
Am Fam Physician. 2017;96(7):453-461
Patient information: See related handout on underlying causes of high blood pressure, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Most patients with hypertension have no clear etiology and are classified as having primary hypertension. However, 5% to 10% of these patients may have secondary hypertension, which indicates an underlying and potentially reversible cause. The prevalence and potential etiologies of secondary hypertension vary by age. The most common causes in children are renal parenchymal disease and coarctation of the aorta. In adults 65 years and older, atherosclerotic renal artery stenosis, renal failure, and hypothyroidism are common causes. Secondary hypertension should be considered in the presence of suggestive symptoms and signs, such as severe or resistant hypertension, age of onset younger than 30 years (especially before puberty), malignant or accelerated hypertension, and an acute rise in blood pressure from previously stable readings. Additionally, renovascular hypertension should be considered in patients with an increase in serum creatinine of at least 50% occurring within one week of initiating angiotensin-converting enzyme inhibitor or angiotensin receptor blocker therapy; severe hypertension and a unilateral smaller kidney or difference in kidney size greater than 1.5 cm; or recurrent flash pulmonary edema. Other underlying causes of secondary hypertension include hyperaldosteronism, obstructive sleep apnea, pheochromocytoma, Cushing syndrome, thyroid disease, coarctation of the aorta, and use of certain medications.
Secondary hypertension is a type of hypertension with an underlying and potentially reversible cause. It makes up only a small fraction (5% to 10%) of hypertensive cases.3–5 The prevalence of secondary hypertension varies by age and is more common in younger persons, with a prevalence close to 30% in those 18 to 40 years of age with hypertension.3 Extensive testing for secondary hypertension is not warranted in all patients with hypertension because of cost, low yield, and the potential for false-positive results; however, testing is recommended in patients younger than 30 years.6,7
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| In the absence of clinical signs to suggest possible secondary hypertension in adults, indications for further evaluation include resistant hypertension and early, late, or rapid onset of high blood pressure. | C | 3 |
| Preadolescent children with hypertension should be evaluated for possible secondary causes. | C | 16 |
| Young adults thought to have secondary hypertension should be assessed for fibromuscular dysplasia of the renal artery with magnetic resonance angiography or computed tomography angiography. | C | 43 |
| The aldosterone-to-renin ratio is the best initial test to determine whether a patient with hypertension should have further evaluation for hyperaldosteronism. | C | 24 |
| Patients who are obese and who have signs or symptoms of obstructive sleep apnea and hypertension should be assessed with polysomnography. | C | 51 |
| Recommendation | Sponsoring organization |
|---|---|
| Do not screen for renal artery stenosis in patients without resistant hypertension and with normal renal function, even if known atherosclerosis is present. | Society for Vascular Medicine |
General Approach to the Patient and Identifying Potential Causes of Secondary Hypertension
Secondary hypertension should be considered in the presence of suggestive signs and symptoms such as severe or resistant hypertension, onset before 30 years of age (especially before puberty), malignant or accelerated hypertension, and an acute rise in blood pressure from previously stable readings (Table 1).3,7–17 Figure 1 provides a suggested approach to the initial evaluation of patients with suspected secondary hypertension.10
| Acute rise in blood pressure in a patient with previously stable readings3,8,9 |
| Age of onset before puberty10 |
| Age younger than 30 years in nonobese, nonblack patients with no family history of hypertension9 |
| Malignant or accelerated hypertension (with signs of end-organ damage)11 |
| Severe (systolic blood pressure > 180 mm Hg and/or diastolic blood pressure > 120 mm Hg) or resistant hypertension; resistant hypertension is defined as hypertension that persists despite three adequate antihypertensive medications, including one diuretic, in accordance with guidelines from the 8th Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure3,8,12,13 |
Accurate measurement of blood pressure, including the use of a correctly sized and appropriately positioned blood pressure cuff, is the most critical aspect of the diagnosis of hypertension.3 At least two or three blood pressure readings taken on two separate visits are recommended to make the diagnosis.18 For patients who have blood pressure variability or possible white coat hypertension, 24-hour ambulatory blood pressure monitoring is recommended.
It also is important to review the patient's diet and medication use for other potential causes of elevated blood pressure. A list of drug classes and common examples to be considered as a cause of hypertension is provided in Table 2.3,10,14,20,21 Excessive consumption of sodium (2.4 g or more per day),3 licorice (3 g or more per day),22 or alcohol (300 g or more per week)20 is known to increase blood pressure.14,20 Of note, licorice is commonly found in chewing tobacco and licorice root tea.
| Drug class | Common examples |
|---|---|
| Anti-infective | Ketoconazole |
| Anti-inflammatory | Cyclooxygenase-2 inhibitors, nonsteroidal anti-inflammatory drugs |
| Chemotherapeutic | Vascular endothelial growth factor inhibitors |
| Herbal | Ephedra, ginseng, ma huang |
| Illicit | Amphetamines, cocaine |
| Immunosuppressive agents | Cyclosporine (Sandimmune), sirolimus (Rapamune), tacrolimus (Prograf) |
| Psychiatric | Buspirone (Buspar), carbamazepine (Tegretol), clozapine (Clozaril), lithium, monoamine oxidase inhibitors, selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants |
| Sex hormones | Estrogen and progesterone in oral contraceptives; androgens |
| Steroid | Methylprednisolone, prednisone |
| Sympathomimetic | Decongestants, diet pills |

| Signs/symptoms | Possible secondary hypertension cause | Diagnostic test options |
|---|---|---|
| Increase in serum creatinine concentration of at least 50% (≥ 0.5 to 1 mg per dL [44 to 88 μmol per L]) after starting angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | Renal artery stenosis | CT angiography |
| Moderate to severe hypertension and unilateral small kidney/recurrent flash pulmonary edema | Doppler ultrasonography of renal arteries | |
| Renal bruit | Magnetic resonance angiography with gadolinium contrast media | |
| Elevated serum creatinine | Renal diseases | Estimated glomerular filtration rate |
| Proteinuria | Renal ultrasonography | |
| Hypokalemia | Primary hyperaldosteronism | Renin and aldosterone levels to calculate aldosterone-to-renin ratio |
| Apneic episodes during sleep | Obstructive sleep apnea | Polysomnography (sleep study) |
| Daytime sleepiness | Sleep Apnea Clinical Score with nighttime pulse oximetry | |
| Snoring | ||
| Flushing | Pheochromocytoma | 24-hour urinary fractionated metanephrines and normetanephrines |
| Headaches | Plasma free metanephrines | |
| Labile blood pressures | ||
| Orthostatic hypotension | ||
| Palpitations | ||
| Sweating | ||
| Syncope | ||
| Arm to leg systolic blood pressure difference > 20 mm Hg | Coarctation of the aorta | Magnetic resonance/CT angiography (adults) |
| Delayed or absent femoral pulses | Transthoracic echocardiography (children) | |
| Murmur | ||
| Buffalo hump | Cushing syndrome | 24-hour urinary free cortisol |
| Central obesity | Late-night salivary cortisol | |
| Moon facies | Low-dose dexamethasone suppression | |
| Striae | ||
| Bradycardia/tachycardia | Thyroid disorders | Thyroid-stimulating hormone |
| Cold/heat intolerance | ||
| Constipation/diarrhea | ||
| Irregular, heavy, or absent menstrual cycle |
Common Causes of Secondary Hypertension
Likely etiologies of secondary hypertension are different in children compared with adults. A summary of the most common causes of secondary hypertension by age is provided in Table 4.4,10,14,29 Preadolescent children with hypertension should be evaluated for possible secondary hypertension.16 Across all adult ages, renovascular hypertension, renal disease, aldosteronism, and obstructive sleep apnea (OSA) represent the most common causes of secondary hypertension.30
| Age groups | Percentage of patients who have hypertension with an underlying cause | Most common etiologies† |
|---|---|---|
| Children (birth to11 years) | 70 to 85 | Renal parenchymal disease |
| Coarctation of the aorta | ||
| Adolescents (12 to 18 years) | 10 to 15 | Renal parenchymal disease |
| Coarctation of the aorta | ||
| Young adults (19 to 39 years) | 5 | Thyroid dysfunction |
| Fibromuscular dysplasia | ||
| Renal parenchymal disease | ||
| Middle-aged adults (40 to 64 years) | 8 to 12 | Hyperaldosteronism |
| Thyroid dysfunction | ||
| Obstructive sleep apnea | ||
| Cushing syndrome | ||
| Pheochromocytoma | ||
| Older adults (65 years and older) | 17 | Atherosclerotic renal artery stenosis |
| Renal failure | ||
| Hypothyroidism |
RENOVASCULAR HYPERTENSION
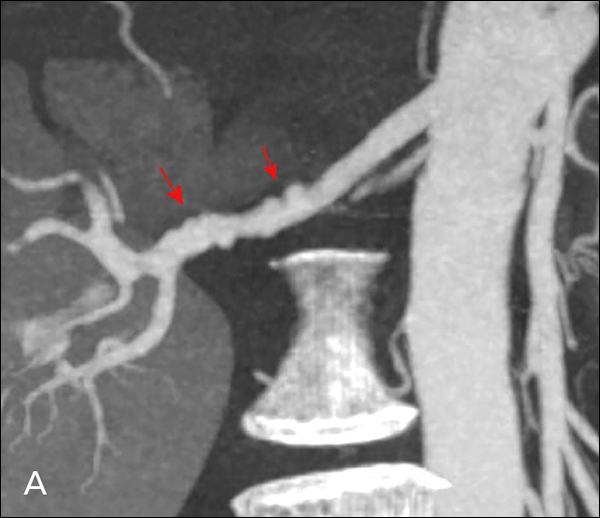
Renovascular hypertension is a common, potentially reversible cause of secondary hypertension. Although it may contribute to only 1% of mild hypertension cases, it accounts for 10% to 45% of severe or malignant hypertension cases in white patients.29,31 Renovascular hypertension often is found in patients with coronary or peripheral atherosclerosis, including renal artery stenosis (RAS).3,31,32 In young adults, especially women, renovascular hypertension can be caused by fibromuscular dysplasia (Figure 233 ). For patients with signs of possible renovascular hypertension, the American College of Cardiology/American Heart Association recommends considering diagnostic testing if they are healthy enough and willing to undergo revascularization32 (Table 53,32,34–37 ).
| Increase in serum creatinine concentration of at least 50% occurring within one week of initiating angiotensin-converting enzyme inhibitor or angiotensin receptor blocker therapy 3 |
| Onset of severe hypertension in patients older than 55 years (e.g., ≥ 180 mm Hg systolic and/or 120 mm Hg diastolic) |
| Renal bruit (associated with only a 40% sensitivity and 99% specificity)34 |
| Severe hypertension in patients with a unilateral smaller kidney or difference in kidney size of > 1.5 cm |
| Severe hypertension in patients with known atherosclerosis |
| Severe hypertension in patients with recurrent flash pulmonary edema32 |
Randomized controlled trials have shown that medical therapy is equal to revascularization, with similar rates of blood pressure control and cardiovascular deaths, and without the associated complications of surgery.34,38–41 Noting that most studies have concentrated on patients with less severe atherosclerotic RAS, a systematic review was unable to determine whether revascularization or medical management is preferable.42 Because revascularization remains a treatment option for patients with hypertension related to fibromuscular dysplasia and possibly for those with rapidly declining renal function, detection of RAS is important in these groups.36,43
The preferred imaging method for patients who have suspected RAS is controversial. Although the diagnostic standard is angiography, the technique is invasive and should not be used as an initial diagnostic test. Doppler ultrasonography is inexpensive and has a 75% sensitivity and a 90% specificity,44 although magnetic resonance angiography (MRA) with gadolinium contrast media and computed tomography (CT) angiography are equally accurate in visualizing stenosis and give better sensitivity, specificity, and anatomic detail than Doppler ultrasonography.23,44 Accurate assessment with standard noninvasive techniques, such as Doppler ultrasonography, can be limited because they provide only indirect evidence of the presence of RAS; however, invasive techniques, although more accurate, have the potential of nephrotoxicity. A glomerular filtration rate must be calculated and patients must be counseled on the risks of nephrotoxicity when physicians order contrast CT angiography or MRA with gadolinium. Alternatively, a captopril renal isotope nuclear scan is noninvasive, with a 90% sensitivity and specificity.45 Invasive imaging should be pursued only in patients who would consider intervention, whether surgical or radiographic.
Patients with RAS should be treated with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers unless there are contraindications to their use. In RAS secondary to fibromuscular dysplasia, the cure rates for angioplasty and surgery are 36% and 54%, respectively.43 Young adults thought to have secondary hypertension should be assessed for fibromuscular dysplasia of the renal artery with MRA or CT angiography.43
RENAL DISEASES
Hypertension can be a major cause of renal failure in older adults, which in turn leads to worsening hypertension.12 Secondary hypertension in these cases is suggested by an elevated serum creatinine level or proteinuria on urinalysis. Renal parenchymal disease is the most common cause of hypertension in preadolescent children. In this age group, causes of secondary hypertension include glomerulonephritis, congenital abnormalities, and reflux nephropathy. Renal ultrasonography should be the first choice of imaging in this age group.
PRIMARY HYPERALDOSTERONISM
Once thought to be rare, primary hyperaldosteronism is now considered one of the more common causes of secondary hypertension. Primary hyperaldosteronism is excess production of aldosterone independent of the renin-angiotensin system and is caused by an adrenal adenoma, unilateral or bilateral adrenal hyperplasia, or adrenocortical carcinoma. Hyperaldosteronism also can be secondary to excessive growth hormone, as in acromegaly. Hypokalemia due to urinary potassium wasting is the most prominent feature of hyperaldosteronism. However, one-half of patients with hyperaldosteronism have a normal potassium level.46 The prevalence of hyperaldosteronism in patients with hypertension is 6%.47
Hyperaldosteronism is the most common cause of drug-resistant hypertension.48 If hypokalemia is found, the next step is a urinary potassium test. The best initial test for primary hyperaldosteronism is measurement of the ratio of the plasma aldosterone concentration to plasma renin activity after potassium repletion.23 The aldosterone-to-renin ratio is the most sensitive test to detect primary hyperaldosteronism because approximately 25% of patients with the condition have normal aldosterone levels. The ratio should be measured in the morning two hours after waking and in the upright position; abnormal test results should prompt referral to an endocrinologist.23 This is the best initial test to determine whether a patient with hypertension should have further evaluation for hyperaldosteronism.24
Agents that may affect the aldosterone-to-renin ratio should be discontinued four weeks before testing, including nonsteroidal anti-inflammatory drugs, aldosterone antagonists (spironolactone and eplerenone [Inspra]), amiloride (Midamor), triamterene (Dyrenium), potassium-wasting diuretics, and licorice. If the ratio is normal, it may be necessary to withdraw other antihypertensives that can interfere with the aldosterone-to-renin ratio two weeks before testing. These antihypertensives include beta blockers, central alpha2 agonists, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, renin inhibitors, and dihydropyridine calcium channel blockers. If it is necessary to maintain hypertensive control, other less-interfering agents can be started, such as extended-release verapamil, hydralazine, prazosin (Minipress), doxazosin (Cardura), or terazo-sin.24 Inappropriate elevation of aldosterone is common in patients who are obese.30 After the diagnosis of primary hyperaldosteronism has been confirmed by demonstrating inappropriate aldosterone secretion, adrenal CT should be performed.24
OBSTRUCTIVE SLEEP APNEA
OSA is a leading treatable cause of secondary hypertension.3,49,50 OSA is common in men 40 to 59 years of age who are obese and who snore, leading to apneic episodes.29 Other symptoms include headache, fatigue, daytime somnolence, confusion, difficulty concentrating, depression, personality changes, hypertension, and cardiac arrhythmias. Patients who are obese and who have signs or symptoms of OSA and hypertension should be assessed with polysomnography.51 Although polysomnography is the standard diagnostic test, clinical assessment tools (e.g., Epworth Sleepiness Scale [https://www.aafp.org/afp/2009/0301/p391.html#afp20090301p391-f1], Sleep Apnea Clinical Score)52,53 with nighttime pulse oximetry may be sufficient for the diagnosis of moderate to severe OSA.25,51 Patients with OSA retain sodium and do not respond to hypertensive medication.54 They also lose the normal circadian rhythm in blood pressure, thus 24-hour ambulatory measurements are often needed to detect nighttime increases that will not be noted in the office.55 Treatment of OSA may improve blood pressure control, sleep quality, daytime sleepiness, and mortality.56
Uncommon Causes of Secondary Hypertension
PHEOCHROMOCYTOMA
Pheochromocytoma should be suspected when there are paroxysmal elevations in blood pressure. Other symptoms include the classic triad of headache, palpitations, and sweating.57 Because pheochromocytoma is rare, only patients with these symptoms or adrenal incidentaloma should be evaluated for pheochromocytoma.4 The investigation of adrenal incidentaloma is important because there are associated cardiovascular sequelae, and the hypertension is largely reversible with treatment. Testing for pheochromocytoma can be done by measuring metanephrines in a 24-hour urine sample or by measuring plasma free metanephrines, followed by CT if results are abnormal.26
CUSHING SYNDROME
Cushing syndrome has classical features of moon facies, central obesity, proximal muscle weakness, and ecchy-mosis. Most cases are iatrogenic from prescribed corticosteroids. Only 20% of patients with iatrogenic Cushing syndrome have hypertension.28 Although tumors causing Cushing syndrome are rare, 80% or more of these patients develop hypertension.28 Evaluation for Cushing syndrome should be done only if there are suggestive symptoms or if adrenal incidentaloma is suspected. First-line testing for Cushing syndrome includes any two of the following: 24-hour urinary free cortisol, low-dose dexamethasone suppression, or late-night salivary cortisol tests. If any test result is abnormal or if there is a high suspicion of Cushing syndrome despite normal results, referral to an endocrinologist is needed.28
COARCTATION OF THE AORTA
Coarctation of the aorta is a common cause of secondary hypertension in children, especially males, but may not be detected until adulthood because it is often asymptomatic.58 Classic signs of coarctation of the aorta include upper extremity hypertension, delayed or decreased femoral pulses (brachial-femoral delay) and low or unobtainable blood pressure in the lower extremities, and murmur.13 In younger patients with coarctation of the aorta, chest radiography may be nonspecific, whereas in adults, the classic figure three sign or rib notching may be evident. Transthoracic echocardiography is sufficient for diagnosing coarctation of the aorta in children, although MRA is the preferred imaging method in adults.16,59 Surgery is recommended for those with a transcoarctation pressure gradient of more than 30 mm Hg.57
THYROID AND PARATHYROID DISEASE
Hypothyroidism can cause an elevation in diastolic blood pressure, whereas hyperthyroidism can cause an elevation of systolic blood pressure, leading to a widened pulse pressure.9 As thyroid disease occurs across the age spectrum, testing for hypo- and hyperthyroidism should be considered if there are any suggestive symptoms of either condition. Thyroid-stimulating hormone is a sensitive marker used for the initial diagnosis of hypo- or hyperthyroidism. Primary hyperparathyroidism, diagnosed by unexplained hypercalcemia, can affect vascular reactivity, circadian blood pressure rhythm, and renal function.
CHEMOTHERAPEUTIC AGENTS
| Chemotherapeutic agent | Description |
|---|---|
| Alkylating agents | Antineoplastic agent |
| Anti–vascular endothelial growth factor signaling | Anticancer therapy (hypertension should be considered as a class effect; the incidence of hypertension is dose related and aggravates preexisting hypertension in those with risk factors) |
| Bevacizumab (Avastin) | Metastatic cancers of the colon, rectum, kidney, and breast; glioblastoma multiforme |
| Cis-diamminedichloro-platinium | Antineoplastic agent (only during intra-arterial administration) |
| Paclitaxel | Antineoplastic agent |
| Sorafenib (Nexavar) | Approved for advanced renal cell carcinoma and hepatocellular carcinoma |
| Sunitinib (Sutent) | Advanced gastrointestinal stromal tumor and renal cell carcinoma |
ORAL CONTRACEPTIVES
Oral contraceptives can raise blood pressure within the normal range but can also cause secondary hypertension.20,21,60 Hypertension is induced in 5% of patients taking combined oral contraceptives with at least 50 mcg of estrogen and 1 to 4 mg of progestin. Risk factors for secondary hypertension with oral contraceptive use include pregnancy-induced hypertension, a family history of hypertension, smoking, black race, obesity, increased body mass index, renal disease, and diabetes mellitus.20
This article updates a previous article on this topic by Viera and Neutze.10
Data Sources: Nine databases were identified and searched, including Medline, PubMed, PsycINFO, Biomedical Reference Collection, CINAHL, Health Source: Nursing/Academic, Psychology and Behavioral Sciences Collection, iMediSearch, and Essential Evidence Plus. Key words: hypertension, secondary hypertension, resistant hypertension, and malignant hypertension. Search dates: December 7, 2015, and February 15, 2017.
The authors thank Peter Tian, MD, for reviewing the manuscript.
