Am Fam Physician. 2019;100(5):306-308
Author disclosure: No relevant financial affiliations.
Case Scenario
A 67-year-old woman came to my clinic with uncontrolled hypertension and stage 3 chronic kidney disease. She told me she had not taken her lisinopril because she read on the internet that taking lisinopril causes lung cancer. I searched online and found the population-based cohort study that appeared to be the source of my patient's concerns. What can physicians do when our patients act on findings from the internet? How do physicians address information that tells us that additional studies and more long-term follow-up are needed when our patients have already decided that the alleged risk outweighs the benefits?
Commentary
This case raises important issues related to communicating with patients, including where and how patients get health information, how reliable the information is, and, above all, how well patients understand risk relating to the information. Regarding these issues, physicians need to know the best way to provide patients with convincing, reliable, and accurate information about risk.
WHERE DO PATIENTS GET HEALTH INFORMATION?
Some studies show high percentages of patients getting information from health professionals1; however, national data show otherwise. The annual Health Information National Trends Survey reports that nearly one-half of U.S. adults use the internet as their first source of medical information, whereas only 10% to 15% rely on health care professionals.2 Perhaps not surprisingly, younger adults are more likely than older adults to seek health information on the internet.3 Many individuals, particularly the one-third of U.S. adults with limited literacy,4 are likely to get health information primarily from television, social media, and celebrity webpages,1 and they are less likely to trust information on government websites.5,6
HOW RELIABLE IS THAT INFORMATION?
The internet provides many excellent sources of health information. Physicians regularly use online resources to guide them in the care of patients. However, studies and media reports indicate that members of the public are not always able to distinguish reliable and authoritative health information from unreliable and incorrect information. Individuals tend to believe things that match their own preexisting biases.7 Fake medical news is common, ranging from the well-known false reports of childhood vaccines causing autism or seizures to reports of statins causing cancer.8 Patients often make decisions (e.g., not getting their children vaccinated, not taking their prescribed statins) after reading about or hearing this incorrect information. They may even reject conventional cancer therapies and turn instead to ineffective alternative medicine treatments, resulting in substantial increases in cancer-related death rates.9
HOW WELL DO PATIENTS UNDERSTAND RISK?
Some information that patients find on the internet is factually correct. For instance, patients taking lisinopril do have increased rates of lung cancer, even after adjusting for smoking status. The increased risk, however, is miniscule. Among patients taking the drug for an average of 6.4 years, the rate of lung cancer was 1.6 per 1,000 people compared with 1.2 per 1,000 people not taking the drug.10 That is a difference of 0.4 per 1,000 people, meaning the drug may cause cancer in one out of every 2,500 people who take it for more than six years.
Research shows that most patients do not understand these risk statistics. In one notable study, patients attending an asthma clinic were told that a drug carries a 1% chance of causing a side effect. When asked, only 38% of patients knew that 1% means one out of 100.11
HOW TO EXPLAIN RISK TO PATIENTS
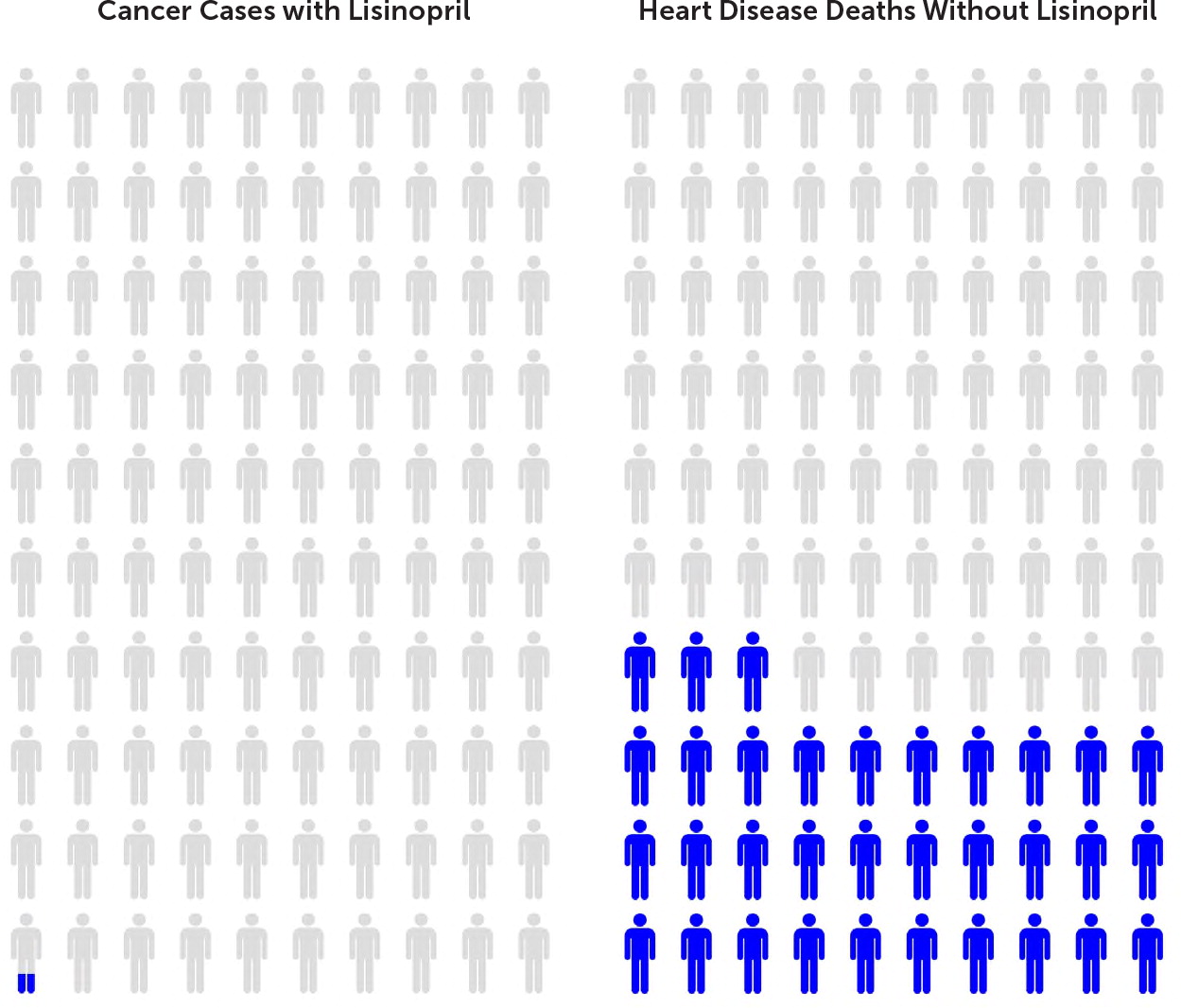
First, commend patients for taking an interest in their medical care. Then, instead of using percentages and other statistics to explain risk, use the research-supported method of showing the patient images (e.g., icon arrays)12,13 that can be easily created using websites (Figure 114), or provide explanations using event rates (i.e., how many out of how many).11,15 For example, ask your patient to imagine a basketball arena containing 10,000 people who have high blood pressure. Treating their blood pressure with lisinopril might cause cancer in four out of those 10,000 people, but it will prevent death from heart disease in more than 3,000 of those 10,000 people.16 The cancer rate associated with patients who take lisinopril is extremely low, whereas the benefit of treating high blood pressure with lisinopril is very high, especially for people with kidney problems, for whom lisinopril is a drug of choice.
Most patients will respond to this kind of explanation, and patient understanding can be confirmed by using the teach-back method—asking patients to explain to you what you have told them.17 Providing understandable information is only the first step in helping patients understand what they need to know as they contemplate the actions they will take in managing their health. But, it is an important first step.
For the patient in this scenario, commend the patient for paying attention to news about the medication she takes. Explain to her that the information she presented is factually correct, but also explain, using event rates and/or an icon array, the risks of her not taking her medication. You can then use the teach-back method to confirm that she understands what you told her and answer any further questions that she might have.
Editor's Note: Dr. Weiss is an Associate Medical Editor for AFP.