A more recent article on lower extremity abnormalities in children is available.
Am Fam Physician. 2017;96(4):226-233
Author disclosure: No relevant financial affiliations.
Leg and foot problems in childhood are common causes of parental concern. Rotational problems include intoeing and out-toeing. Intoeing is most common in infants and young children. Intoeing is caused by metatarsus adductus, internal tibial torsion, and femoral anteversion. Out-toeing is less common than intoeing and occurs more often in older children. Out-toeing is caused by external tibial torsion and femoral retroversion. Angular problems include genu varum (bowleg) and genu valgum (knock knee). With pes planus (flatfoot), the arch of the foot is usually flexible rather than rigid. A history and physical examination that include torsional profile tests and angular measurements are usually sufficient to evaluate patients with lower extremity abnormalities. Most children who present with lower extremity problems have normal rotational and angular findings (i.e., within two standard deviations of the mean). Lower extremity abnormalities that are within normal measurements resolve spontaneously as the child grows. Radiologic studies are not routinely required, except to exclude pathologic conditions. Orthotics are not beneficial. Orthopedic referral is often not necessary. Rarely, surgery is required in patients older than eight years who have severe deformities that cause dysfunction.
Parents commonly seek medical advice because of concerns about the appearance of their child's lower extremities, feet, or gait.1,2 Most concerns are normal variations of growth and development and are best managed with parental reassurance.1 Common normal variants of the lower extremities in children include rotational problems such as intoeing and out-toeing, angular problems such as genu varum (bowleg) and genu valgum (knock knee), and pes planus (flatfoot).
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Radiography is not needed in the initial evaluation to differentiate normal variations in childhood limb development from pathologic lower extremity abnormalities. | C | 2–7, 9, 12 |
| The physical examination for lower extremity abnormalities should include measurements of height and weight with growth percentiles; inspection of the face, skin, and neurologic system; and focused musculoskeletal examination, including torsional profile and angular measurements. | C | 3–6 |
| Discussions with parents should focus on the natural course of lower extremity abnormalities and include reassurance; most rotational and angular concerns resolve spontaneously if measurements are within two standard deviations of the mean. | C | 1–5, 12, 18–21, 25–28, 30, 31 |
| Lower extremity rotational and angular abnormalities that are two standard deviations outside the mean or that persist beyond the expected age of resolution should be referred to an orthopedic surgeon. | C | 3, 5, 11, 21, 25–28 |
| Orthotics are not effective in the treatment of lower extremity rotational and angular abnormalities. | C | 3–5, 20 |
| Adjustable shoes are effective for the treatment of metatarsus adductus in prewalking infants with motivated parents and are less expensive than serial casting. | B | 10, 14, 16, 17 |
| Adolescents with rigid or symptomatic flexible pes planus should receive imaging of the feet and referral to a podiatrist or orthopedist. | C | 6, 22–24 |
History and Physical Examination
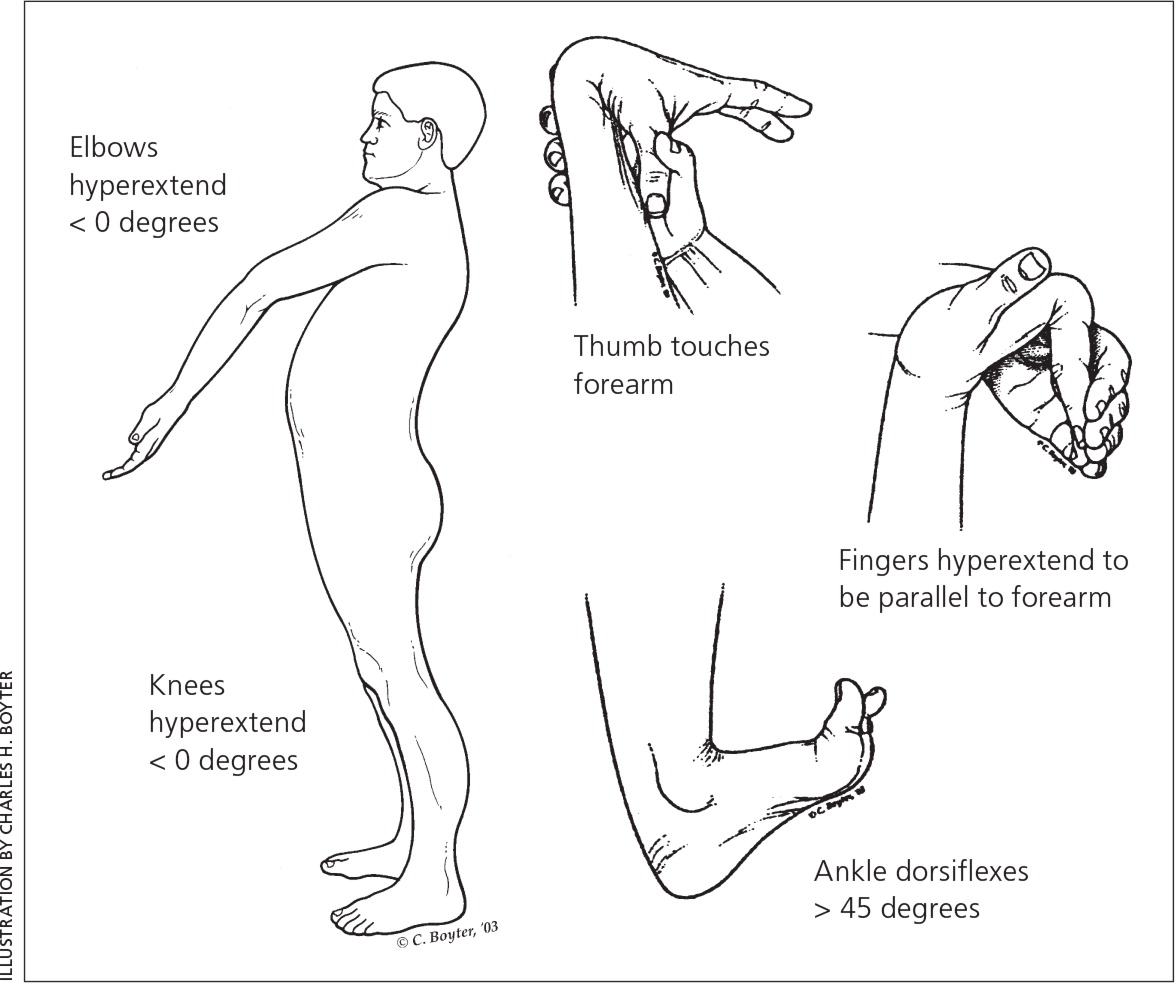
A comprehensive history and physical examination (Table 13,4 and Table 24–6 ) are often sufficient to differentiate normal variations in limb development from pathologic abnormalities, without the need for radiography.3–5 For the physical examination, the lower extremities should be fully exposed, and the child may need to wear shorts, a diaper, underwear, or a gown.4–6 The child's height and weight with growth percentiles should be reviewed because normal growth reduces the likelihood of systemic conditions.5 The musculoskeletal examination should include evaluation for hip dysplasia, leg length discrepancy, and joint laxity (Figure 15 ); assessment of passive range of motion and rotational positioning of the lower extremities (i.e., torsional profile); and a gait analysis (Figure 25 ).
| Understand parental concerns: gait, function, appearance, duration, and progression |
| Patient history: prenatal and birth history, developmental milestones |
| Family history: complete orthopedic family history of pathologic rotational or angular deformities and interventions required |
| Signs/symptoms: gait problems, issues wearing shoes, limping, tripping, falling |
| Sitting habits: the W sitting position (Figure 8) is common in children with increased femoral anteversion; however, there is no evidence that sitting habits cause or worsen orthopedic lower extremity problems |
| Component | Findings | Possible diagnosis |
|---|---|---|
| Screening examination | ||
| Height and weight | Plot on appropriate Centers for Disease Control and Prevention or World Health Organization growth chart | Abnormal measurements may suggest pathologic conditions (e.g., rickets, metabolic bone disease) |
| Facial appearance | Abnormal facies | Genetic disorders |
| Skin | Warmth or redness | Septic arthritis |
| Ecchymosis | Fracture, nonaccidental trauma | |
| Masses; sacral pits, dimples, hair patch; congenital lesions (e.g., café au lait spots) | Spina bifida, neurofibromatosis | |
| Spine | Flexion and extension of the spine | Scoliosis, lordosis, dorsal kyphosis |
| Neurologic | Neurologic abnormalities | Developmental delay |
| Focused musculoskeletal examination | ||
| Torsional profile (Figure 5) | External and internal hip rotation (Figure 3) | Measurements more than 2 standard deviations outside the mean may suggest femoral anteversion or retroversion, or internal or external tibial torsion |
| Thigh-foot angle (Figure 4) | ||
| Angular measurements | Intercondylar distance: with medial malleoli touching, measure distance between the femoral condyles | Measurements more than 2 standard deviations outside the mean may suggest genu varum or valgum |
| Intermalleolar distance: with femoral condyles touching, measure distance between the medial malleoli in sitting position | ||
| Evaluation for limb asymmetry and joint laxity | Measure leg lengths for asymmetry | Asymmetry may be due to contracture, cerebral palsy, perinatal stroke, intracranial mass, neuromuscular disorder, fracture, or septic joint |
| Assess range of motion (Figure 1) | Joint laxity can mimic or worsen torsional or angular deformities and contributes to pes planus, hip dysplasia, and dislocated patella | |
| Foot | Heel bisector line (Figure 6) | Metatarsus adductus |
| Lateral C shape, tight heel cord | ||
| Gait analysis | Observe child standing for loss of medial foot arch | Pes planus |
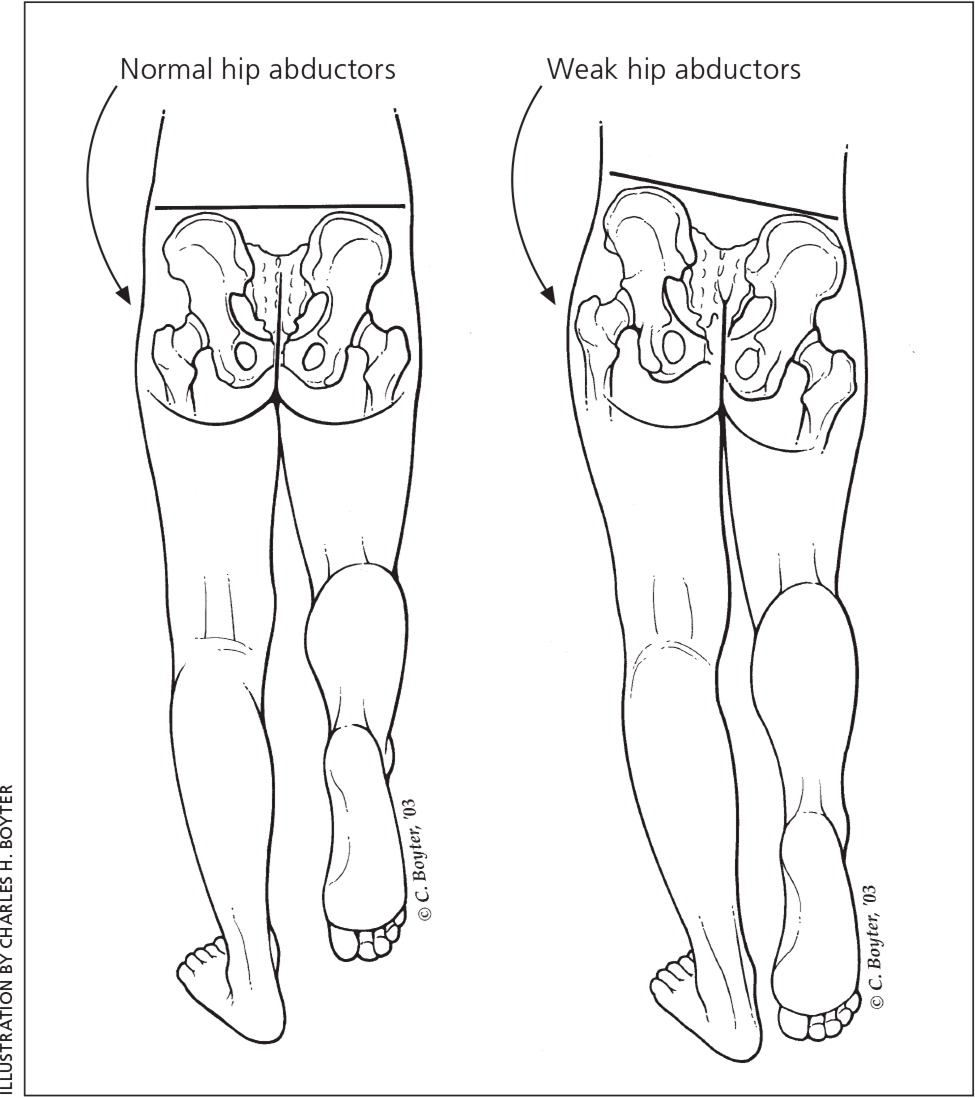
| Trendelenburg sign (Figure 2) | Hip dysplasia, leg length discrepancy | |
| Observe child's gait for intoeing and out-toeing, and measure foot progression angle: apply dusted chalk or sanitizing gel to child's bare feet, have child walk on strips of examination paper | Internal or external tibial torsion, femoral anteversion or retroversion | |
| Assess for W sitting position (Figure 8) | Femoral anteversion | |
Torsional profile, a key component of the musculoskeletal examination, includes foot progression angle, internal and external hip rotation (Figure 37 ), and thigh-foot angle (Figure 43,7 ). Figure 5 provides normal ranges for torsional profile measurements.8 Measurements outside these ranges indicate a pathologic condition.3–5,7
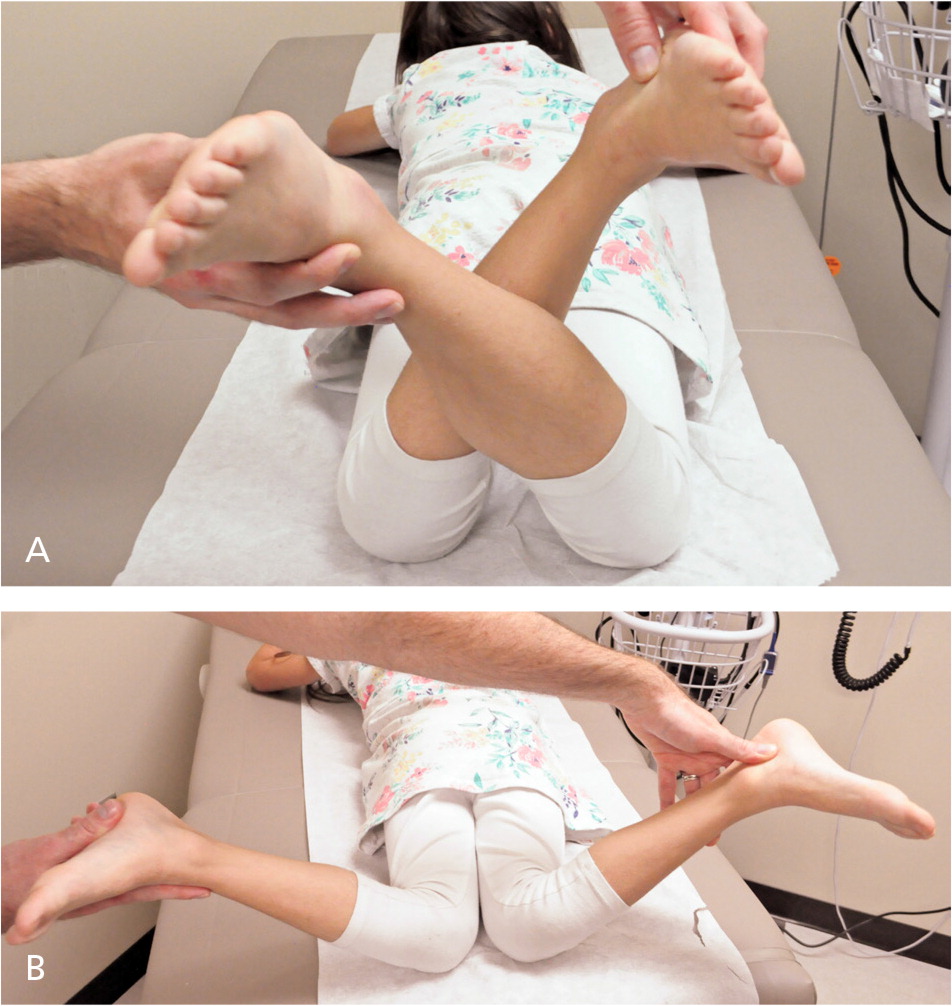

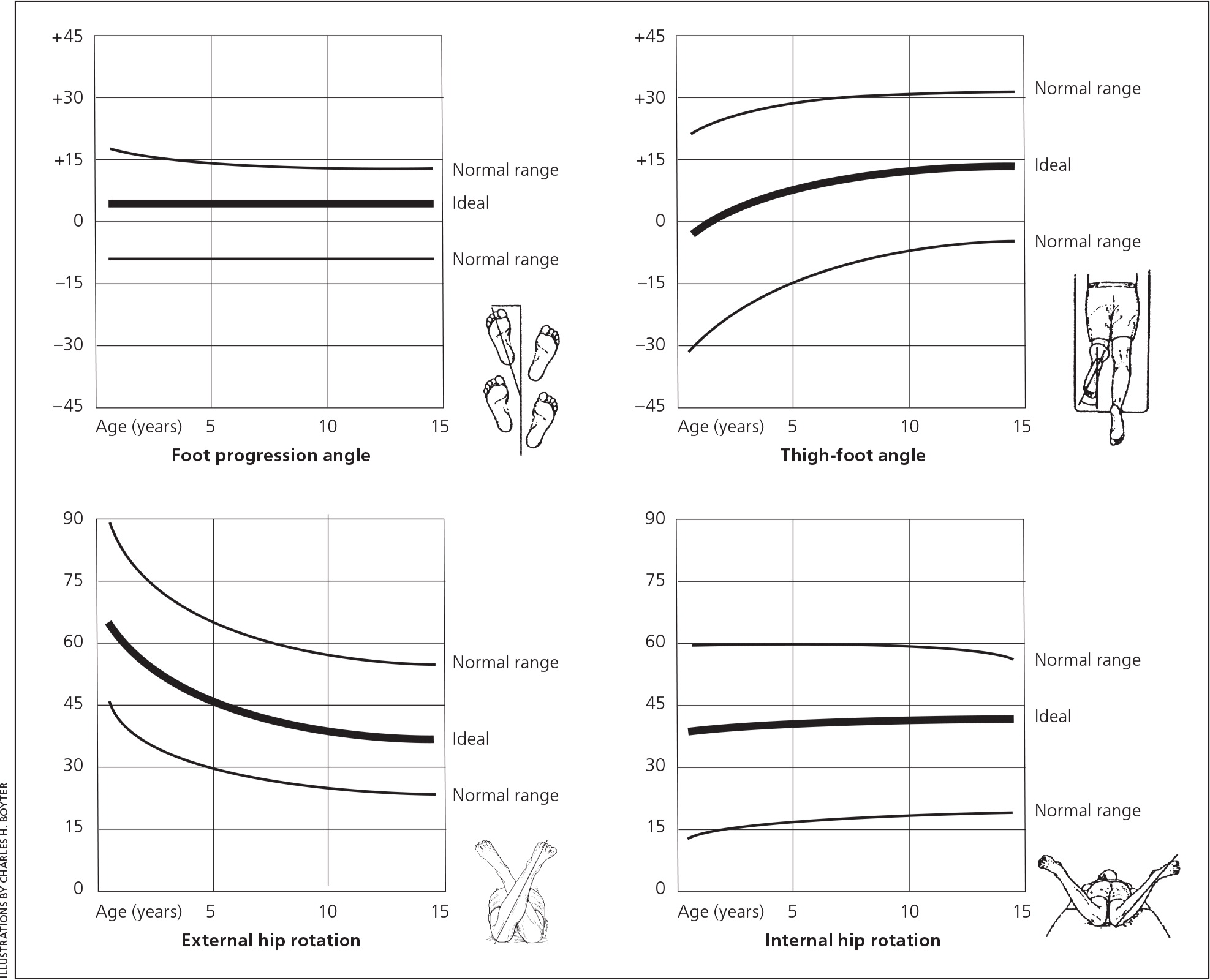
Foot progression angle measurements will have positive values with out-toeing and negative values with intoeing.4,5 Evaluation of hip rotation shows increased internal rotation with femoral anteversion and increased external rotation with femoral retroversion.3,4 Thigh-foot angle testing is positive for tibial torsion when the foot turns in relative to the thigh axis.9
Clinical Conditions
Lower limb abnormalities in children can be grouped broadly into three categories: rotational, angular, and foot variations (eTable A).
| Condition | Epidemiology | Common features | Diagnostic measurements | Management |
|---|---|---|---|---|
| Rotational | ||||
|
|
|
|
|
|
|
|
| |
|
|
|
| |
|
|
|
| |
|
|
|
| |
|
|
|
| |
|
|
|
| |
| Angular | ||||
|
|
|
| |
|
|
|
| |
| Foot | ||||
|
|
|
| |
INTOEING
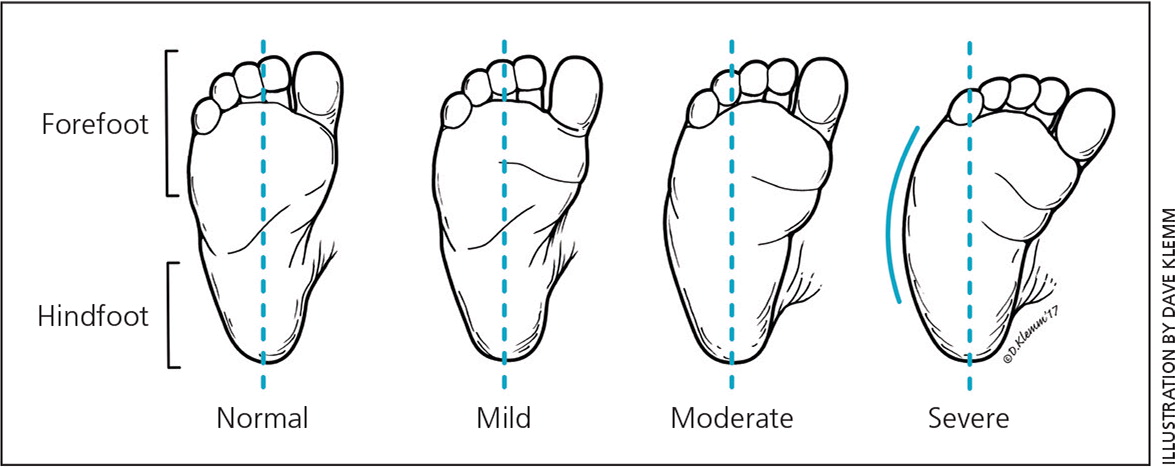
Metatarsus Adductus. Metatarsus adductus is the most common congenital foot abnormality and usually resolves spontaneously by one year of age.13 Physical examination reveals medial deviation of the forefoot relative to a normal hind-foot, lack of a tight heel cord, a convexity or C shape of the lateral aspect of the foot, and a concave medial border of the foot3,12 (Figure 7). Severity is determined by the heel bisector line. The foot should be assessed for flexibility to rule out rigid deformities (e.g., metatarsus varus). Treatment is based on severity and age.12 Flexible metatarsus adductus does not require treatment.14,15 Severe metatarsus adductus and rigid deformities are treated with serial casting.3,5 Adjustable shoes are effective in prewalking infants who have motivated parents and are less expensive than serial casting.14,16,17

Rigid metatarsus adductus is ideally treated with serial casting. This is most feasible in children who are not yet walking. Older children or those with persistent symptomatic metatarsus adductus resistant to casting may require surgery if the deformity causes significant dysfunction. Surgery for metatarsus adductus has high failure and complication rates, and thus casting or adjustable shoes are generally attempted first, before the child starts walking. Casting in older children who are walking is often not a feasible option, and surgical consultation may be appropriate to discuss risks and benefits of surgery. Most cases of persistent metatarsus adductus are still asymptomatic in adulthood, and surgery is rarely indicated.3,4,12,18
Internal Tibial Torsion. Internal tibial torsion is a common normal rotational variant.3,19 It is the most common cause of intoeing,5,6 usually presenting in toddlers. The child walks with patellae facing forward and feet pointing inward, producing an internally rotated thigh-foot angle and negative foot progression angle on torsional profile.4,5 Internal tibial torsion usually resolves spontaneously by five years of age.4 Braces, night splints, shoe modification/wedges, other orthotics, and serial casting are not recommended for this condition.3 Residual internal tibial torsion has not been shown to cause degenerative joint disease or disability and, thus, surgery is rarely indicated.3,4 Surgery may be considered in patients older than eight years who have a severe residual deformity (thigh-foot angle more than three standard deviations above the mean [i.e., greater than 15 degrees internal rotation]) and severe functional or cosmetic abnormality that is not expected to self-correct.3,18,20
Femoral Anteversion. Femoral anteversion is the most common cause of intoeing in school-aged children and is most severe between four and seven years of age.3,19,20 Physical examination focuses on assessment of internal and external rotation of the hip. Increased internal rotation (60 to 90 degrees) with reduced external rotation (10 to 15 degrees) is diagnostic of femoral anteversion. The patellae and feet appear to point inward (known as squinting or kissing patellae), resulting in a clumsy, circumduction gait.4,5,12 Children with femoral anteversion often sit in the W position (Figure 8) for comfort rather than sitting cross-legged.4,12 Spontaneous resolution occurs in more than 80% of children by eight years of age.4,5,12 Special shoes, braces, connective bars, and other orthotics are not effective.3–5,12,21 Surgical intervention is indicated for children older than eight years with severe functional or cosmetic abnormality secondary to persistent femoral anteversion greater than 50 degrees and internal rotation greater than 80 degrees.4,12

OUT-TOEING
External Tibial Torsion. External tibial torsion usually presents between four and seven years of age when the tibia externally rotates during normal growth and worsens into a deformity. Physical examination reveals a positive foot progression angle and a thigh-foot angle greater than 30 degrees3,4 (Figure 9). Surgery to correct external tibial torsion is rarely recommended before 10 years of age, but may be performed to prevent disability from patellofemoral syndrome and knee joint instability. Surgery can have a high complication rate.3,4,11

Femoral Retroversion. Femoral retroversion is common in newborns because of contracture of the hip from intrauterine positioning.5,9,11 It is diagnosed when the feet of a prewalking child are rotated outward by nearly 90 degrees (i.e., Charlie Chaplin appearance).5,9,11 There is a markedly decreased hip internal rotation and increased external rotation on torsional profile.3,4
Femoral retroversion typically improves during the first year of walking.9 Persistence after three years of age warrants radiography of the pelvis, hips, and lower extremities and referral to an orthopedist.11 If femoral retroversion is diagnosed after eight years of age, it may be associated with a slipped capital femoral epiphysis.3,11 Femoral retroversion results in osteoarthritis and increased risk of lower extremity stress fracture.11 Surgical consultation should be considered for children with persistent femoral retroversion at three years of age5; however, the average age for surgical correction with osteotomy is 10 years of age.3,11
Pes Planus. Pes planus, or flatfoot, is the absence of the medial longitudinal arch on weight bearing and presence of the arch with tiptoeing3 (Figure 10). Physiologic flatfoot that is flexible is a benign, normal variant.6,22,23 Pathologic flatfoot is rigid and requires orthopedic referral.6,22,23 Physiologic flatfoot is observed in nearly all infants, 45% of preschool-aged children, and about 15% of persons older than 10 years.6,24 Most children with physiologic flatfoot are asymptomatic and develop an arch before 10 years of age.3,23 Painless, flexible flat-foot does not require investigation or intervention.3,6,22,23 Orthotics such as special shoes and insoles are not effective for painless pes planus.3,6,22,23 Pes planus should be distinguished from tarsal coalition in adolescents.3,23 On examination, limited movement of the subtalar joint and absence of the medial arch with tiptoeing suggest tarsal coalition, which requires further investigation with oblique radiography or computed tomography.3,23

Surgical consultation is recommended for patients with tarsal coalition and symptomatic pes planus (rigid type and flexible type with persistent pain and dysfunction despite previous nonoperative treatments). Nonoperative treatments for symptomatic flexible pes planus include rest, activity modification, massage, physical therapy, and a trial of a nonsteroidal anti-inflammatory drug. Although orthotics are ineffective at altering the course of flexible flatfoot, they may provide relief of pain when present and may also be tried before surgical management.22
ANGULAR VARIATIONS
During childhood, knee alignment changes with skeletal growth and development. At birth, most newborns have physiologic genu varum.4 This gradually progresses to a neutral position by two years of age and then to physiologic genu valgum between three and six years of age. By seven to 11 years, most children's knees return to a neutral or slightly valgus position. Girls tend to have more valgus positioning than boys.25–28
Parental concerns for knee misalignment are often because of appearance, awkward gait, or clumsiness. Normal, transient physiologic angulation should be distinguished from pathologic processes. Evaluation of standing knee alignment includes the intercondylar and intermalleolar distances, and the tibiofemoral angle measured with a goniometer.4,26 Severe deformity, unilateral or asymmetric presentation, and concerns for metabolic or endocrine disorders warrant further workup.
Genu Varum. Genu varum (Figure 11) is typically bilateral, symmetric, and self-limited. Bracing, connective bars, and other orthotics are not necessary for most patients. Persistence after two years of age is unusual. Adolescents who participate in high-impact sports may develop genu varum.29 Pathologic genu varum may be due to rickets, skeletal dysplasia, or Blount disease (abnormal growth of medial proximal tibial physis that is associated with obesity).4,30,31

Genu Valgum. Genu valgum commonly occurs between three and six years of age and is self-limited. Onset in adolescence is unusual and warrants investigation. Pathologic causes of genu valgum include trauma or fracture, prior osteomyelitis, and possibly obesity.32
Treatment of Angular Variations. Pathologic genu varum and valgum may be associated with early osteoarthritis.29,32 Surgical correction of genu varum and valgum is reserved for when the condition does not spontaneously resolve, conservative measures are ineffective, or there is extreme angulation. Surgical techniques attempt to realign the bone or reorient bone growth.33
This article updates a previous article on this topic by Sass and Hassan.5
Data Sources: A PubMed search was completed using Clinical Queries and the Therapy Narrow Filter with the terms pediatric, lower extremity abnormality, lower extremity variant, metatarsus adductus, genu valgum, genu varum, tibial torsion, angular deformity, intoeing, and out-toeing. The search included randomized controlled trials, clinical trials, and reviews. Also searched were Essential Evidence Plus and the Cochrane Database of Systematic Reviews. Search dates: December 2015 to February 2016, and April 2017.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army Medical Department or the U.S. Army Service at large.