Am Fam Physician. 2019;100(2):113-114
Author disclosure: No relevant financial affiliations.
A 52-year-old man presented with dysphagia to solids and liquids that had been worsening gradually over the previous two years. He reported a choking sensation with gagging while eating, but drinking water helped wash the food down. He had unintentional weight loss of 100 lb. He also had a dry cough. He had no history of caustic ingestions. Before quitting 10 years earlier, the patient was a 40-pack-year smoker and drank alcohol heavily.
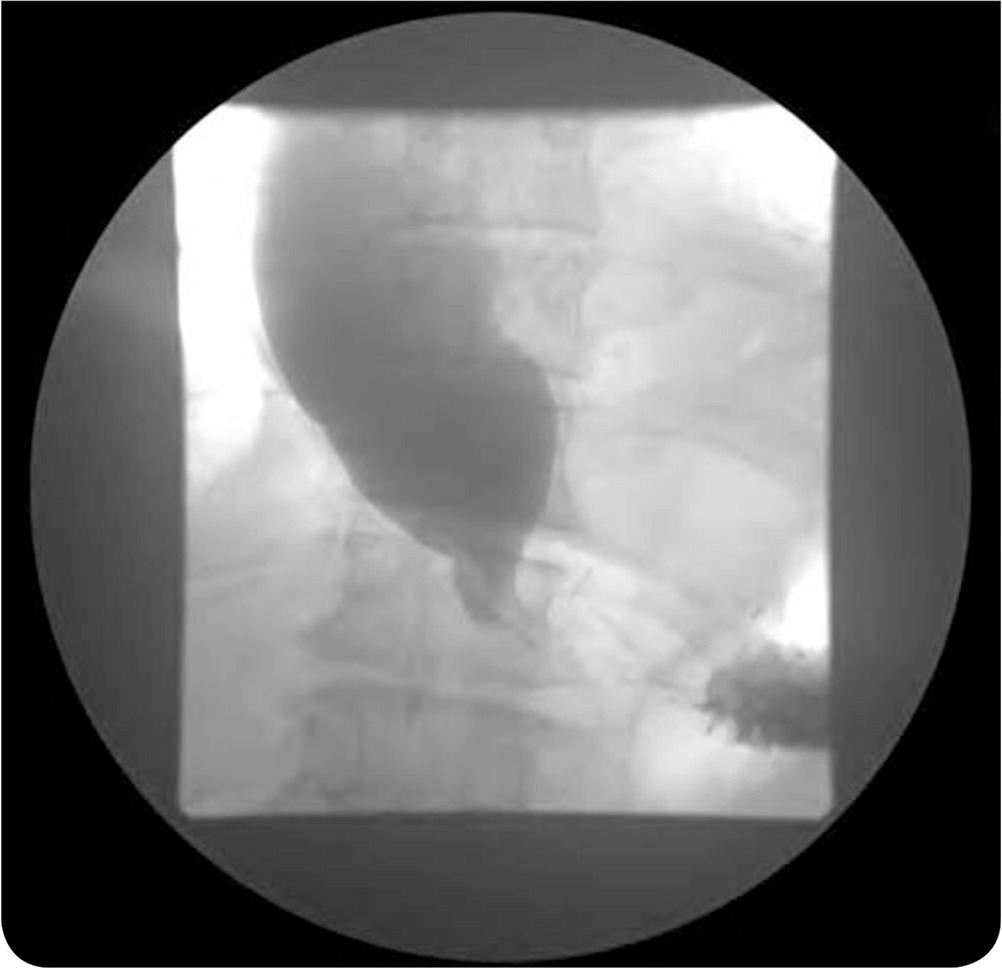
The patient had no improvement with a trial of histamine H2 blockers and proton pump inhibitors. On physical examination, he was obese but had normoactive bowel sounds and no oral lesions. The abdominal examination was normal. A barium swallow test was performed as part of the workup (Figure 1).
Question
Discussion
The answer is A: esophageal achalasia, the inability of the lower esophageal sphincter to relax. People with this condition also have a lack of esophageal peristalsis. Achalasia results from inflammation and degeneration of neurons in the esophageal wall. Although the cause is unknown, there is an association with an inflammatory attack on esophageal neurons in response to a viral infection such as herpes zoster, measles, or herpes simplex virus 1.1,2 There is a possible genetic predisposition to HLA-DQ.2
Achalasia has an annual incidence of 1.6 cases per 100,000 individuals.3 Men and women are affected equally. It has an insidious onset and is usually diagnosed between 25 and 60 years of age.2 Patients present with dysphagia to solids (91%) and liquids (85%), as well as regurgitation of undigested foods or saliva (75% to 91%).4 Patients may present with chest pain, weight loss, and reflux not relieved with acid reducers. Because the food is regurgitated from the esophagus, it is bland, unlike the sour taste that occurs with reflux. Secondary achalasia has been associated with Chagas disease, amyloidosis, sarcoidosis, neurofibromatosis, and eosinophilic esophagitis.5
Esophageal manometry with findings of incomplete relaxation of the lower esophageal sphincter and absent peristalsis of the distal two-thirds of the esophagus is diagnostic for esophageal achalasia.3 Esophagogastroduodenoscopy is needed to exclude malignancy (pseudoachalasia) at late or end-stage achalasia. A barium swallow demonstrates the “bird-beak” appearance caused by the persistently contracted lower esophageal sphincter, as seen in Figure 1. Patients can progress to megaesophagus (diameter greater than 6 cm). Patients with esophageal achalasia have a slightly increased risk of cancer, but endoscopic surveillance is not recommended.4
Esophageal adenocarcinoma commonly arises in the lower half of the esophagus. Barrett esophagus, a condition characterized by metaplastic columnar epithelium that takes over the squamous epithelium in the distal esophagus as a result of gastroesophageal reflux, can lead to the development of adenocarcinoma. Esophageal cancer is more likely to present as a mechanical obstruction rather than dysphagia to solids.
Ingestion of caustic substances can cause injury to the upper gastrointestinal tract, sometimes leading to esophageal stricture. Common alkali-containing agents are bleaches, drain openers, toilet cleaners, and dish detergents. Acid-containing agents include antirust compounds, swimming pool cleaners, and vinegar. Esophagogastroduodenoscopy is important for diagnosis and to detail the extent of injury.
Symptoms of gastroesophageal reflux disease include heartburn, regurgitation, and dysphagia. Patients have daily episodes of symptomatic reflux, including a sour taste, nighttime coughing, and hoarseness. Symptoms usually improve with antireflux measures. It is important to rule out achalasia before surgery in patients with suspected resistant reflux.6
| Condition | Characteristics |
|---|---|
| Esophageal achalasia | Chest pain; weight loss; reflux not relieved with acid reducers because the food is regurgitated from the esophagus; “bird-beak” appearance on a barium swallow test |
| Esophageal cancer | Mechanical obstruction may result in a bird-beak appearance on a barium swallow test, leading to a pseudoachalasia diagnosis (biopsy is required for definitive diagnosis of malignancy in this case); associated with reflux disease |
| Esophageal stricture | Dysphagia and stricture on a barium swallow test; history of caustic ingestion; acute onset |
| Gastroesophageal reflux disease | Heartburn, regurgitation, dysphagia; symptomatic reflux, including a sour taste, nighttime coughing, and hoarseness |