
Am Fam Physician. 2019;99(12):760-766
Author disclosure: No relevant financial affiliations.
The Bartholin glands, located in the base of the labia minora, have a role in vaginal lubrication. Because of the presence of other glands, removal of a Bartholin gland does not affect lubrication. Ductal blockage of these typically pea-sized structures can result in enlargement of the gland and subsequent development of Bartholin duct cysts or gland abscesses. Two percent of women will develop a cyst or an abscess in their lifetime, and physicians should be familiar with the range of treatment options. Bartholin duct cysts and gland abscesses can be treated in the office. The healing and recurrence rates are similar among fistulization, marsupialization, and silver nitrate and alcohol sclerotherapy. Needle aspiration and incision and drainage, the two simplest procedures, are not recommended because of the relatively increased recurrence rate.
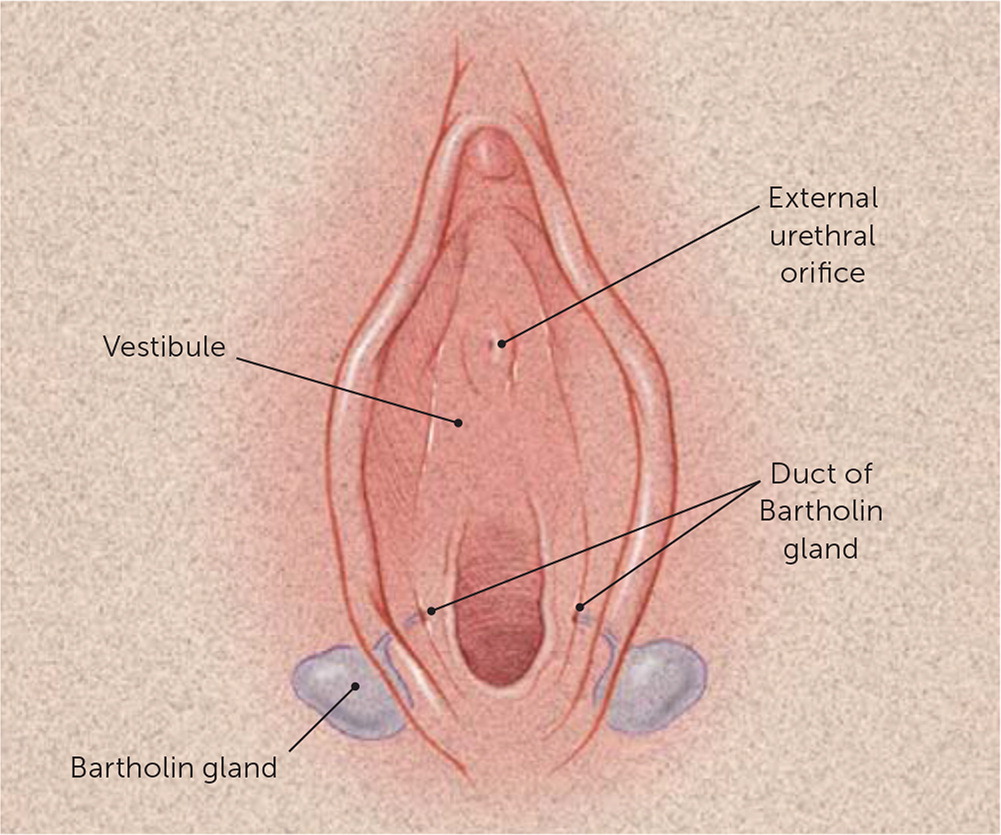
The Bartholin glands, homologues of the male bulbourethral glands, are found bilaterally at 4 and 8 o'clock of the labia minora and drain through ducts 2.0 to 2.5 cm long1,2 (Figure 11). The glands are impalpable and usually pea-sized, rarely exceeding 1 cm.2 The epithelium of the gland is columnar and the duct is squamous, allowing for the possibility of squamous cell carcinoma or adenocarcinoma development.3 During sexual arousal and intercourse, the Bartholin glands secrete vaginal lubricating mucus.2,4 Because of the presence of other glands, including the Skene glands, removal of a Bartholin gland does not affect lubrication.1,2,5
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Bartholin duct cysts or gland abscesses can be effectively treated by several office procedures under local anesthesia. | A | 1, 2, 17, 19, 21, 32 | Based on consistent evidence from patient-oriented studies and supported by usual practice |
| Biopsy with and without excision is recommended in patients 40 years and older to rule out malignancy. | C | 1, 5, 8 | Consensus based on expert opinion and supported by usual practice |
| Jacobi ring and Word catheter placement have acceptable recurrence rates and low complication risks. | B | 19, 23 | Based on consistent evidence from patient-oriented studies |
| Bartholin duct cysts or gland abscesses treated with incision and drainage alone or with needle aspiration have a high rate of recurrence. | B | 1, 2, 5, 8, 17, 18 | Based on patient-oriented evidence with small sample size |
Pathology
Two percent of women develop a Bartholin duct cyst or gland abscess in their lifetime, and physicians should be familiar with the anatomy and range of treatment options.1,3 The ducts leading from the Bartholin glands can become obstructed, resulting in formation of cysts and, when infected, abscesses in the gland.6 Bartholin duct cysts and gland abscesses are more likely to occur in sexually active women as a result of ductal obstruction caused by friction during intercourse.2 Several vulvar lesions mimic Bartholin duct cysts and gland abscesses1–3,7 (Table 11).
| Lesion | Location | Characteristics | |
|---|---|---|---|
| Cystic lesions | |||
| Bartholin duct cyst | Vestibule | Usually unilateral, asymptomatic if small | |
| Bartholin gland abscess | Vestibule | Usually unilateral, painful, erythematous; may be fluctuant | |
| Cyst of the canal of Nuck | Labia majora, mons pubis | Soft, compressible; peritoneum entrapped within round ligament; may mimic inguinal hernia | |
| Epidermal inclusion cyst | Labia majora (usually) | Benign, mobile, nontender; caused by trauma or obstruction of pilosebaceous ducts | |
| Hidradenoma papilliferum | Between labia majora and labia minora | Benign, slow-growing, small nodule (2 mm to 3 cm); arises from apocrine sweat glands | |
| Mucous cyst of the vestibule | Labia minora, vestibule, periclitoral area | Soft, smaller than 2 cm in diameter, smooth surface, superficial location, solitary or multiple, usually asymptomatic | |
| Skene duct cyst | Adjacent to urethral meatus in vestibule | Benign, asymptomatic; if large, may cause urethral obstruction and urinary retention | |
| Solid lesions | |||
| Acrochordon | Labia majora | Benign, fleshy, variable size, polypoid in appearance; usually pedunculated but may be sessile | |
| Angiokeratoma | Multicentric | Rare, benign, vascular, variable size and shape, single or multiple; associated with and aggravated by pregnancy; associated with Fabry disease | |
| Fibroma | Labia majora, perineal body, introitus | Firm, asymptomatic; may develop pedicle; may undergo myxomatous degeneration; potential for malignancy | |
| Leiomyoma | Labia majora | Rare; solitary, firm; arises from smooth muscle | |
| Lipoma | Labia majora, clitoris | Benign, slow-growing, sessile or pedunculated | |
| Neurofibroma | Multicentric | Small, fleshy, multiple, polypoid in appearance; associated with von Recklinghausen disease | |
| Squamous cell carcinoma | Multicentric | Related to benign epithelial disease in older women and to human papillomavirus infection in young women | |
Abscesses are not always preceded by cysts and occur three times more often.1,4,8 Single or polymicrobial opportunistic organisms can cause abscesses. Escherichia coli and Staphylococcus aureus are the most common isolates.6–9 Respiratory organisms such as Streptococcus pneumoniae and Haemophilus influenzae are becoming more common, possibly because of the practice of oral sex.9,10 Sexually transmitted infections have a role in a minority of cases.1,2,6
Bartholin gland involution occurs by 30 years of age, and enlargement in women older than 40 years should raise suspicion for malignancy, particularly if the gland is firm, fixed, or irregularly shaped.1 Therefore, biopsy with or without excision is recommended in patients 40 years and older to rule out malignancy.1,5,8 Although Bartholin gland cancers account for only about 5% of vulvar carcinomas, early recognition is important because of the risk of local invasion and metastasis.1,5,11–14 The two most common types of Bartholin gland carcinomas are squamous cell carcinoma and adenocarcinoma. Human papillomavirus, particularly type 16, is associated with the pathogenesis of squamous cell carcinoma of the Bartholin gland.14–16
Presentation

Office Management
Of the several available office procedures, none has been proven superior in terms of healing time or recurrence rate. Although needle aspiration and incision and drainage are not complicated to perform and have shorter healing time, they confer a considerably higher risk of lesion recurrence.1,2,5,8,17,18
Management is determined by the cyst size, symptoms, patient's age, and history of recurrence.8 Asymptomatic cysts in women younger than 40 years can be left untreated, whereas larger cysts and abscesses may require minor surgical procedures and excisions.1,5,8,19 Antibiotic treatment of Bartholin duct cysts and simple gland abscesses is not necessary in the absence of sexually transmitted infection, urinary tract infection, or cellulitis.2,8,17,20
Fistulization and marsupialization are the two most common procedures for Bartholin duct cysts and gland abscesses.17 Fistulization is the traditional approach for treating symptomatic cysts or abscesses, although it is not appropriate for deep cysts.1,8 The introduced foreign body prevents wound closure, resulting in an epithelialized fistula (i.e., a new outflow tract).17,21,22 Fistulization is achieved by the placement of a Word catheter or Jacobi ring.17,18 The Word catheter is commercially available, whereas the Jacobi ring is assembled by the clinician. Patient and clinician satisfaction with the Jacobi ring is higher compared with the Word catheter.23 The Jacobi ring and the Word catheter result in good resolution, low recurrence, and fewer postprocedure complications; they are also easy and inexpensive.19,23
Although no recent studies have compared all types of fistulization with marsupialization, some have compared Word catheter fistulization with marsupialization, with conflicting results. One study comparing the ease, lesion recurrence rate, and cost of Word catheter fistulization with marsupialization concluded that the Word catheter conferred a higher recurrence rate than marsupialization, although its placement was easier and less expensive.3 The WoMan trial (Word catheter vs. marsupialization), a randomized clinical trial conducted in the Netherlands in women with a Bartholin duct cyst or gland abscess, demonstrated similar recurrence rates with both procedures.21
Sclerotherapy using alcohol or silver nitrate may also be used to treat Bartholin duct cysts and gland abscesses.24,25 Procedure preparation is similar for fistulization or marsupialization (Table 2).1,2,23–26 The benefits, risks, and recurrence rates of these procedures are shown in Table 3.3,18,21,23,24,27–31
| The labia majora is everted, and the mucosal surface overlying the cyst is cleaned with Betadine |
| The subdermal area overlying the cyst/abscess is anesthetized with lidocaine, 1% to 2%, with or without epinephrine |
| The cyst/abscess wall is grasped with small forceps |
| A 3- to 5-mm stab incision is made into the cyst wall with a #11 or #15 blade |
| Procedure | Benefits/advantages | Risks/disadvantages | Risk of recurrence |
|---|---|---|---|
| Alcohol sclerotherapy18,27 | Faster healing than silver nitrate sclerotherapy; short treatment time | Hyperemia; hematoma; tissue necrosis; scarring | 8% to 10% at seven months |
| Incision and drainage alone18,23 | Short treatment time | High recurrence rate | 13% |
| Jacobi ring fistulization23,28 | Easy to perform; two drainage tracts; no premature expulsion; low cost; low short-term recurrence rate; greater patient satisfaction compared with Word catheter fistulization | Requires two incision sites; limited evidence | 0% at six months; 4% at 12 months |
| Marsupialization21,29,30 | Low risk of recurrence | Prolonged healing; secondary infection; prolonged external draining; greater expense | 0% at six months; 10% at 12 months |
| Needle aspiration18,27 | Short treatment time | High recurrence rate | Up to 38% |
| Silver nitrate sclerotherapy24,31 | Less scar tissue than alcohol sclerotherapy; short treatment time | Scarring; vulvar burning; chemical burns; labial edema; hematoma | 3.8% at two months |
| Word catheter fistulization3,18,21 | Easy to perform; low cost; low short-term recurrence rate | Catheter may expel prematurely (23%) if incision is too large; pain at site if balloon is overinflated; contraindicated in patients with latex allergy | 3% at six months; 12% at 12 months |
FISTULIZATION
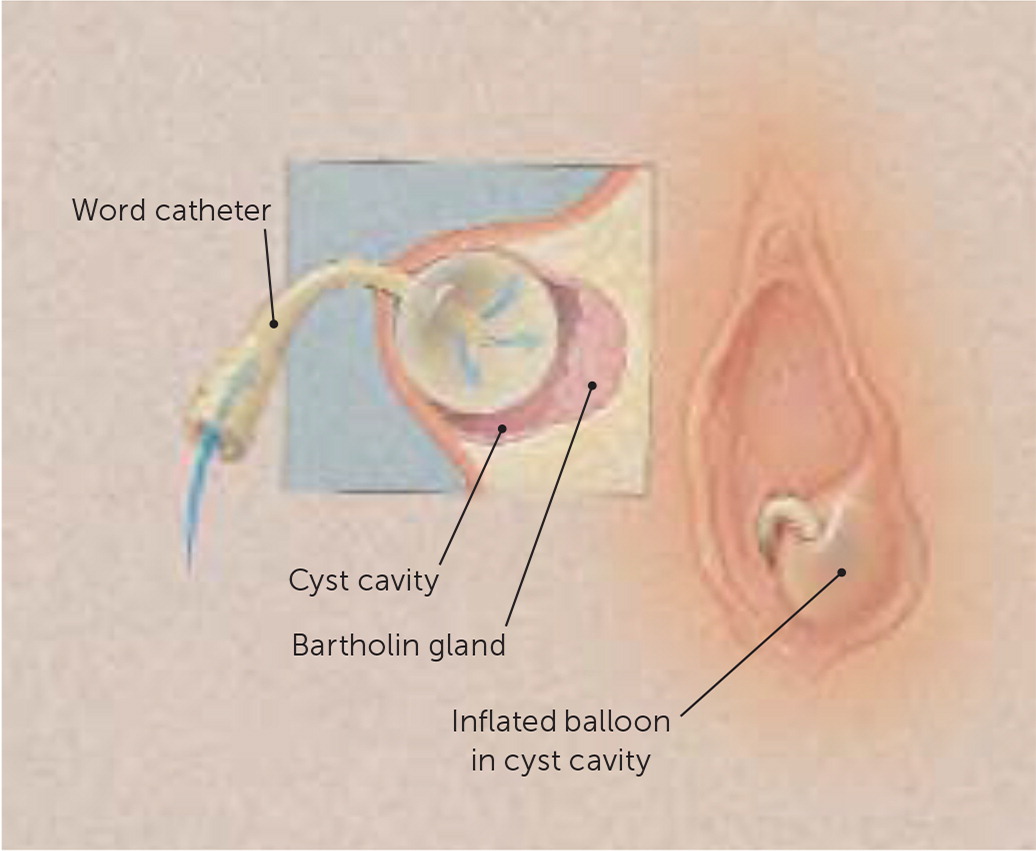
Word Catheter. Once the gland is drained, the Word catheter (Figure 31) is placed into the defect, and the balloon is inflated with 2 to 3 mL of saline (Figure 45; also see https://www.youtube.com/watch?v=zyopxjyExtI). The end of the catheter is placed into the vagina while the cyst continues to drain. It is left in place while the tract completely epithelializes, which takes approximately four to six weeks, or until the balloon spontaneously expels.5 Word catheter placement requires careful attention to incision length because the catheters are often prematurely expelled.1,2,21,22 A suture may be used to close the incision to help keep the catheter in place.22

Ring Catheter. A hemostat is passed into the abscess/cyst cavity and tunneled into the cyst and back to the vaginal mucosa, where a second incision is made. A hemostat is used to grasp one end of the tube/catheter, which has a piece of suture threaded through the lumen. The suture is pulled through the cavity along the same plane, taking care not to pull out the catheter. The two ends of the suture are tied, forming a closed ring (Figure 5). Placement of a ring catheter does not risk premature expulsion and has the benefit of creating two drainage tracts.23
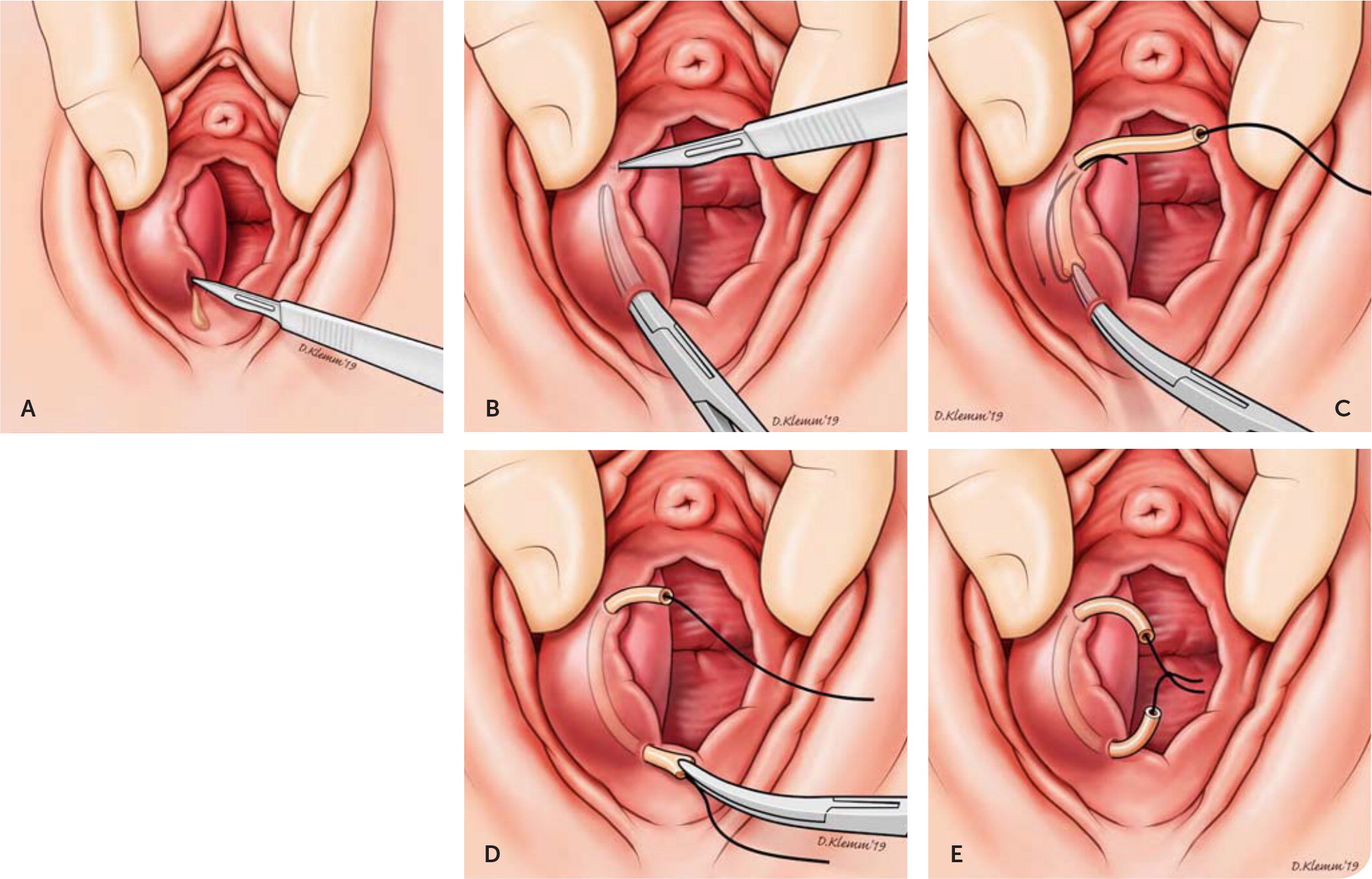
There are no commercially available ring catheters, and two techniques for creating them in the office have been described: (1) a 7-cm length of an 8-French T tube is threaded with a 20-cm length of 2-0 silk suture (Jacobi ring)23; or (2) a 5-cm piece of tubing from a butterfly blood collection set is threaded with absorbable sutures (Vicryl) through the lumen.28
MARSUPIALIZATION
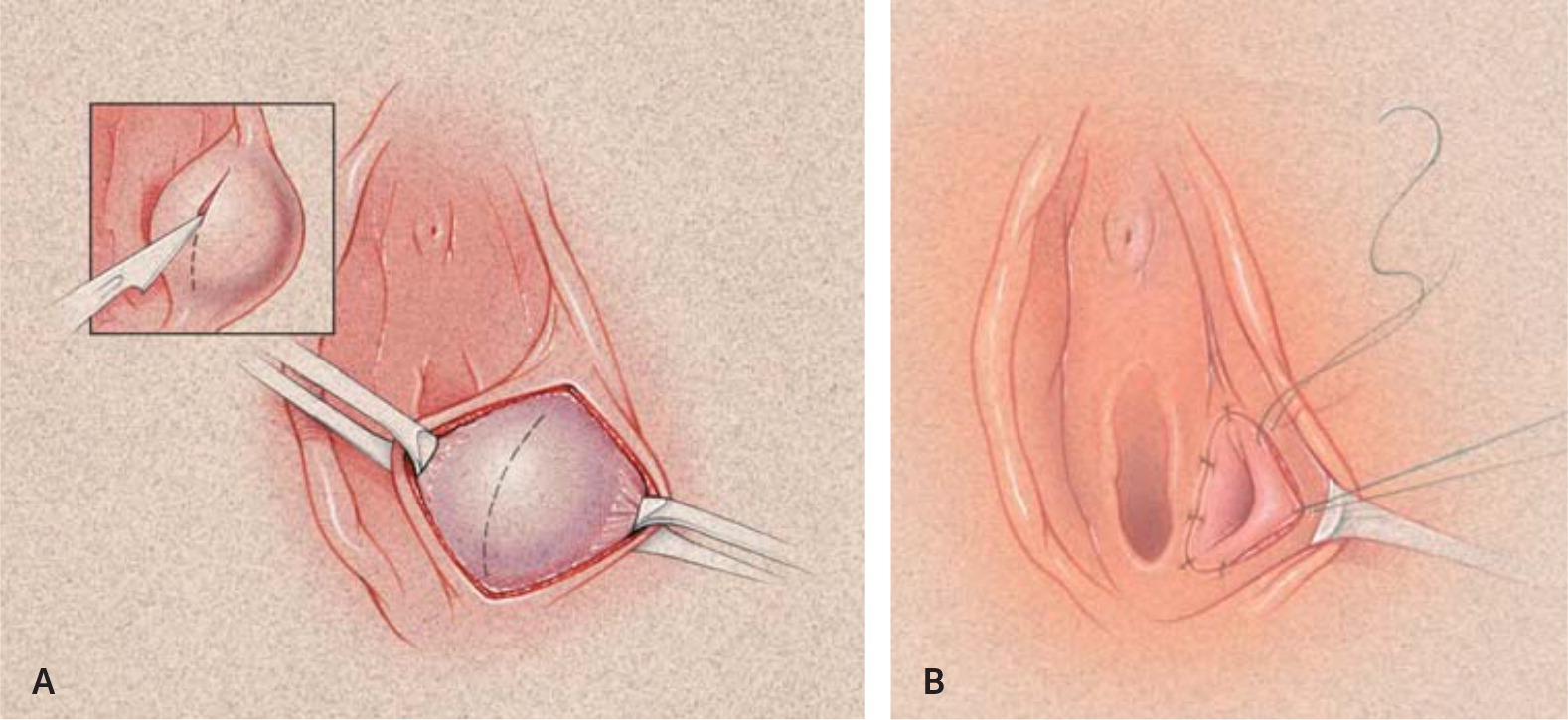
Marsupialization can be used for Bartholin duct cysts and gland abscesses and is the preferred treatment for recurrent lesions.17,31,32 An incision the entire length of the cyst wall is made. Once the cyst is open, it is drained and irrigated with saline. The cyst wall and mucosa are sutured open with interrupted absorbable sutures (2-0 or 3-0 Vicryl) using a small needle (Figure 61; also see https://www.youtube.com/watch?v=mqNmGMv815E). Sitz baths are recommended at least daily beginning on postoperative day 1. The patient is evaluated four weeks after the procedure to assess resolution and adequate healing.17
SCLEROTHERAPY
Sclerotherapy, also known as ablation, is a chemical destruction of the epithelial lining of a Bartholin duct cyst or gland abscess. A randomized controlled trial concluded that the effectiveness and safety of alcohol vs. silver nitrate sclerotherapy are similar despite the minor risks of tissue necrosis and scar formation.24 Both procedures have tolerable complication and recurrence rates. Alcohol sclerotherapy had a healing time of five days vs. 10 days for silver nitrate sclerotherapy.18,24 Preparation of the vaginal mucosa for both procedures is described in Table 2.1,2,23–26
Alcohol Sclerotherapy. An 18- to 20-gauge needle is inserted into the cyst at the point of maximal fluctuation. The contents are aspirated until the cyst walls collapse. A similar volume of 70% alcohol is injected into the cyst and left for five minutes, then aspirated. Healing usually occurs within one week.18
Silver Nitrate Sclerotherapy. A clamp is placed into the cyst/abscess, and the contents are fully drained. A 5-mm diameter silver nitrate stick, trimmed to a length of 5 mm, is inserted into the cavity. One suture is applied to the incision site to allow retention of the stick in the cavity and continued drainage. Using a clamp, the stick is removed with the necrotized tissue after three days. Healing time is approximately two weeks.18,24
PROCEDURES NOT RECOMMENDED
RECURRENCE AND EXCISION
Excision is appropriate after any recurrence. Alternatively, Word catheter fistulization and marsupialization can be used for the first recurrence. The patient should be referred to a gynecologist for excision if she has recurrent lesions, has cysts larger than 5 cm, or is 40 years or older.1,5,17,33
This article updates previous articles on this topic by Omole, et al.,1 and by Hill and Lense.5
Data Sources: A PubMed search was completed using the key terms Bartholin's cyst, gland abscess, and treatment options. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. We also searched the Cochrane database and Essential Evidence Plus. References in these resources were also searched. Search dates: January 2018 to January 2019.
