
Am Fam Physician. 2019;99(4):228-236
Patient information: See related handout on hand infections, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Acute hand infections are often caused by puncture wounds and are generally classified into superficial or deep infections. Superficial infections occur in the skin and subcutaneous tissues, whereas deep infections can involve the tendon sheaths, adjacent anatomic compartments, deep fascial planes, bursae, joint spaces, and bones. Superficial hand infections are more common than deep infections and are typically managed with elevation, warm soaks, splinting in the position of function, analgesics, and empiric antibiotics when indicated. Paronychia, which can be acute or chronic, is an infection or inflammation of the nail fold. Treatment involves warm soaks, topical antibiotics, and abscess drainage, if indicated. A felon is an infection of the distal pulp of the finger. Treatment often involves surgical drainage and empiric oral antibiotics. Herpetic whitlow is caused by herpes simplex virus and typically resolves without intervention. Deep hand infections include pyogenic flexor tenosynovitis and clenched-fist bite wounds. Pyogenic flexor tenosynovitis is a rapidly progressing bacterial infection of the flexor tendon sheaths in the hand, most commonly caused by a penetrating injury to the finger. Clenched-fist bite wounds result from direct contact of the fist on incisor teeth and are associated with polymicrobial infections. Empiric antibiotics and prompt surgical consultation are indicated to reduce long-term morbidity.
The hand can easily be injured during everyday activities. Any trauma to the hand, particularly a penetrating trauma, may introduce damaging pathogens. The hand's compartmentalized anatomy may contribute to the development of an infection, and if an infection is not appropriately diagnosed and treated, significant morbidity can result.
| Recommendation | Sponsoring organization |
|---|---|
| Avoid antibiotics and wound cultures in emergency department patients with uncomplicated skin and soft tissue abscesses after successful incision and drainage and with adequate medical follow-up. | American College of Emergency Physicians |
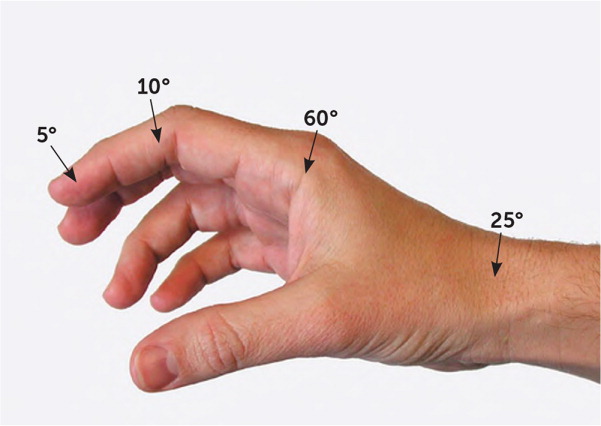
Some general wound care principles apply to all hand infections.1 Initial nonsurgical management of superficial infections includes rest, elevation, and splint immobilization in the position of function (Figure 1).1 Splints are indicated for rest and prevention of flexion contractures, elevation reduces edema, and warm compresses improve blood flow and antibiotic delivery.2,3 Open wounds should be copiously irrigated with tap water or saline, and abscesses should be drained.4–6 Surgical debridement may be necessary to remove necrotic tissue that is not adequately removed by irrigation.7 Several studies have failed to show that the addition of povidone-iodine or other antibacterial solutions are more beneficial than saline alone.8,9
More severe infections, such as deep hand infections, require early surgical intervention and oral or parenteral antibiotics.1,4 Selection of empiric antibiotics depends on the type and severity of the infection, host factors, and local antibiotic resistance patterns (Table 1).1,3,8,10–23 Anti-tetanus immunoglobulin, plus tetanus and diphtheria toxoids (Td) or the tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine, should be administered per recommendations from the Advisory Committee on Immunization Practices (i.e., administer if the patient has not had a tetanus toxoid–containing vaccine in the past five years).24
| Condition | Common pathogens | Management recommendations |
|---|---|---|
| Superficial hand infections | ||
| Acute paronychia1,8,10–15 | Staphylococcus aureus and other streptococci are most common Pseudomonas, gram-negative bacilli (e.g., Proteus), and anaerobes from exposure to oral flora Opportunistic infections in immunocompromised patients | Conservative therapy (elevation, warm soaks, splint in functional position [Figure 1]) for simple, early, uncomplicated infections without abscess Topical antibiotics: gentamicin, mupirocin (Bactroban), or topical fluoroquinolones Incision and drainage in patients with obvious fluid collection and when conservative management is ineffective Oral antibiotics for seven to 10 days (typically not indicated; limit use to immunocompromised or severely ill patients): trimethoprim/sulfa-methoxazole, cephalexin (Keflex), amoxicillin/clavulanate (Augmentin), or clindamycin |
| Felon1,3,12,14–16 | S. aureus and other streptococci | Conservative therapy (warm soaks and elevation) and oral antibiotics (seven to 10 days of trimethoprim/sulfamethoxazole, cephalexin, amoxicillin/clavulanate, or clindamycin) for early infections without abscess formation Incision and drainage for infections with abscess; leave packing in place for 24 to 48 hours, then daily dressing changes to allow for healing by secondary intent |
| Herpetic whitlow1,3,16–18 | Herpes simplex virus types 1 and 2 | Supportive therapy is mainstay of treatment (coverage with dry dressing to prevent spread) Incision and drainage are contraindicated Consider antivirals (acyclovir, famciclovir [Famvir], or valacyclovir [Valtrex]) if infection has been present less than 48 hours, if lesion is recurrent, or in immunocompromised patients Consider antibiotics to cover skin flora if secondary bacterial infection is suspected or abscess is confirmed by ultrasonography |
| Deep hand infections | ||
| Pyogenic flexor tenosynovitis1,3,8,14–16 | S. aureus, including methicillin-resistant S. aureus, and other streptococci are most common Disseminated Neisseria gonorrhoeae or Candida albicans in people who are sexually active, immunocompromised, and have no history of injury Mixed anaerobic and aerobic oral pathogens in injection drug users | Start parenteral antibiotics: vancomycin, daptomycin (Cubicin), linezolid (Zyvox), telavancin (Vibativ), or clindamycin In injection drug users, treat suspected polymicrobial infection with broad-spectrum parental antibiotics (e.g., β-lactamase inhibitor); consider gentamicin; common empiric regimen is vancomycin plus piperacillin/tazobactam (Zosyn) Inpatient admission with early surgical consultation for incision and drainage with immediate catheter irrigation of the sheath if presenting more than 24 hours from symptom onset or if no improvement in 12 to 24 hours of parental antibiotics plus symptomatic treatment (splinting, elevation, heat) Occupational therapy after surgical treatment |
| Clenched-fist bite wound1,16,19–23 | S. aureus, other streptococci, Eikenella corrodens, gram-negative bacilli, anaerobes | Surgical consultation is indicated Wounds should be explored, copiously irrigated, and surgically debrided Inpatient management is generally recommended; outpatient management is reasonable when presenting less than 24 hours after injury with no signs of infection; oral empiric antibiotics with next-day follow-up is advised Outpatient antibiotics: amoxicillin/clavulanate, fluoroquinolones, doxycycline, trimethoprim/sulfamethoxazole; avoid monotherapy with first-generation cephalosporins, macrolides, and aminoglycosides Inpatient treatment with broad-spectrum parental antibiotics: ampicillin/sulbactam (Unasyn), piperacillin/tazobactam, ticarcillin/clavulanate (Timentin), or ceftriaxone plus metronidazole (Flagyl) |
Management of Specific Conditions
Acute hand infections are grouped broadly into two categories: superficial and deep infections. Table 2 lists the differential diagnosis for acute hand infections and common noninfectious mimickers.10,16,25–39 eTableA provides links to previous American Family Physician articles that include more details about related topics.
| Condition | Characteristics |
|---|---|
| Superficial infections | |
| Acute paronychia | Acute inflammation of the nail fold, with or without abscess; redness, swelling, and tenderness of the nail fold with possible fluctuance |
| Felon | Distal digital pulp infection presenting with throbbing pain, tense swelling, and erythema of the finger pad distal to the distal interphalangeal joint |
| Herpetic whitlow | Herpes simplex virus infection of the distal finger presenting with vesicles of clear fluid on an erythematous base; usually resolves spontaneously |
| Lymphangitis | Inflammation of the lymphatic system, often from bacterial causes, resulting in linear erythematous streaking proximally from the source25 |
| Subcutaneous abscess | Erythema, warmth, edema, and pain of superficial skin; induration is often present26 |
| Deep infections | |
| Animal bite | Animal bites involving the hands should be allowed to heal by secondary intent, and prophylactic antibiotics should be given; all cat bites are at high risk of infection27 |
| Candida | Most common cause of fungal infection in immunocompromised people; skin manifestations can present as multiple macules, papules, or pustules with erythematous border28 |
| Clenched-fist bite wound | 3- to 5-mm laceration over the metacarpophalangeal joint or proximal interphalangeal joint, often sustained from contact of the fist on incisor teeth29 |
| Deep space abscess | Involvement of the thenar space, midpalmar space, Parona space, or the interdigital web spaces of the hand; usually arises from direct inoculation or contiguous spread; marked swelling of the hand may occur; ultrasonography or magnetic resonance imaging may help differentiate from superficial infection16 |
| Necrotizing fasciitis | Presents as rapidly spreading cellulitis, edema, erythema, “shiny skin,” and bullae; gas in tissue may be evident on physical examination or imaging16,30 |
| Neisseria gonorrhoeae | Common cause of arthritis in sexually active people; skin lesions including petechiae, macules, papules, pustules, and vesicles are present in 75% of patients with bacteremia; can be asymmetric31 |
| Osteomyelitis | Rare cause of hand infections; usually arises after trauma or from contiguous spread; often presents late after inciting factor; radiographic changes may include osteopenia, osteosclerosis, and periosteal reactions32 |
| Pyogenic flexor tenosynovitis | Closed-space infection of the flexor tendon sheath, usually from a penetrating finger injury; characterized by four Kanavel signs (Table 3) |
| Septic joint | Typically results from penetrating injuries or contiguous spread; presents as a painful, swollen, and erythematous joint; passive and active range of motion is painful; joint aspiration reveals more than 50,000 white blood cells (more than 75% are polymorphonuclear lymphocytes)16 |
| Noninfectious etiologies (including mimickers) | |
| Acute calcific tendinitis | Deposition of calcium around the tendons presenting with pain, swelling, erythema, and tenderness over the affected tendon; fever, lymphadenopathy, and elevated inflammatory markers are absent; radiography shows homogenous calcific densities over tender areas33 |
| Chronic paronychia | Results from repeated irritant dermatitis after nail barrier disruption; usually involves multiple digits with duration of at least six weeks; physical findings include nail dystrophy and possible absence of cuticle10 |
| Contact/irritant dermatitis | Localized pruritic eczematous eruption after contact with allergen or irritant34 |
| Crystalopathies (e.g., gout, pseudogout) | Painful, swollen, and erythematous joint with crystals on joint aspiration; commonly occurs in first metatarsophalangeal joint35 |
| Dyshidrotic eczema | Chronic or recurrent vesicular eruption on the palms, soles, and interdigital areas; can be associated with pain, pruritus, and burning34 |
| Foreign body reaction | Granuloma formation in response to foreign material penetrating the skin; can be asymptomatic; imaging can confirm presence and location of foreign body36 |
| Inflammatory arthritis | Joint swelling, erythema, prolonged morning stiffness (longer than one hour), and symmetric pain, including during rest; other systemic signs may be present (e.g., rash, mucosal lesions and inflammation, Raynaud phenomenon, neurologic symptoms)37 |
| Metastatic tumor | Rare, usually involving the distal phalanx of the finger; primary lung cancer is most common; colon, kidney, breast, prostate, and thyroid cancers may also have bony metastasis to the hand; radiography can help differentiate metastatic tumors from felons38 |
| Pyogenic granuloma | Benign, rapidly growing tumor, usually yellow to purplish with tendency to bleed easily39 |
| Acute and Chronic Paronychia |
| Approach to Septic Arthritis |
| Common Questions About Wound Care |
| Diagnosis and Management of Osteomyelitis |
| Dog and Cat Bites |
| Nongenital Herpes Simplex Virus |
| Skin and Soft Tissue Infections |
SUPERFICIAL HAND INFECTIONS
Superficial infections arise from the skin and subcutaneous soft tissues located superficially to the tendons in the hand.40Superficial hand infections are more common than deep infections, with infections of the fingertip (paronychia and felon) being most common.8 Other superficial hand infections are listed in Table 2.10,16,25–39
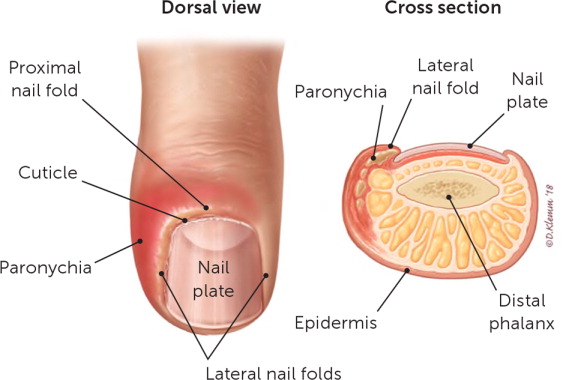
Acute Paronychia. Paronychia is inflammation of a nail fold, with or without abscess formation. Paronychia can be acute (typically limited to a single digit and caused by infection) or chronic (lasting at least six weeks, affecting multiple nails, or related to chemical irritants).1,10,11,40 Acute paronychia is caused by trauma to the nail, cuticle, or nail fold that leaves it vulnerable to bacterial invasion, infection, and inflammation. Symptoms include redness, swelling, and tenderness of the nail fold with or without pallor and fluctuance suggestive of abscess (Figure 2 and Figure 3). Risk factors include artificial nails or recent manicure, manipulating a hangnail, occupational trauma (e.g., dishwashers), ingrown nails, and nail biting or thumb-sucking.10 Staphylococcal and streptococcal species are the most common pathogens, followed by polymicrobial infections including anaerobes (more common in people with diabetes mellitus or exposure to oral flora, and in injection drug users).1,8,10,12,40,41 Pseudomonas (suggested by a discolored green nail bed) and gram-negative bacilli are rare isolates.12,42

Mild infections without obvious abscess should be treated with warm soaks and topical antibiotics.10 If an abscess is present, conservative measures to provoke spontaneous drainage may be tried for two to three days; however, mechanical drainage is often needed.8 Procedures for draining paronychia have been described in a previous American Family Physician article.10 Routine cultures for uncomplicated skin and soft tissue infections are not recommended.26,43 Oral antibiotics typically are not needed after successful drainage, but if used, they should be limited to treatment of immunocompromised or severely ill patients, based on local community resistance patterns and established guidelines.10,12,14,26
Felon. A felon is a subcutaneous infection within the fleshy part of the fingertip, known as the distal digital pulp (Figure 4).1 Common causes include puncture wounds (e.g., finger stick, splinters) and spread of untreated paronychia.1 The digital pulp is divided into compartments by numerous fibrous septae1,16,40 (Figure 5). A felon presents with severe throbbing pain, tense swelling, and erythema of the finger pad that does not extend proximal to the distal interphalangeal joint because the infection is confined within the noncompliant septal compartments of the digital pulp. Ultrasonography can be used to evaluate for the presence of an abscess.44

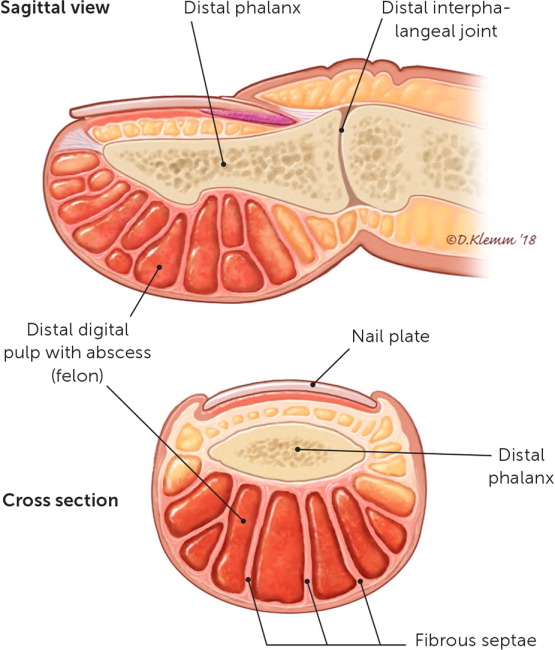
Appropriate management is critical because felons can cause tissue necrosis of the finger pad, osteomyelitis, or pyogenic flexor tenosynovitis if untreated.16 Treatment of an early felon in which no abscess is present should include warm soaks, elevation, and empiric oral antibiotics directed at staphylococcal and streptococcal infections.12,15 Surgical drainage is required if an abscess is present; a high lateral incision should be made for a deep abscess, and a volar longitudinal incision should be made for a superficial abscess.1,16 Methods of performing these incisions, risks of the incisions (anesthetic fingertip, neuroma, and unstable finger pad), and postoperative care recommendations have been described in a previous American Family Physician article.1 Surgical drainage of a felon with abscess is the mainstay of treatment; antibiotics do not provide additional benefit once appropriate drainage has been performed.41
Herpetic Whitlow. Herpetic whitlow is a viral infection of the distal finger caused by inoculation of herpes simplex virus through broken skin. Vesicles of clear fluid on an erythematous base appear within three to four days of exposure to the virus, often coalescing into bullae (Figure 6). Fluid may become turbid or opaque over time. In the absence of other symptoms, this does not signify bacterial superinfection and should not be routinely drained.45 The diagnosis of herpetic whitlow is clinical. In uncertain cases, Tzanck testing, viral culture, or polymerase chain reaction testing of fluid from an unroofed vesicle can confirm the diagnosis. Recurrence occurs in 20% to 50% of cases.17,46 A prodrome of mild burning, itching, and discomfort at a site of prior eruption may occur two to three days before a recurrent outbreak, similar to other herpes simplex virus infections.

Mainstays of therapy for herpetic whitlow include reducing the risk of transmission, pain control, and consideration of antiviral medications. Primary herpetic whitlow is typically self-limited, with complete resolution within 21 days. However, off-label use of oral antivirals should be considered for patients with recurrent lesions or symptoms present for less than 48 hours, or for immunocompromised patients, who may develop disseminated disease requiring intravenous antiviral treatment and critical care.1,18,47 It is important to keep dressings over active lesions dry and to refrain from incision and drainage, which increases the likelihood of bacterial superinfection.17
DEEP HAND INFECTIONS
The anatomy of the hand allows infections to easily spread from the point of inoculation to deep structures, including tendon sheaths, adjacent anatomic compartments, deep fascial planes, bursae, joint spaces, and bones.40 Penetrating trauma often results in severe or rapidly progressing infections within deep structures of the hand. These infections are associated with significant morbidity and dysfunction if not recognized and treated early with surgical management and antibiotics.1,40 Two of the most common deep hand infections are pyogenic flexor tenosynovitis and clenched-fist bite wounds.
Pyogenic Flexor Tenosynovitis. Pyogenic flexor tenosynovitis is a closed-space infection of the flexor tendon sheath. It is most commonly caused by a penetrating injury to the finger. The flexor tendon sheaths in the hand typically span from the neck of the metacarpal to the distal interphalangeal joint, although there are many anatomic variations. Flexor tendon sheaths have a poor vascular supply and are filled with synovial fluid, which is a good medium for bacterial growth.3 Inoculation of bacteria into the synovial fluid causes increased pressure within the sheath, leading to impaired vascular flow, tendon necrosis, and ultimately, tendon rupture.16 Staphylococcus species, including methicillin-resistant S. aureus, and Streptococcus species are the most commonly identified pathogens,12 although approximately one-third of wound cultures show no growth, and gram-negative organisms are present in 10% of cases.2 Hematogenous spread to the tendon sheaths is less common and typically occurs only in immunocompromised patients.40
Pyogenic flexor tenosynovitis is a clinical diagnosis (Figures 7A and 7B) and is classically characterized by the four Kanavel signs: pain with passive extension, tenderness to palpation of the tendon sheath, flexed position, and fusiform swelling1,48 (Table 349–51). Surgical consultation within 72 hours of symptom onset and early treatment with systemic antibiotics improve outcomes.52 Early pyogenic flexor tenosynovitis can be managed nonoperatively, although no specific protocol exists.52 If a nonoperative approach is chosen, surgery should be considered if there is no improvement within 12 to 24 hours.2,52 Minimal incision with catheter irrigation is the mainstay of surgical treatment and results in improved range of motion and fewer infectious complications compared with open surgery53 (Figure 7C). Tobacco use (greater than five-pack-year history) is a newly identified risk factor for more serious infections and delayed wound healing.54

| Kanavel sign | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) |
|---|---|---|---|---|
| Fusiform swelling | 94.3 | 51.3 | 63.5 | 90.9 |
| Flexed position | 91.4 | 51.3 | 62.7 | 86.9 |
| Pain with passive extension | 97.1 | 53.8 | 65.4 | 95.4 |
| Tenderness to palpation of tendon sheath | 91.4 | 69.2 | 72.7 | 90.0 |
Clenched-Fist Bite Wounds. Human bite wounds most often result from direct contact of the fist on incisor teeth, and are known as clenched-fist bite wounds, “fight bite,” or tooth-knuckle injuries. These injuries are more common in younger males and often occur during physical altercations. Clenched-fist bite wounds are usually characterized by a 3- to 5-mm laceration, most often over the metacarpophalangeal joint, followed by the proximal interphalangeal joint.29 Because these injuries do not initially appear severe, many patients do not seek medical attention until infections are advanced.
Because the fist is clenched during injury, teeth may damage deeper structures within the hand, resulting in fracture, joint capsule penetration, or extensor tendon damage29,55 (Figure 8). Older studies have shown that up to 75% of clenched-fist bite wounds result in tendon, bone, joint, or cartilage damage, whereas newer studies suggest that the incidence of joint capsule penetration may be higher, with 100% proximal interphalangeal joint involvement and 95% metacarpophalangeal joint involvement.55,56 Because of the high level of tendon, bone, and joint involvement, it is important that physicians recognize the potential for serious complications when managing clenched-fist bite wounds. Radiography should be obtained to evaluate for fracture, foreign bodies, and early signs of osteomyelitis.19 Neurovascular and musculoskeletal examinations should be performed, and Elson testing should be performed on each digit to evaluate extensor tendon function (https://www.youtube.com/watch?v=wyHSKgAZ1eA).19
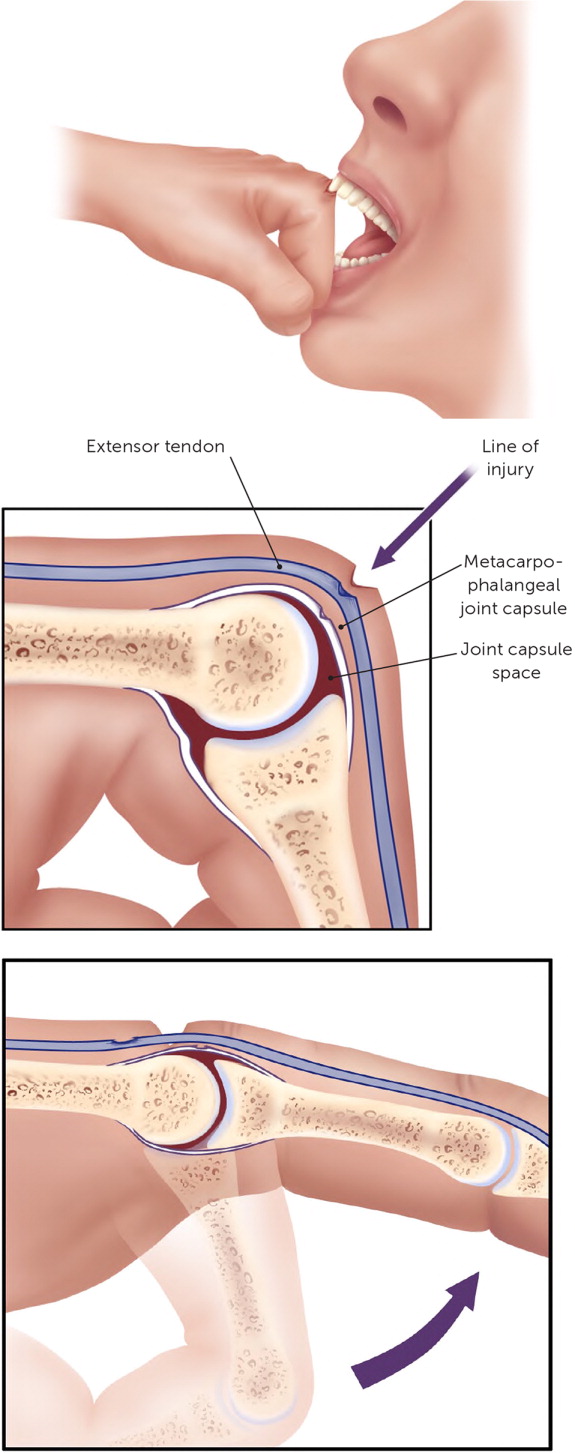
Initial wound management should include hemostasis, copious irrigation, removal of any foreign bodies, and debridement of necrotic tissue.19,29 The wound should be extended to inspect the joint capsule and extensor tendon mechanism.19,55 A tetanus booster and immunoglobulin should be administered, if indicated.19,24,29 Before initiation of empiric antibiotics, tissue should be obtained for Gram staining and aerobic and anaerobic cultures. Tissue cultures are preferred over wound cultures because of their improved accuracy.19 Wounds should be allowed to heal by secondary intent,19,20 and the hand should be splinted in a position of function and elevated.1
Human saliva is bacteria rich; as a result, clenched-fist bite wounds are often polymicrobial.1,12 A single prospective randomized controlled trial supports empiric antibiotic use in all patients.21 This trial compared mechanical wound care alone (n = 15) with wound care plus oral cefaclor (n = 16), or intravenous cefazolin plus penicillin G (n = 17). Patients with joint capsule penetration, tendon injury, or bites older than 24 hours were excluded.20 The trial was terminated because of high rates of infection with wound care alone (47%).20 None of the patients who were treated with antibiotics developed infection.20,21 Oral and intravenous antibiotics were equally effective.20,21
Patients presenting with clenched-fist bite wounds within 24 hours after injury may be treated as outpatients if there are no signs of infection. They should be instructed to follow up within 24 hours after initial treatment.19 Hospitalization should be considered for patients with delayed presentation (more than 24 hours since injury); immunocompromised patients; and those with established infection, systemic manifestations, or evidence of joint capsule penetration.19,22,23,55 Empiric broad-spectrum antibiotics and urgent surgical consultation are indicated for inpatient management.19,22,23,55
Data Sources: A PubMed search was conducted using the key terms acute hand infection, paronychia, felon, herpetic whitlow, flexor tendon synovitis, pyogenic tenosynovitis, human bite injury, clenched fist injury. The search included systematic and clinical reviews, meta-analyses, reviews of clinical trials and other primary sources, and evidence-based guidelines. Also searched were the Cochrane database, the National Institute for Health and Care Excellence guidelines, the Choosing Wisely Campaign, Essential Evidence Plus, Google Scholar, and UpToDate. References from these sources were consulted to clarify the statements made in publications. Search dates: November 2017 to November 2018.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as the official policy or position of the Department of Defense or the U.S. government.
