
Am Fam Physician. 2019;100(10):639-641
Author disclosure: No relevant financial affiliations.
A 42-year-old man presented after a seizure that lasted approximately four or five minutes. The patient said he had a “weird feeling” before the seizure and a headache afterward. He had not traveled recently and did not have fever, chills, nausea, vomiting, confusion, neck stiffness, head trauma, urinary or bowel incontinence, or other medical problems. He was not taking any medications. The patient immigrated 20 years earlier from Central America. He had a seizure 17 years prior, for which he took an unknown medication.
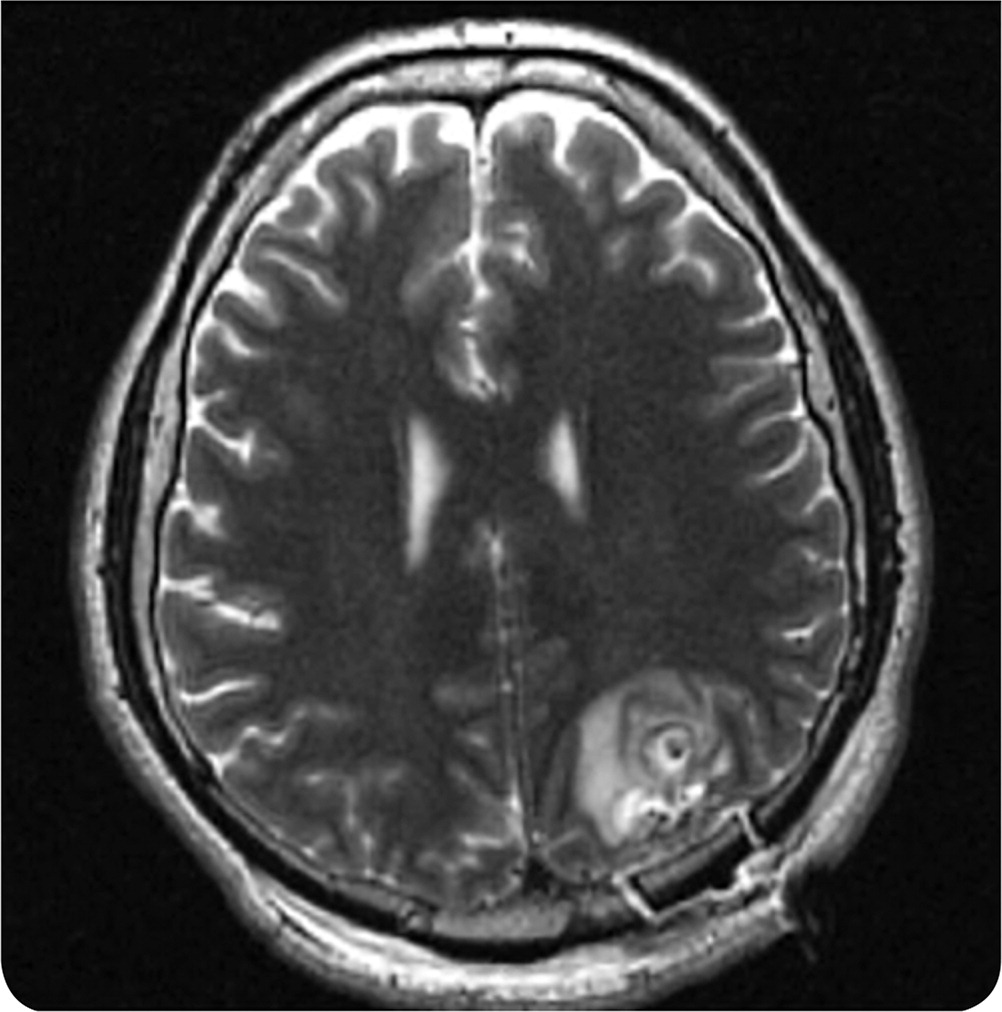
His vital signs were normal. Results of a complete neurologic examination were normal with no focal deficits. Laboratory tests were significant for a lactate level of 36.9 mg per dL (4.1 mmol per L) and mild hyperbilirubinemia. Findings on a complete blood count, basic metabolic panel, and urinalysis were unremarkable. Computed tomography (CT) of the head revealed multiple lesions. A lumbar puncture showed a white blood cell count of 2 per μL (2 × 106 per L), red blood cell count of 198 per μL (198 × 106 per L), protein level between 4 and 8 mg per dL (0.04 and 0.08 g per L), and glucose level between 5 and 8 mg per dL (0.3 and 0.4 mmol per L). Findings on magnetic resonance imaging (MRI) of the brain were abnormal (Figure 1).
Question
Discussion
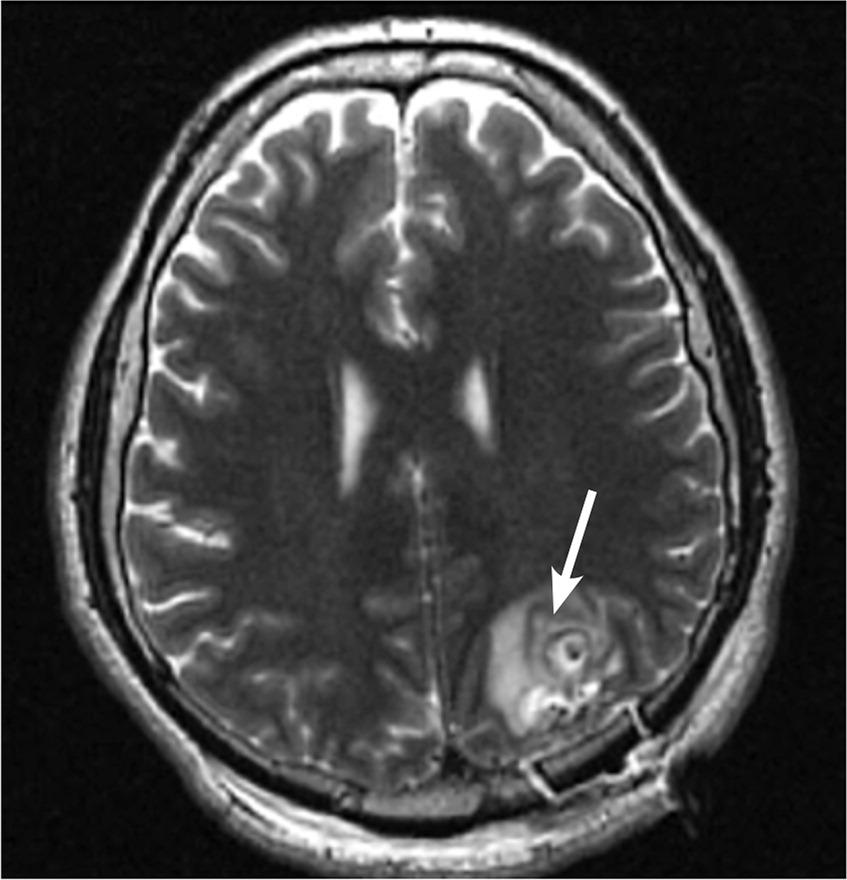
The answer is C: cysticercosis. Cysticercosis is a syndrome caused by infection with Taenia solium larvae, a pork tapeworm that is endemic in Central and South America, Asia, India, and sub-Saharan Africa. Transmission most commonly occurs with consumption of undercooked pork; however, there may be fecal-oral transmission via human carriers in nonendemic areas. Ingested eggs subsequently grow into larvae, leading to cystic lesions.1 These lesions develop in the brain parenchyma and can cause nonspecific neurologic symptoms, including seizures and headaches. Onset of symptoms usually occurs three to five years after exposure, although infection may be asymptomatic or subclinical for decades.2 Intraparenchymal cysticercosis presents as a single ring-enhancing cystic lesion on CT or MRI.
The diagnosis can be confirmed if imaging studies show a contrast-enhancing scolex (the head portion of the tapeworm) inside a cyst (Figure 2) in a patient with exposure risk.3 Serologic and cerebrospinal fluid testing may be performed if the history and imaging are inadequate for conclusive diagnosis.
Treatment is not indicated in all patients and may be harmful by triggering a severe host immune response. When indicated, cysticercosis is treated with albendazole (Albenza). Praziquantel (Biltricide) can be added in cases of high disease burden and should be accompanied by dexamethasone suppressive therapy (beginning one day before initiating praziquantel) and prolonged antiepileptic therapy.2,3 The recurrence rate after initial treatment is unknown, but several cases of recurrence have been reported.
Brain tumors can be primary or metastatic. Typically, primary tumors are solitary, and metastases are multiple. Metastases are unlikely with a single brain lesion and no extracranial primary lesion. Patients with metastatic cancer often have systemic symptoms, such as weight loss.
Coccidioidomycosis is caused by infection with the dimorphic fungi of the genus Coccidioides (C. immitis and C. posadasii), which are endemic in the Desert Southwest region of the United States and in Central and South America. Transmission occurs through inhalation of spores. Meningitis is the most serious complication of coccidioidomycosis. However, cocci infections usually present as pulmonary symptoms and systemic symptoms, such as fever, chills, night sweats, and weight loss. Chest radiography shows pulmonary granulomas, and neuroimaging may reveal a single granuloma or multiple granulomas with ischemia and/or vasculitis.4
Toxoplasmosis is caused by Toxoplasma gondii infection. Like cysticercosis, it can be contracted by eating undercooked meat. Toxoplasmosis causes small intraparenchymal ring-enhancing lesions on CT5 but without the scolex typical of neurocysticercosis. It is usually asymptomatic in immunocompetent people.
Tuberculomas are foci of Mycobacterium tuberculosis bacteria that can develop anywhere in the body, including the brain. CT may reveal a mass with centralized calcification, whereas MRI may show a mass with an enhancing rim.6 Tuberculosis usually presents as pulmonary symptoms (cough, hemoptysis) and systemic symptoms (e.g., fever, chills, night sweats, weight loss).
| Condition | Characteristics | Imaging findings |
|---|---|---|
| Brain metastases | Metastases from other primary tumors, especially carcinomas, including melanoma and lung, breast, kidney, and colorectal cancers | Multiple solid, ring-enhancing lesions |
| Coccidioidomycosis | Caused by Coccidioides immitis or C. posadasii infection; endemic in the Desert Southwest region of the United States and in Central and South America; transmission occurs through inhalation of spores; primarily pulmonary and systemic symptoms | Pulmonary granulomas on chest radiography; neuroimaging may reveal a single granuloma or multiple granulomas with ischemia and/or vasculitis |
| Cysticercosis | Syndrome caused by infection with Taenia solium larvae; endemic in Central and South America, Asia, India, and sub-Saharan Africa; transmission usually through undercooked pork, but fecal-oral transmission possible in nonendemic areas; nonspecific neurologic symptoms, including seizures or headaches | Single ring-enhancing lesions on head CT or MRI; pathognomonic intralesional contrast-enhancing scolex |
| Toxoplasmosis | Caused by Toxoplasma gondii infection; transmission through undercooked meat or cat feces; usually asymptomatic in immunocompetent people | Intraparenchymal ring-enhancing lesions on CT |
| Tuberculosis | Tuberculomas (foci of Mycobacterium tuberculosis bacteria that can develop anywhere in the body, including the brain); pulmonary and systemic symptoms | Hilar adenopathy and pulmonary infiltrates on chest radiography; single small, calcified lesion on CT or ring-enhancing lesions on MRI |
