Am Fam Physician. 2019;100(2):89-96
Related editorial: Integrating Medical Acupuncture into Family Medicine Practice.
Related letters: Evidence Lacking That Acupuncture Is More Effective Than Placebo and Acupuncture Not Supported by Strong Scientific Evidence
Patient information: See related handout on acupuncture for pain relief, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Acupuncture has been increasingly used as an integrative or complementary therapy for pain. It is well-tolerated with little risk of serious adverse effects. Traditional acupuncture and nontraditional techniques, such as electroacupuncture and dry needling, often result in reported pain improvement. Multiple factors may contribute to variability in acupuncture's therapeutic effects, including needling technique, number of needles used, duration of needle retention, acupuncture point specificity, number of treatments, and numerous subjective (psychological) factors. Controlled trials have been published on pain syndromes, such as acupuncture for acute and chronic low back pain, knee osteoarthritis, headache, myofascial pain, neck pain, and fibromyalgia. For some conditions, enough data are available for systematic evaluations or meta-analyses. Acupuncture may provide modest benefits in the treatment of chronic low back pain, tension headache and chronic headache, migraine headache prophylaxis, and myofascial pain. Although patients receiving acupuncture for acute low back pain and knee osteoarthritis report less pain, the improvement with true (verum) acupuncture over sham acupuncture is not clinically significant for these conditions. These two conditions illustrate a recurring pattern in acupuncture trials, in which the additional improvement that can be attributed to verum over sham acupuncture, even when statistically significant, is of less clinical significance. This pattern supports the notion that acupuncture treatment has a notable placebo response, or meaning response, that may be responsible for much of its demonstrated benefits. For certain patients, especially those who are unresponsive or intolerant to standard therapies, acupuncture is a reasonable treatment option.
Ever since a National Institutes of Health consensus panel concluded that acupuncture is effective for postoperative dental pain,1 interest in and use of acupuncture in the United States has grown significantly.2,3 Acupuncture has been increasingly used as an integrative or complementary therapy for pain. This article describes the current evidence regarding the use of acupuncture for common pain conditions since the topic was previously covered in American Family Physician.4 Acupuncture resources are listed in Table 1.
| Education and training |
| American Academy of Medical Acupuncture https://www.medicalacupuncture.org/For-Physicians/Education/Ongoing-Courses-Colleges-and-Acupuncture-Schools |
| American Board of Medical Acupuncture http://www.dabma.org/programs.asp |
| Council of Colleges of Acupuncture and Oriental Medicine http://www.ccaom.org/ |
| Demonstration videos |
| Acupuncture https://youtu.be/JnKPNw9K2Ng https://youtu.be/Az9kfSBJeLM https://youtu.be/fqUuPkaHFDI https://youtu.be/SltB04exwo4 |
| Electroacupuncture https://youtu.be/pCZThScE2Ec https://youtu.be/hNWWs7553jE |
| Position papers on dry needling as a type of acupuncture |
| American Academy of Medical Acupuncture https://www.medicalacupuncture.org/Portals/2/PDFs/DryNeedlingPolicyMar2017.pdf |
| American Medical Association https://policysearch.ama-assn.org/policyfinder/detail/dry%20needling?uri=%2FAMADoc%2FHOD-410.949.xml |
| American Physical Therapy Association http://www.apta.org/StateIssues/DryNeedling/ |
| Council of Colleges of Acupuncture and Oriental Medicine http://www.ccaom.org/downloads/CCAOM_Position_Paper__May_2011_Update.pdf |
Traditionally, acupuncture is thought to restore the normal flow of energy (qi) in the body. In the modern era, acupuncture has been shown to have multiple effects on the central and peripheral nervous systems. Functional magnetic resonance imaging has made it possible to study brain responses to acupuncture.5 Release of endogenous opioids, serotonin, and norepinephrine may have downstream effects on nociceptors, inflammatory cytokines, and other physiologic mechanisms that can change pain perception.6 However, the mechanism of acupuncture is likely not completely known.7–9 Acupuncture has been shown to be helpful in some pain syndromes,9,10 although recommendations are generally not strong, and most of the evidence is low or moderate quality.11,12 Quantitative outcome comparisons are included in Table 2.13–18
| Comparison | Outcome |
|---|---|
| Acute low back pain: verum vs. sham acupuncture | MD on a 100-point visual analog scale = −9.38; 95% CI, −17.00 to −1.7613 |
| Acute low back pain (improvement): verum acupuncture vs. nonsteroidal anti-inflammatory medications | RR = 1.11; 95% CI, 1.06 to 1.1613 |
| Chronic nonspecific low back pain: verum vs. sham acupuncture | MD on a 100-point visual analog scale = −17; 95% CI, −33 to −0.214 |
| Peripheral osteoarthritis*: verum acupuncture vs. waiting list controls | Four-point improvement on a 20-point visual analog scale at eight weeks15 |
| Peripheral osteoarthritis*: verum vs. sham acupuncture | SMD = −0.28; 95% CI, −0.045 to −0.11; 0.9-point improvement on a 20-point visual analog scale at eight weeks15 |
| Tension headaches: verum acupuncture vs. usual care | 48% vs. 19% had ≥ 50% reduction in frequency; NNT = 3; RR = 2.5; 95% CI, 2.1 to 3.016 |
| Tension headaches: verum vs. sham acupuncture | 51% vs. 43% had ≥ 50% reduction in frequency; NNT = 13; RR = 1.3; 95% CI, 1.09 to 1.516 |
| Episodic migraine headaches: verum acupuncture vs. drug prophylaxis† | 57% vs. 46% had ≥ 50% reduction in frequency; NNT = 9; RR = 1.24; 95% CI, 1.08 to 1.4417 |
| Episodic migraine headaches: verum vs. sham acupuncture | 50% vs. 41% had ≥ 50% reduction in frequency; NNT = 11; RR = 1.23; 95% CI, 1.11 to 1.3617 |
| Myofascial trigger points associated with low back pain (pain intensity): dry needling vs. other treatments‡ | SMD = −1.1; 95% CI, −1.8 to −0.418 |
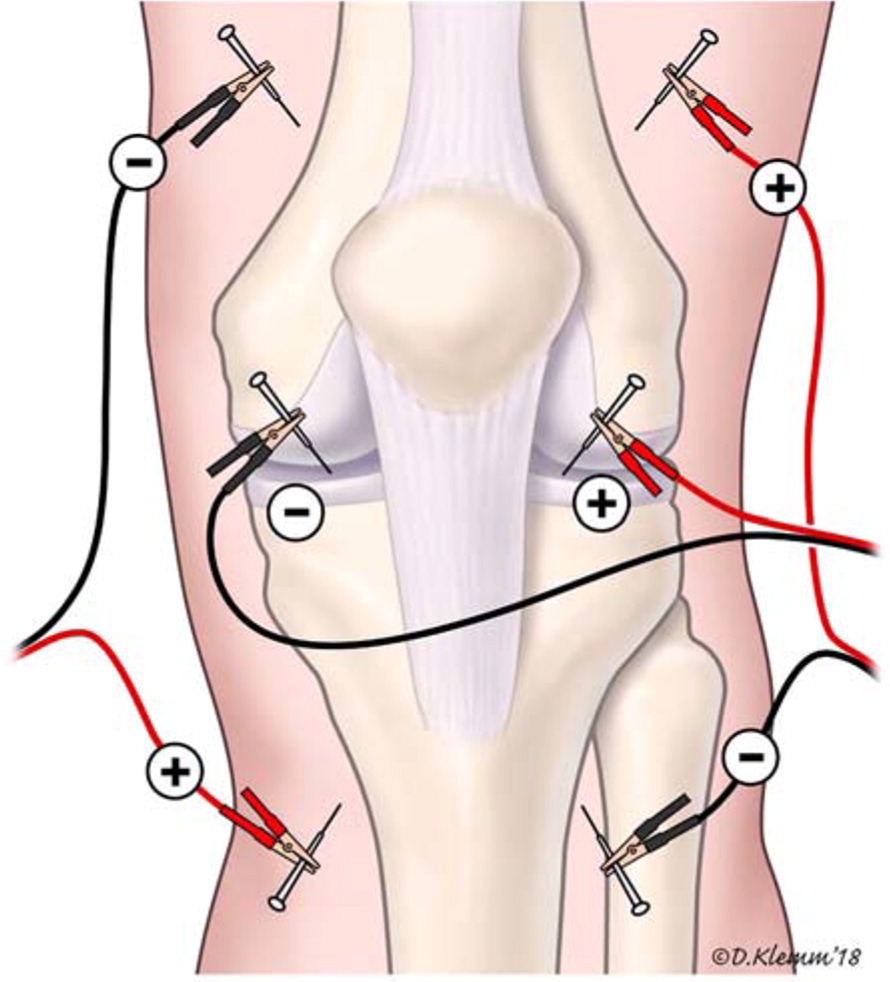
Acupuncturists vary in training, style, experience, and use of related modalities such as traditional pulse diagnosis, tongue diagnosis, herbal therapies, and lifestyle modification. Some use other “microsystem” acupuncture methods, such as ear acupuncture, in addition to or instead of body acupuncture. Physician acupuncturists usually have different training and practice styles than nonphysician acupuncturists and are more likely to use a variety of nontraditional neuroanatomic acupuncture techniques for pain, such as percutaneous electrical nerve stimulation or intramuscular stimulation.19–25
Given the heterogeneity of theory and practice, challenges of conducting randomized controlled trials (RCTs) of acupuncture include effective blinding, adequacy of treatment “dose,” and identification of suitable controls.26,27 The type of needling sensation, method of needle manipulation, use of specific acupoints, and duration of needling potentially effect treatment outcomes,28 although there is little research evidence regarding this. For pain, there is evidence of improved outcomes when more needles are used and when a higher number of treatment sessions are provided.27 RCTs have commonly shown that although sham and verum acupuncture both improve pain, the differences between the two are not large, even when statistically significant.29 Sham treatments can be overly similar to verum treatment, especially when sham treatment includes needle insertion. For example, in 139 studies of painful conditions, when verum acupuncture was compared with no treatment, no needle insertion, and needle insertion, it was shown to significantly reduce pain in 84.3%, 53.3%, and 38% of studies, respectively.30 A recent meta-analysis had similar findings. 29 Importantly, treatment rituals and patient expectations play a role in responses to acupuncture, as they do for other treatments.31
Uses and Effectiveness
Research results are often described in terms of a pain score or a standardized mean difference (SMD). In general, the minimal clinically important difference in a pain score is at least 10%, or 10 points on a 100-point scale. An SMD of 0.2 indicates a small effect, 0.5 a moderate effect, and 0.8 or higher a large effect.
ACUTE AND CHRONIC LOW BACK PAIN
Low back pain is a common reason for people to seek acupuncture treatment. In the past two decades, there have been more than 600 journal articles describing investigations of acupuncture for acute and chronic low back pain.32 In 2005, a Cochrane review concluded that the data at that time did not allow for firm conclusions about the effectiveness of acupuncture for acute back pain. For chronic low back pain, acupuncture was found to be more effective for pain relief and improved function than no treatment or sham treatment in the short term.33
A 2013 systematic review of acupuncture for acute low back pain demonstrated a small but statistically significant improvement in pain intensity with verum vs. sham acupuncture (two studies; mean difference on a 100-point visual analog scale = −9.38 points; 95% CI, −17.00 to −1.76] and a small but statistically significant overall improvement with verum acupuncture vs. anti-inflammatory medications (five studies; risk ratio = 1.11; 95% CI, 1.06 to 1.16).13 However, these differences were of borderline clinical significance. The American College of Physicians recommends including acupuncture as one treatment option for acute and subacute low back pain, based on low-quality evidence.12
In a systematic review and meta-analysis of 25 studies of chronic nonspecific low back pain, verum acupuncture was associated with a statistically and clinically significant reduction in pain compared with sham acupuncture (mean difference on a 100-point visual analog scale = −17 points; 95% CI, −33 to −0.2).14 Using a World Health Organization cost-effectiveness benchmark, acupuncture is cost-effective as a complement to standard care for chronic low back pain ($48,562 per disability-adjusted life-year avoided).34 These findings have led to the inclusion of acupuncture in published guidelines, with evidence for chronic low back pain rated as more robust than that for acute low back pain.12,35 An appraisal of 16 systematic reviews of acute and chronic low back pain reached similar conclusions.36
KNEE OSTEOARTHRITIS
When compared with waiting list controls, acupuncture was associated with clinically and statistically significant improvements in osteoarthritis pain (about four points on a 20-point scale at eight weeks). When compared with sham acupuncture, verum acupuncture was not significantly better clinically (SMD = −0.28; 95% CI, −0.045 to −0.11; 0.9-point improvement on a 20-point scale at eight weeks).15 This suggests that placebo responses are an important mechanism of symptom improvement. Despite this, reviewers pragmatically conclude that acupuncture can be considered as one of the more effective treatments for knee osteoarthritis in the short term.37
HEADACHE PAIN
Acupuncture has been studied in patients with chronic daily idiopathic or tension headaches and for migraine headache prophylaxis. A Cochrane review compared acupuncture with usual care and sham acupuncture for tension headache. When compared with those receiving sham acupuncture, more patients receiving verum acupuncture had at least a 50% reduction in headache frequency (51% vs. 43%; P < .05; number needed to treat [NNT] = 13). This benefit was more notable when verum acupuncture was compared with usual care (48% vs. 19%; P < .05; NNT = 3).16
Another Cochrane review compared verum acupuncture with drug prophylaxis, no treatment, and sham acupuncture for prevention of episodic migraine. More patients receiving verum acupuncture had at least a 50% reduction in headaches compared with sham acupuncture (50% vs. 41%; P < .05; NNT = 11) and drug prophylaxis (57% vs. 46% after three months; P < .05; NNT = 9).17 A separate systematic review reached similar conclusions.40
Acupuncture is as effective as conventional migraine prophylaxis treatments such as valproic acid (Depakene), topiramate (Topamax), metoprolol, and flunarizine (not available in the United States).41 The cost-effectiveness of acupuncture for chronic headache is favorable in the United Kingdom (95% of patients had chronic migraine, $12,080 per QALY gained)42 and Germany (55% of patients had migraine, 39% had tension headache; $13,623 incremental cost per QALY gained compared with routine care alone).43 Overall, the evidence supports acupuncture as a treatment option for migraine and tension headache disorders.44
DRY NEEDLING FOR MYOFASCIAL PAIN
Myofascial pain is characterized by areas of abnormal muscle texture on palpation that is accompanied by tender points and/or taut bands, pain, and reduced range of motion. A characteristic finding is myofascial trigger points. There are many treatment options, such as manipulation, massage, stretching, trigger point injection, and a variety of noninjection needle techniques (dry needling).45
Dry needling is distinguished from trigger point injection (wet needling) because it uses solid acupuncture needles rather than hollow hypodermic needles. Acupuncturists consider dry needling to be a form of nontraditional acupuncture. There are a variety of dry needling approaches, rationales, and styles.46,47 Dry needling is relatively easy to learn and minimally invasive with low risk.45 In many U.S. states, physical therapists are now approved or credentialed to perform dry needling.48
In a systematic review of dry needling for cervicogenic or tension headaches, dry needling resulted in statistically significant improvements in severity and frequency of headaches similar to conventional physiotherapy, as well as clinically significant improvement when added to conventional physiotherapy (45-point improvement on a 100-point visual analog scale).49
Two systematic reviews and meta-analyses of the treatment of trigger points in patients with neck, shoulder, or upper-quarter myofascial pain concluded that dry needling is effective in the short term, with significant improvement in pain intensity immediately to three days after treatment (SMD = −1.9; 95% CI, −3.1 to −0.73).50,51 In the medium term (nine to 28 days after treatment), wet needling and physiotherapy were more effective than dry needling.51
A recent systematic review and meta-analysis including 11 RCTs of the treatment of trigger points associated with low back pain demonstrated that dry needling is more effective than comparison treatments (e.g., verum or sham acupuncture, trigger point injection, superficial or sham dry needling, physical therapy) in reducing pain intensity (SMD = −1.1; 95% CI, −1.8 to −0.4) and functional disability (SMD = −0.76; 95% CI, −1.47 to −0.06). Dry needling in two of the RCTs had additive effects on pain intensity when combined with other treatments (SMD = 0.83; 95% CI, 0.55 to 1.1) but no additive effect on functional disabilty.18 A recent systematic review including 15 RCTs of dry needling to treat trigger points in patients with myofascial pain syndrome and other pain conditions concluded that dry needling is effective in the short-term for pain relief, improved range of motion, and quality of life when compared with no intervention, sham needling, or placebo.52
OTHER PAIN SYNDROMES
A Cochrane review concluded that acupuncture (especially electroacupuncture) can improve pain and stiffness in people with fibromyalgia, based on low to moderate quality evidence.53 It relieves neck pain better than sham acupuncture at completion of treatment and at short-term follow-up.54 Acupuncture has been shown in some studies to improve postoperative pain and to reduce the use of opioid analgesics, although most studies of postoperative pain are small and at risk of bias.55,56
Safety and Adverse Effects
Acupuncture is generally well tolerated with few adverse effects.57 In two large series, mild adverse effects, such as tiredness, local pain, or headache, occurred at least once in about 10% of patients. More significant minor adverse effects, such as severe nausea, fainting, severe or prolonged exacerbation of symptoms, or strong emotional reactions, occurred in 1.3 per 1,000 treatments. No serious events, such as hospital admission, permanent disability, or death occurred. 58,59 Pneumothorax or serious infection has been reported rarely.60
Acupuncture and the Placebo Response
In well-conducted systematic reviews, acupuncture has been shown to provide clinically and statistically significant improvement in patients with certain pain syndromes. However, these studies are often at high risk of bias, especially because of the difficulty in blinding patients to the intervention. When adequately compared, the additional improvement that can be attributed to verum over sham acupuncture is often statistically significant but of questionable clinical significance. This pattern of results makes it likely that much of acupuncture's effectiveness is related to patient expectations, the treatment ritual, the therapeutic interaction with the acupuncturist, and other aspects of placebo responses.
Placebo responses, or meaning responses, are responsible for a significant proportion of the therapeutic effects usually attributed to some medical interventions, especially when outcomes are subjective.31,61,62 An example of objective vs. subjective responses was demonstrated in a small study of patients with asthma, in which albuterol increased forced expiratory volume in one second (FEV1) by 20%, whereas acupuncture and sham acupuncture each resulted in 7% increases in FEV1. However, patient report of improvements was not significantly different for albuterol (50%), acupuncture (45%), or sham acupuncture (46%).63
Placebo responses may be larger for pain conditions than for other target symptom patterns.64 People with a pain syndrome may prefer to try acupuncture instead of usual treatment or may want a trial of acupuncture when other modalities have not been effective or are contraindicated. In a number of common pain syndromes, acupuncture can be recommended to patients as an adjunctive or primary treatment option.
Data Sources: We searched PubMed, the Cochrane database, Essential Evidence Plus, and the National Guideline Clearinghouse. We additionally reviewed information and citations from references 9 and 10. Our focus was on recent systematic reviews and meta-analyses. Search dates: January to March 2018 and February 1, 2019.
The authors thank Michael Wells for his assistance in the literature review and preparation of the manuscript.