 5 shows the expected visual acuity with LASIK.3,4,11,18
| UCVA of 20/20 | UCVA of 20/40 | Predictable correction within 0.5 D | Predictable correction within 1 D | Patient satisfaction |
|---|---|---|---|---|
| > 90% | 98% | > 80% | > 95% | 97% |
DRY EYE
Postoperatively, 20% to 40% of patients report symptoms such as dry eye, burning, itching, discomfort, or ocular surface dryness. These symptoms typically peak in intensity around three months after the procedure and usually resolve after six to 12 months. Up to 20% of patients have persistent symptoms, although only 2% to 3% considered them to be bothersome.3,4,18,19
The cause of dry eye symptoms is multifactorial and varies among individuals. Some of these symptoms, particularly when more persistent or severe, may be manifestations of corneal neuropathy.20 Patients with other chronic pain syndromes (e.g., fibromyalgia, irritable bowel syndrome, migraine) report more dry eye symptoms pre- and postoperatively than those without these conditions,21 and should perhaps be more wary of refractive surgery, especially if it is being considered because of contact lens intolerance.
VISUAL SYMPTOMS
Various visual symptoms, such as a glare, halos, starbursts, and reduced contrast sensitivity, affected up to 20% of patients in the PROWL studies. These symptoms were especially bothersome when patients were driving at night. Less than 1% reported “a lot of difficulty” in general with usual activities.18
Considerations for the Aging Eye
With all refractive surgery procedures, postoperative visual acuity seems to be generally stable over the first two to five years, typically with less than 1 D of refractive regression. Stability over longer periods has not been well studied.24
Postoperative visual acuity is typically measured with ideal lighting and does not necessarily predict whether glasses will be needed for routine activities, such as night driving, especially in older individuals. It is not known whether dry eye or visual symptoms will become more troublesome as the patient ages.
PRESBYOPIA AND READING GLASSES
Although refractive surgery can improve near vision in patients with hyperopia, it does not correct presbyopia in older patients. Although everyone develops presbyopia as they age, those with myopia (who have often required many years of correction for distance vision) generally need little, if any, correction for reading or other near vision activities. However, if these same individuals undergo refractive surgery at any age, they will eventually need reading glasses as they get older. The idea that the need for reading glasses will be greater, rather than less, with age is counterintuitive for many patients. This must be thoroughly explained to patients before refractive surgery.3,4,11
CATARACTS AND INTRAOCULAR LENSES
Older patients with early cataracts may elect to have them removed and their vision corrected with intraocular lenses rather than undergoing LASIK. Some patients may be candidates for monovision, in which the dominant eye is corrected for distant vision and the nondominant eye is corrected for near vision (anisometropia). Older patients may be somewhat more tolerant of anisometropia, but this is unpredictable. Physicians should first try contact lenses of different corrections, gradually increasing the discrepancy between eyes, to see if this is acceptable to the patient.
The effect of prior refractive surgery on measurements of corneal curvature (keratometry) must be taken into account when calculating intraocular lens parameters before cataract surgery years later. Ideally, preoperative measurements should be obtained from the refractive surgeon and retained for future reference.
GLAUCOMA
Prior refractive surgery may result in falsely low or inconsistent intraocular pressure readings, making them less reliable for the early diagnosis of glaucoma.23 Closer long-term monitoring, with optic disk examinations and visual field testing, may be advisable when diagnostic accuracy of readings is in question.
Shared Decision Making
COST CONSIDERATIONS
Refractive surgery is not covered by insurance, and fees vary by market region, the specific procedure, technology used, and surgeon. The cost ranges from approximately $1,500 to $2,500 per eye.27,28 A second enhancement procedure or other services may not be included in the basic charge. With cataract surgery, Medicare pays for only the most basic intraocular lenses. Surgeons are allowed to “balance bill” for more advanced intraocular lenses, and patients’ out-of-pocket costs may be higher than they expected.
Ophthalmic surgeons often have a direct financial interest in performing refractive eye surgery, including covering the cost of laser equipment. Although this usually is not a problem, patients need to be aware of this in the process of shared decision making.
CHOOSING A SURGEON
There is no evidence that patients ask about surgical training, experience, and equipment when choosing a surgeon or facility, or that these questions result in better outcomes. As with any other specialized decision, asking for a recommendation from an ophthalmologist the family physician knows and trusts is the best way to identify a surgeon who will put the needs of the patient first and with whom the patient feels comfortable.
PATIENT SATISFACTION AND PREFERENCES
Overall, most patients report satisfaction with refractive surgery, although patients have differing levels of satisfaction with similar vision correction, and some individuals may be less tolerant of discomfort and inconvenience. These subjective differences cannot be reliably predicted.
In the PROWL studies, 93% of patients were completely or very satisfied, 2% were dissatisfied with the LASIK procedure itself, and 3% were dissatisfied with their vision after LASIK. Although 10% of patients reported that they were only somewhat satisfied, 97% of patients reported that, in retrospect, they would still have the procedure.3,4,18 Most patients probably decide to have refractive surgery based on personal preferences, and are influenced by marketing or the experiences of others.29 Unbiased patient information is available,27,30,31 as are two LASIK decision aids, which have been independently evaluated.32–34 These decision aids can be accessed at https://decisionaid.ohri.ca/.
Even family physicians who may not support refractive surgery for vision correction because of concerns about complications and uncertain long-term outcomes can help patients make informed decisions. Ultimately, the patient and physician should assess the necessity, safety, and risk of elective refractive surgery together, using their own preferences, values, and experiences, in the shared decision making process.
Data Sources: We searched PubMed and Google Scholar using the search terms refractive surgery, laser eye surgery, LASIK, PRK, LASEK, IOL alone and in combination with the terms quality of life, decision aids, and decision making. We examined clinical trials, meta-analyses, review articles, and selected case series, as well as the bibliographies of selected articles. Cochrane and Essential Evidence Plus were also searched. We reviewed selected patient and consumer websites. Search dates: November 2015 and May 2016.
