
Am Fam Physician. 2019;99(12):743
Author disclosure: No relevant financial affiliations.
The United States depends on a robust primary care workforce to achieve the Institute for Healthcare Improvement Triple Aim goal of population health delivered at lower cost and with an improved patient care experience. With nearly 40% of U.S. family physicians older than 55 years, policymakers should support broad-spectrum training models that produce enough primary care physicians to meet state population needs.
In 2018, the World Health Organization reaffirmed the critical role of primary care in driving efficiency, effectiveness, and equity in health systems.1 Access to primary care physicians has been shown to positively influence a range of health outcomes vital to a delivery system increasingly driven by paying for value and the health of populations.2,3 With the decreasing production of general internal medicine physicians because of increases in hospitalists and non–primary care subspecialization, family physicians play a critical role in ensuring a robust primary care workforce.4 However, an aging family physician workforce is a threat to primary care access.
Using data from the 2018 American Medical Association (AMA) Physician Masterfile, we identified primary care physicians (i.e., family physicians, general internists, geriatricians, general pediatricians, and general practitioners) in direct patient care and used their geocoded addresses to map their distribution. We supplemented the total number of doctors of osteopathy in the AMA Physician Masterfile with 2016 Centers for Medicare and Medicaid Services' National Plan and Provider Enumeration System data and Physician Compare data. We identified and excluded hospitalists using 2016 Medicare Provider Utilization and Payment data with methods by Kuo, et al., 2009, and accounted for retired physicians using a method by Petterson, et al., 2016.5,6
We found that, on average, family physicians make up 40% of the primary care physician workforce. We designate “40-40 states” as those with at least 40% of their primary care physician workforce made up of family physicians and at least 40% of their family physicians being older than 55 years (Figure 1).
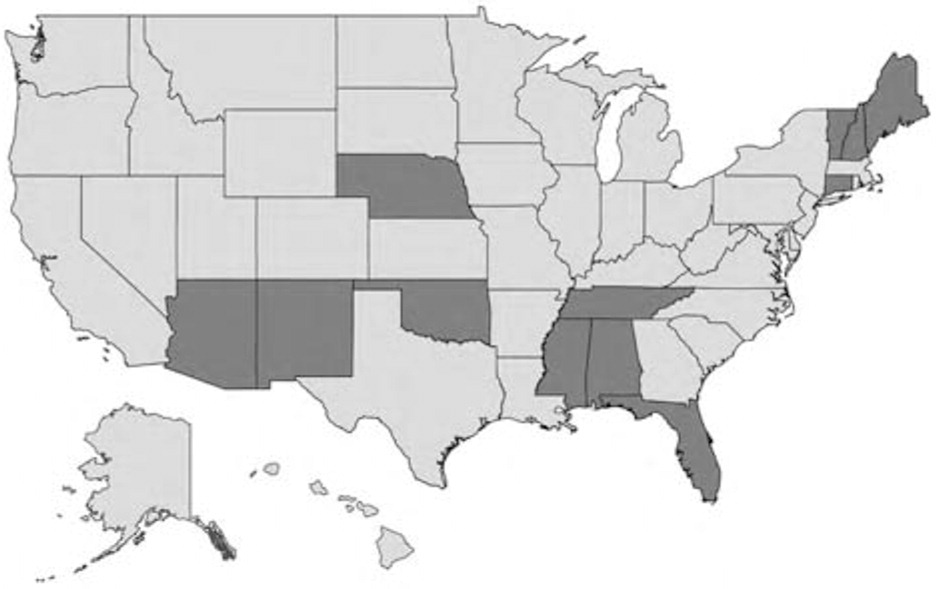
The authors thank David Grolling, MPS, at HealthLandscape for creating the map.
