Am Fam Physician. 2020;101(2):84-88
Author disclosure: No relevant financial affiliations.
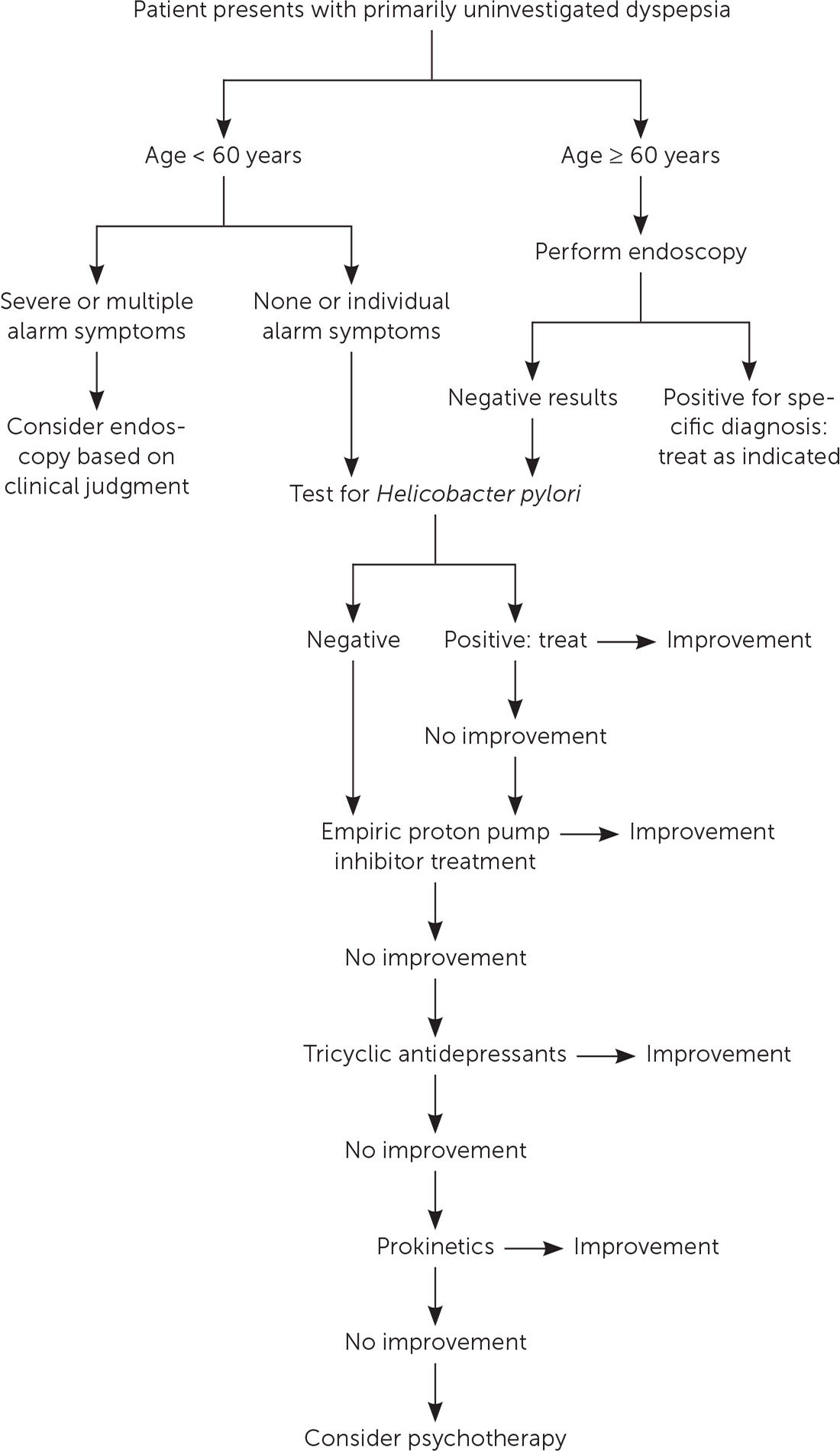
Functional dyspepsia is defined as at least one month of epigastric discomfort without evidence of organic disease found during an upper endoscopy, and it accounts for 70% of dyspepsia. Symptoms of functional dyspepsia include postprandial fullness, early satiety, and epigastric pain or burning. Functional dyspepsia is a diagnosis of exclusion; therefore, evaluation for a more serious disease such as an upper gastrointestinal malignancy is warranted. Individual alarm symptoms do not correlate with malignancy for patients younger than 60 years, and endoscopy is not necessarily warranted but should be considered for patients with severe or multiple alarm symptoms. For patients younger than 60 years, a test and treat strategy for Helicobacter pylori is recommended before acid suppression therapy. For patients 60 years or older, upper endoscopy should be performed. All patients should be advised to limit foods associated with increased symptoms of dyspepsia; a diet low in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) is suggested. Eight weeks of acid suppression therapy is recommended for patients who test negative for H. pylori, or who continue to have symptoms after H. pylori eradication. If acid suppression does not alleviate symptoms, patients should be treated with tricyclic antidepressants followed by prokinetics and psychological therapy. The routine use of complementary and alternative medicine therapies has not shown evidence of effectiveness and is not recommended.
Dyspepsia affects up to 30% of the general population in the United States, Canada, and the United Kingdom, with 70% of these patients having functional dyspepsia.1 The American College of Gastroenterology (ACG) and the Canadian Association of Gastroenterology (CAG) broadly define functional dyspepsia as at least one month of epigastric discomfort without evidence of organic disease on endoscopy.2 The more detailed Rome IV diagnostic criteria define functional dyspepsia as one to three days per week of symptoms of postprandial fullness, early satiety, epigastric pain, or epigastric burning without evidence of structural disease (Table 1).3 A calculator using the Rome IV criteria is available to aid with diagnosis at https://www.mdcalc.com/rome-iv-diagnostic-criteria-dyspepsia. Historically, Rome criteria have been used primarily for research, but the update to Rome IV attempts to increase its usefulness in clinical practice.4 The superseded Rome III criteria specifically excluded patients with heartburn and gastroesophageal reflux disease, but the definition of functional dyspepsia has now been broadened to include these patients. A cross-sectional study using the Rome IV criteria estimated the prevalence of functional dyspepsia to be 12% in the United States and was the most common cause of dyspepsia.1
WHAT'S NEW ON THIS TOPIC
Functional Dyspepsia
A cross-sectional study using the Rome IV diagnostic criteria for functional dyspepsia estimated the prevalence to be 12% in the United States, making it the most common cause of dyspepsia.
A systematic review of 15 observational studies and one randomized controlled trial found that foods high in fat, wheat, FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), and naturally occurring food chemicals, such as caffeine, were associated with symptoms of functional dyspepsia.
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Endoscopy should be performed for all patients 60 years and older with at least one month of dyspepsia symptoms.2 | C | Expert opinion based on the low prevalence of malignancy in younger patients and economic modeling |
| For patients younger than 60 years with a single, nonsevere alarm feature, endoscopy should not be the first diagnostic step.2,13 | B | Systematic review of seven retrospective cohort studies showing a positive predictive value of less than 1% for malignancy |
| For patients younger than 60 years, a Helicobacter pylori test and treat strategy before acid suppression is effective.2,14,17,18 | A | Consistent evidence from high-quality meta-analysis of 25 RCTs and one high-quality RCT |
| Proton pump inhibitor therapy is more effective than placebo for symptom relief.2,20 | A | Meta-analysis of seven high-quality RCTs |
| Presence of at least one of the following: |
| Postprandial fullness (3 days per week) |
| Early satiety (3 days per week) |
| Epigastric pain (1 day per week) |
| Epigastric burning (1 day per week) |
| and |
| No evidence of structural disease |
Pathophysiology
The causes of functional dyspepsia are multifactorial.5 Helicobacter pylori infection and acid secretion may play a role because H. pylori eradication and acid suppression improve symptoms of dyspepsia.2 Abnormal gastric or duodenal motility and impaired gastric myoelectrical activity are present in 70% to 80% of patients with functional dyspepsia accompanied by postprandial pain or discomfort.6 Other studies implicate immune activation, with increased T cells, eosinophilia, and mast cells found in the bowel wall of patients with functional dyspepsia and irritable bowel syndrome.7,8 There is also an association with mental health disorders, because rates of anxiety and depression are higher for patients with functional dyspepsia than for patients with dyspepsia from an organic cause or for healthy individuals.9 There is overlap in functional dyspepsia with gastroesophageal reflux disease and irritable bowel syndrome, with some studies estimating that 50% of patients with functional dyspepsia have gastroesophageal reflux disease and 35% have irritable bowel syndrome.10
Diagnostic Approach
Functional dyspepsia has been categorized as a diagnosis of exclusion in the past. The more specific Rome IV criteria allow for a definitive diagnosis of functional dyspepsia to be made for patients who have normal upper endoscopy findings.3 For patients who have not had an endoscopy, the diagnosis is only likely based on the exclusion of other causes. Family physicians should complete a history and physical examination to determine other possible etiologies of the dyspeptic symptoms (Table 22,11,12). Medication history should be taken to assess for any drugs that are associated with dyspepsia (Table 311). Functional dyspepsia is the most common cause of dyspepsia, and many organic dyspepsia etiologies are rare; therefore, history is not useful in differentiating between functional and organic dyspepsia, and management does not depend on this differentiation.1,11,12 Figure 1 is an algorithm for the evaluation and management of dyspepsia.2,11
| Clinical indications | Possible etiologies |
|---|---|
| Age 60 or older; severe or multiple alarm features (e.g., dysphagia, weight loss, anemia); epigastric mass; enlarged supraclavicular lymph node | Malignancy |
| Pain radiating to the back, right upper quadrant pain, vomiting, jaundice | Biliary or pancreatic processes |
| Vomiting, severe nausea | Gastroparesis |
| Acarbose (Precose) |
| Antibiotics |
| Bisphosphonates |
| Corticosteroids |
| Herbs (e.g., chaste tree berry, feverfew, garlic, ginkgo, saw palmetto, white willow bark) |
| Iron |
| Metformin |
| Miglitol (Glyset) |
| Nonsteroidal anti-inflammatory drugs, including cyclooxygenase-2 inhibitors |
| Opiates |
| Orlistat (Xenical) |
| Potassium chloride |
| Theophylline |
The 2017 ACG/CAG guidelines recommend upper endoscopy be performed for all patients 60 years or older who present with at least one month of dyspepsia symptoms. The age threshold may be lowered in patients with a higher risk of upper gastrointestinal malignancy (e.g., patients of southeast Asian descent). Endoscopy should not be performed routinely for patients younger than 60 years. This recommendation is based on the low prevalence of malignancy in younger patients and cost-effective economic modeling.2 The presence of one alarm feature such as weight loss, anemia, or dysphagia should not be used to recommend endoscopy because each has a positive predictive value of less than 1% for malignancy.2,13 The predictive values of severe (e.g., profound weight loss, quickly progressing dysphagia) or multiple alarm symptoms have not been studied; therefore, the judgment of the physician should determine the need for endoscopy.2 A test and treat strategy for H. pylori for all patients younger than 60 years is a safe and effective option before treatment with acid suppression.2,14 Endoscopy does not reassure patients with functional dyspepsia or improve quality of life assessments.15
Treatment
DIETARY MODIFICATION
A low-risk intervention for patients is to encourage dietary modifications to limit foods associated with functional dyspepsia. A systematic review of 15 observational studies and one randomized controlled trial (RCT) found that foods high in fat, wheat, FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols), and naturally occurring food chemicals such as caffeine were associated with symptoms of functional dyspepsia.16 A list of FODMAP common foods can be found at https://www.ibsdiets.org/wp-content/uploads/2016/03/IBSDiets-FODMAP-chart.pdf. The association of alcohol consumption with the symptoms of functional dyspepsia is not as clear and may depend on the type of alcohol.16
H. PYLORI ERADICATION
H. pylori test and treat strategies, when compared with endoscopy, are safe, effective, and cost-effective for managing patients with dyspepsia.2 Noninvasive testing for H. pylori includes a urea breath test and an H. pylori stool antigen test. In a meta-analysis of 23 studies, H. pylori eradication therapy demonstrated no difference in symptoms of functional dyspepsia at six months but did show improvement at one year.17 An RCT comparing H. pylori eradication with placebo found a 50% reduction in functional dyspepsia symptoms (number needed to treat [NNT] = 8).18 Another guideline strongly recommended that H. pylori infection was the cause of dyspepsia in a subset of patients and recommended eradication.19 Patients who test negative for H. pylori or continue to have symptoms after treatment should be started on a proton pump inhibitor (PPI).2
ACID SUPPRESSION
The mainstay of acid suppression includes two classes of medications: PPIs and histamine H2 receptor antagonists. A meta-analysis found standard daily dosages of PPIs taken over two to eight weeks to be superior to placebo for the reduction of functional dyspepsia symptoms (NNT = 14).20 The treatment benefit presented only in patients with burning epigastric pain and reflux-like pain and not for patients with dysmotility-related issues.21 Observational studies have found that long-term use of PPIs, typically longer than 12 months, is associated with chronic kidney disease, bone fracture, Clostridioides difficile (formerly Clostridium difficile) infection, and community-acquired pneumonia. The benefits likely outweigh the harms with an estimated number needed to harm of greater than 1,000.2,22 PPIs should be prescribed for eight weeks with standard per-day dosing. There is not an advantage to doubling the dosing.2
H2 antagonists are also an option for functional dyspepsia treatment. Twelve RCTs compared H2 antagonists with placebo and showed a relative risk reduction of 23% in symptoms of dyspepsia (NNT = 7).12 In a systematic review of seven heterogeneous RCTs comparing H2 antagonists with PPIs, there was no statistically significant difference in the two approaches in providing symptom relief. Four of the seven studies found PPIs to be superior, leading the ACG to recommend PPIs as first-line treatment.2 Antacids and sucralfate (Carafate) are not effective for the treatment of functional dyspepsia.23 Although bismuth has shown a small benefit, it is not recommended because of the risk of long-term toxicity.23
PSYCHOTROPIC MEDICATIONS
A systematic review of psychotropic medications compared with placebo for the treatment of functional dyspepsia included three trials of tricyclic antidepressants (TCAs) and found a reduction in dyspepsia symptoms (NNT = 6; 95% CI, 4 to 16).24 The dosages for these trials were 25 mg of amitriptyline per day and 50 mg of imipramine per day. Two trials compared selective serotonin reuptake inhibitors with placebo and found no significant effect for dyspepsia symptoms. Given these findings, guidelines recommend the use of TCAs, before using prokinetics, for functional dyspepsia that is not improving with treatment for H. pylori or PPI use.2 A small placebo-controlled study found buspirone (Buspar) reduced fullness and bloating.25
PROKINETICS
For patients who have functional dyspepsia with postprandial distress syndrome, which is characterized by meal-related symptoms, prokinetic agents can reduce symptoms. A review of 29 trials comparing prokinetics (predominantly cisapride) to placebo found a significant reduction in global symptoms of functional dyspepsia (NNT = 7).26 Domperidone is not available in the United States, and cisapride was withdrawn from the market because of cardiac adverse effects. Neither of the prokinetic agents available in the United States, metoclopramide (Reglan) or prucolamide (Motegrity), have been evaluated for the treatment of functional dyspepsia. Guidelines from the ACG recommend metoclopramide as a treatment option.2 [revised]
NONPHARMACOLOGIC THERAPY
A review of 12 RCTs of patients with functional dyspepsia found a statistically significant benefit of psychological therapy (i.e., cognitive behavior therapy and other forms of psychotherapy) over the control group.2 Psychotherapy should not be used as a first-line treatment for functional dyspepsia because of the low quality of the data, the high risk of bias attributed to the lack of blinded psychological interventions, and subjective symptom scoring. It is reasonable to consider psychological therapy if drug therapy has been ineffective.
COMPLEMENTARY AND ALTERNATIVE MEDICINE
The ACG does not recommend the routine use of complementary and alternative medicines for the treatment of functional dyspepsia but states that these alternatives can be considered for patients who are motivated. Iberogast, an herbal preparation containing extracts of bitter candytuft, matricaria flower, peppermint leaves, caraway, licorice root, and lemon balm, was statistically superior, but only marginally clinically superior, to placebo in one randomized trial.27 A Cochrane review of seven low-quality studies of patients with functional dyspepsia evaluated acupuncture compared with medications or sham acupuncture and found no clear evidence of effectiveness.28 A systematic review of 27 RCTs evaluated Si-Mo-Tang liquid, a Chinese herbal medicine, and found some symptomatic improvement but the studies were low quality with significant heterogeneity.29
This article updates previous articles on this topic by Loyd and McClellan,11 and Dickerson and King.30
Data Sources: A PubMed search was completed using the key words functional dyspepsia, nonulcer dyspepsia treatment for H. pylori, and treatment for functional dyspepsia with prokinetics, PPI, and complementary and alternative medicine. Additional searches included the Cochrane database of systematic reviews, the Cochrane database of RCTs, Essential Evidence, Agency for Healthcare Research and Quality, Trip database, and the U.S. Preventive Services Task Force. The ACG functional dyspepsia guidelines were also reviewed. Search dates: February to April 2019, and October 2019.