
Am Fam Physician. 2018;98(4):251-252
Author disclosure: No relevant financial affiliations.
A 56-year-old white man with dark hair and blue eyes presented for his annual physical examination. His medical history was significant for type 2 diabetes mellitus, hypertension, hyperlipidemia, and primary hypothyroidism.
The physical examination revealed multiple nevi on his back and a nontender, ulcerated lesion on his left upper arm (Figure 1). It was heterogeneous in color with irregular borders and measured 1.5 × 1.5 × 2.5 cm. The examination findings were otherwise normal.

Question
Discussion
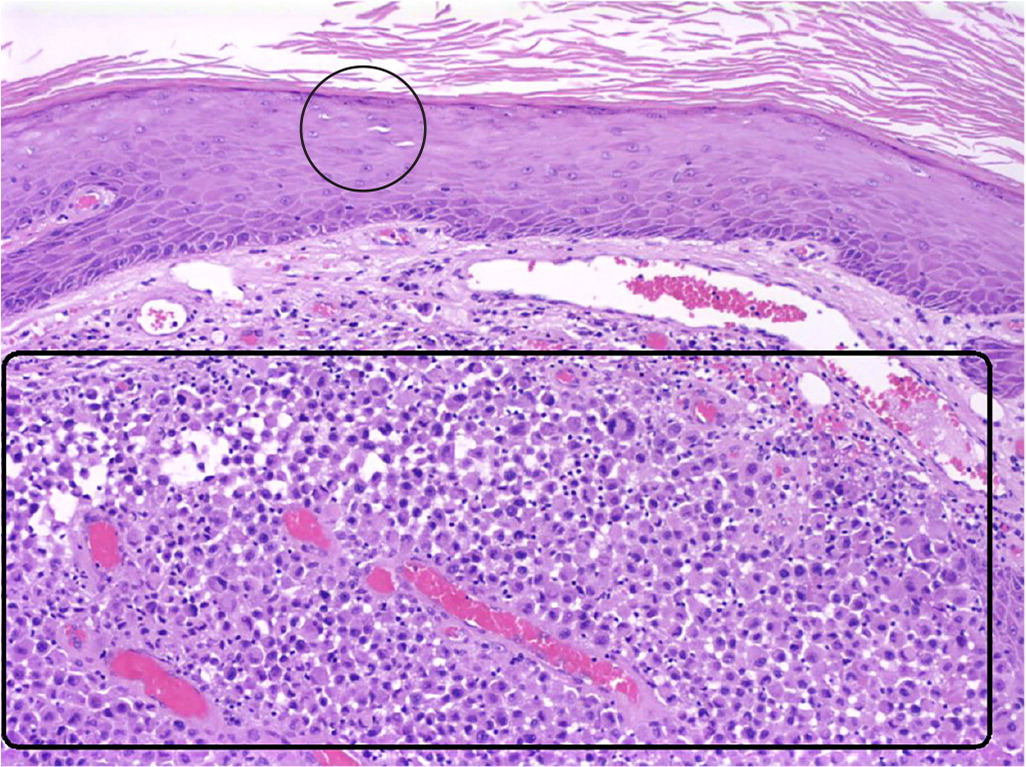
The answer is B: nodular malignant melanoma. This is a vertical growth phase melanoma that accounts for 15% to 30% of all melanomas.1 A nodular melanoma is typically more than 2 mm thick and appears as a darkly pigmented, pedunculated or polypoid nodule that may be ulcerated.2,3 Histologically, it appears as a rapidly mitotic pigmented dermal growth of epithelioid cells or spindlelike atypical neoplastic cells without an epidermal component (Figure 2). Nonpigmented nodular melanomas (pink lesions) often have a delayed diagnosis. It is important to recognize the “ugly duckling” lesion that might be darker or larger than the surrounding moles.2,3 Nodular melanoma is treated with surgical excision of the lesion and normal tissue margins.3
Dermatofibrosarcoma protuberans presents as an asymptomatic plaque with an indurated, flesh-colored sclerodermiform or telangiectatic lesion. It is extremely slow growing but may rarely present as an ulcerated and protuberant nodule. It is an uncommon cutaneous sarcoma with low metastatic potential but a high local recurrence rate that can be diagnosed with core needle or incisional biopsy.4
A keratoacanthoma is a 1- to 2-cm, dome-shaped or crateriform, squamoproliferative nodule with central hyperkeratosis. It is characterized by spurts of rapid growth, followed by a variable period of lesion stability and spontaneous resolution. Diagnosis is based on histopathologic and clinical findings, including inflammatory infiltrates in the dermis, epidermal hyperplasia, and “lipping” or “buttressing” of the epidermis over the rim of the central keratotic plug.5
Mycosis fungoides is typically a multifocal disease, but rare cases of solitary lesions have been reported. It presents as a single erythematous, scaly patch or plaque predominantly located on non–sun-exposed areas and is typically present for several years before diagnosis.6 Histopathologic features include dermal fibrosis, microabscesses, and hyperconvoluted dermal and epidermal lymphocytes.
Pyogenic granuloma is a benign vascular tumor of the skin that presents as a rapidly growing, red, dome-shaped, pedunculated or sessile papule that is usually less than 1 cm in size. It tends to bleed easily and has a base that is surrounded by a collarette of acanthotic epidermis.7 It may develop on a capillary vascular or arteriovenous malformation and occasionally occurs following laser treatment or cryotherapy.8 Spontaneous resolution is rare, but it can be treated with curettage and cauterization or laser therapy.
| Condition | Characteristics |
|---|---|
| Dermatofibrosarcoma protuberans | Slow-growing plaque with an indurated, flesh-colored sclerodermiform or telangiectatic lesion |
| Nodular malignant melanoma | Darkly pigmented, pedunculated or polypoid nodule that may be ulcerated; more than 2 mm thick |
| Pyogenic granuloma | Benign vascular, rapidly growing, red, dome-shaped, pedunculated or sessile papule that is usually less than 1 cm in size; bleeds easily |
| Keratoacanthoma | 1- to 2-cm, dome-shaped or crateriform, squamoproliferative nodule |
| Unilesional (solitary) mycosis fungoides | Single erythematous, scaly patch or plaque on non–sun-exposed areas; typically present for several years before diagnosis |
