Am Fam Physician. 2020;101(8):463-470
Patient information: See related handout on burn injuries, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Most patients with burn injuries are treated as outpatients. Two key determinants of the need for referral to a burn center are burn depth and percentage of total body surface area involved. All burn injuries are considered trauma, prompting immediate evaluation for concomitant injuries. Initial treatment is directed at stopping the burn process. Superficial (first-degree) burns involve only the epidermal layer and require simple first-aid techniques with over-the-counter pain relievers. Partial-thickness (second-degree) burns are subdivided into two categories: superficial and deep. Superficial partial-thickness burns extend into the dermis, may take up to three weeks to heal, and require advanced dressings to protect the wound and promote a moist environment. Deep partial-thickness burns require immediate referral to a burn surgeon for possible early tangential excision. Full-thickness (third-degree) burns involve the entire dermal layer, and patients with these burns should automatically be referred to a burn center. Prophylactic antibiotics are not indicated for outpatient management and may increase bacterial resistance. People with diabetes mellitus are at increased risk of complications and infection, and early referral to a burn center should be considered. Pruritus, hypertrophic scarring, and permanent hyperpigmentation are long-term complications of partial-thickness burns. Burn injuries are more likely to occur in children and older people. Patient education during primary care visits may be an effective prevention strategy.
Approximately 500,000 patients seek medical care for burns every year in the United States, and roughly 92% are treated as outpatients.1,2 Even small-appearing burns can cause significant morbidity because of pain, secondary infection, and scarring if not treated properly.1 The mechanism of burn injury can be categorized as thermal (caused by contact with flames, steam, or hot surfaces), electrical, chemical, and radiation.1,3 Thermal burns are the most common type among all ages.2,3
Anatomy and Skin Function
Familiarity with skin anatomy is necessary to understand burn injury classification. Skin is the largest organ of the body and functions include thermoregulatory control, prevention of fluid loss, vitamin D synthesis, sensory contact with the environment, and a physical barrier against injury.4 The outermost skin layer is the avascular epidermis, which is 10 to 100 cells thick.5 Under the epidermis and basal membrane is the dermis, which contains sebaceous and sweat glands, hair follicles, blood vessels, nerves, and stem cells.1,5 The dermis lies on the subcutis, which consists of thick adipose tissue.5
Burn Classification
The American Burn Association classifies burns by depth: superficial (first-degree), partial-thickness (second-degree), and full-thickness (third-degree). The “thickness” and “degree” naming conventions are commonly used and must be understood to effectively communicate with burn center personnel and surgeons.6
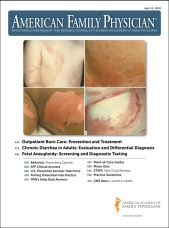
Superficial burns (Figure 17) are localized to the epidermal layer and are painful, erythematous, dry, and blanching. These burns do not blister and take three to six days to heal.1,3,5,6 With partial-thickness burns, the epidermis is destroyed and the dermal layer is injured.1,3,5 Partial-thickness burns are subclassified as superficial or deep (Figure 28). Superficial partial-thickness burns are exudative, blanch with pressure, may blister, and are generally painful.1,3 Most will heal within three weeks.1,6 Deep partial-thickness burns involve the reticular dermis, are drier, and do not blanch.3 These usually take more than three weeks to heal and lead to loss of the dermal layer and scarring.3,6 Deep partial-thickness burns should receive immediate evaluation by a burn surgeon for consideration of early operative management with tangential excision and skin grafting.3,6 Full-thickness burns (Figure 37) extend through the entire dermis and into underlying fat and connective tissue and require automatic referral to a burn center.1,3,5 These burns appear white, waxy, dry, and leathery. Pain sensation is reduced because nerve endings have been destroyed.1,3 Surgical intervention and skin grafting are needed when burns extend beyond the superficial dermal layer, and healing usually takes three weeks or more.5,6


Estimating the percentage of total body surface area (TBSA) involved is also critical to managing burn injuries. Three commonly used tools to quickly approximate the involved surface area are the rule of nines, Lund and Browder charts, and the palm method.1,3 Superficial burns are not included in these calculations. Although the rule of nines allows for a faster assessment, Lund and Browder charts provide a more accurate estimation in children and adults, with surface area adjusted to age.1,3,9 An illustration of these methods is available at https://www.aafp.org/afp/2012/0101/p25.html#afp20120101p25-f1. The palm method uses the palm of child and adult patients as a visual estimate of the size of small scattered burns. The palm equals approximately 0.5% TBSA. The entire palm including fingers is approximately 1% TBSA.9 Although it is simple to use, the palm method may overestimate surface area in large burns.9
Treatment
Most patients with burns of up to 10% TBSA can be managed successfully as outpatients.3,10–12 The American Burn Association has published criteria for burn center referral (Table 1).10,11 Burn injuries are considered trauma, and all patients with burns, even in the outpatient setting, should be assessed for concomitant injuries according to Advanced Trauma Life Support or Advanced Burn Life Support guidelines.13
| Burns to the face, hands, feet, major joints, genitalia, or perineum |
| Children in health care facilities without staff trained to treat children or appropriate equipment for children |
| Concurrent trauma |
| Electrical or chemical burns |
| Full-thickness (third-degree) burns at any age |
| Greater than 10% total body surface area involved |
| Inhalation injuries |
| Need for special support (social, emotional, rehabilitative) |
| Preexisting medical issues that may complicate treatment or recovery or increase mortality risk |
Injuries to the face and neck and exposure to fire in an enclosed space or to chemicals predispose patients to airway injury and warrant close monitoring for airway compromise.14 A rapid history directed at identifying the causative agent and determining the depth and extent of the burn is important. Judging initial burn depth can be difficult.1 Slow or absent skin blanching indicates a deep lesion, whereas pain level is inversely proportionate to burn depth.
Burn injuries are dynamic in nature, and even minor-appearing injuries can worsen with time (burn wound conversion) and need to be reassessed in 24 to 72 hours.14,15 Superficial partial-thickness burns can deepen spontaneously to deep partial-thickness or full-thickness involvement within 48 hours. Depth can also increase because of inadequate treatment or superinfection.15
For all types of minor burn injuries, the goals of initial treatment are to minimize the extent of the burn, clean the wound, and address pain.13,14 For scalds, immediate clothing removal lessens burn injury.16 For chemical burns, all clothing is assumed to be contaminated and should be removed using appropriate protective equipment, such as eye protection and gloves.17 It is important to ensure the removal of all items that can cause a tourniquet effect when a body part swells, such as jewelry, belts, watches, and diapers.14,18 Because patients with burns have impaired thermoregulation, the environment should be kept warm during examination.14,18
Active cooling of the burn surface with running tap water (at 46.4°F [8°C] to 77°F [25°C]) for at least 20 minutes has been shown to reduce burn depth, improve healing time, and decrease grafting requirements.14,16,19,20 Cooling should commence within 30 minutes of the initial burn, but emerging evidence suggests this benefit may be achieved up to three hours after the burn.19 Wet dressings are not effective at cooling wounds.14 Ice should not be used because of its vasoconstrictive effects and risk of further tissue injury.14 Contaminants and nonadherent necrotic skin should be removed with gentle irrigation to prevent infection.13,18 Irrigation with tap water instead of sterile or antiseptic agents does not increase infection rates.13,21–23
Superficial burns do not require dressings to promote healing; however, covering burns with wet gauze may reduce pain.18,24 Aloe vera cream and nonsteroidal anti-inflammatory drugs may also assist with pain control.18,25,26 Superficial partial-thickness burns require a moist, protected environment to promote reepithelialization while preventing desiccation, burn progression, and secondary infection.1
Blistering mostly occurs with superficial partial-thickness burns, and management is controversial.15,18 Characteristics that favor debridement include size greater than 6 mm, location over joints, and high likelihood of spontaneous rupture.13,18 Debridement reduces pressure on the wound; removes necrotic skin, which may act as a nidus of infection; allows visualization of the wound bed; and permits placement of an antibacterial dressing directly over intact skin.15,27 Recent evidence suggests that deroofing blisters is not superior to aspiration in regard to pain reduction and wound healing.28
Two methods of dressing partial-thickness wounds are commonly practiced. A systematic review has demonstrated no difference in wound healing rates between the two methods.29
In the first method, a topical antimicrobial agent is applied with a simple dressing that is changed every 12 to 24 hours to allow for monitoring of burn progression.18,27 Silver sulfadiazine (Silvadene) is the most popular topical antibacterial agent for burns, although evidence of its benefit in the prevention or control of infection in patients with burns is lacking. Silver sulfadiazine has been shown to delay wound healing by impairing leukocytes and epidermal growth, which can increase scar formation.30 Additionally, a Cochrane review suggests an association between silver sulfadiazine and increased burn wound infection rates.31 Table 2 lists topical agents commonly used in the treatment of burns.18,30,32,33
| Agent | Description | Advantages | Disadvantages |
|---|---|---|---|
| Bacitracin | Antimicrobial ointment | Inexpensive, painless, can be used on the face and near mucous membranes | Narrow microbial coverage, need for frequent dressing changes, does not penetrate eschar, may cause urticaria or burning |
| Impregnated nonadherent gauze (Xeroform, Vaseline gauze) | Semiocclusive, nonabsorptive dressing | Nonadherent barrier, secondary dressing over absorptive dressing, helps maintain moist environment, clings to the body | No antimicrobial activity |
| Mafenide acetate (Sulfamylon) | Water-based cream; bacteriostatic against gram-positive and gram-negative bacteria | Pseudomonal coverage, penetrates eschar, used for deep burns or exposed cartilage, can be used on the face | Pain associated with application, may delay wound healing, associated with metabolic acidosis |
| Medical grade honey | Variety of preparations, including topical and honey-based hydrogel-impregnated dressings | Inhibits growth of common burn pathogens, reduces healing time for partial-thickness burns compared with simple dressings | Low-quality evidence |
| Mupirocin | Ointment; inhibits bacterial protein and RNA synthesis, bactericidal at high concentrations | Good gram-positive antimicrobial coverage, active against most strains of methicillin-resistant Staphylococcus aureus, painless, may be used on the face | Need for frequent dressing changes, expensive |
| Silver sulfadiazine (Silvadene) | Water-based cream; interferes with bacterial DNA synthesis | Painless, long shelf life, broad antimicrobial coverage | Need for frequent dressing changes; delays wound healing; associated leukopenia; stains tissues; contraindicated in pregnant women, nursing mothers, newborns, and those with a sulfa allergy |
With the second method, advanced dressings of various materials are applied to the wound and kept in place for up to 14 days, depending on manufacturer specifications.13,29 Advanced dressings have inherent antimicrobial properties, keep injured tissue moist, and control exudative fluids. Silver-impregnated foam dressings are standard at outpatient burn clinics because they only require one or two dressing changes until reepithelialization.24 This alleviates home dressing changes and associated patient discomfort, which is especially helpful in children.24 Table 3 lists advanced dressings commonly used in the treatment of burns.14,18,32
| Dressings | Description | Advantages | Disadvantages |
|---|---|---|---|
| Hydrocolloids (Duoderm) | Hydrophilic absorptive dressing with a viral and bacterial barrier; facilitates autolytic debridement | Can remain in place for up to seven days, good for management of light to moderate exuding wounds while keeping wound moist, shorter time to wound closure than silver sulfadiazine (Silvadene), assists in scar management, inexpensive | Cannot be used for large exuding wounds, malodorous |
| Silicone (Mepitel) | Nonabsorptive, transparent, open mesh, polyamide net coated with a soft silicone layer | Can remain in place for up to 14 days, conforms to the shape of the wound, allows for drainage of exudate to secondary bandage | Expensive |
| Silver impregnated | |||
| Acticoat | Layered nanocrystalline silver-coated mesh surrounding an inner rayon layer | Three-day and seven-day versions, broad antimicrobial coverage | Cannot be used with magnetic resonance imaging, may not completely clear wound of bacteria, some pain with initial application, temporary skin staining, may dry out and adhere (moistened secondary dressing should be used for optimal moisture level), cannot be used with oil-based products |
| Aquacel Ag | Absorptive carboxy-methylcellulose sodium fiber dressing | Can remain in place for up to seven days, requires fewer dressing changes than with other silver-based dressings, painless, nonadhering, broad antimicrobial spectrum, facilitates debridement | Cannot be used with oil-based products, amount of exudate dictates frequency of changes |
| Mepilex Ag | Absorptive silicone foam dressing | Can remain in place for up to seven days, decreases pain, antimicrobial, maintains moist environment | Expensive, cannot be used with magnetic resonance imaging, cannot be used with hypochlorite solutions or hydrogen peroxide |
Pain medication should be given early during treatment.24 Pain from superficial burns can often be treated with oral pain medications, such as ibuprofen and acetaminophen. Topical aloe vera and emollient moisturizers with wet gauze dressings have been shown to reduce pain.34 Patients with partial-thickness burns may require opioids for acute pain control (parenteral route in children) and should be administered 30 minutes before anticipated dressing changes.24,35 Studies have supported the use of pregabalin (Lyrica) as an adjunct for acute burn pain.36
Prophylactic antibiotics do not affect morbidity and may increase bacterial resistance.24,31 Because burn wounds are prone to tetanus infection, tetanus immunization status should be determined for patients with partial- and full-thickness burns.13 Patients who have completed a three-dose primary tetanus vaccine and received a booster in the previous five years are considered protected against tetanus, according to the Centers for Disease Control and Prevention.37 Vaccination and administration of tetanus immune globulin are recommended when tetanus vaccination status is unknown or inadequate (less than three doses of vaccines containing tetanus toxoid have been administrated).13,14,37 Fever during the first 72 hours after a burn is common because of hypermetabolism and can be treated with anti-pyretics alone. Fever after 72 hours or systemic signs of infection warrant inpatient treatment.24,32
Persons with diabetes mellitus are more likely to present for medical care more than 24 hours after a burn injury because of preexisting neuropathy.38 A 10-year retrospective analysis showed that burn patients with diabetes had an overall complication rate of 90%, with 44% developing local infection.39 In persons without diabetes, cellulitis is typically caused by Staphylococcus aureus or Streptococcus pyogenes, whereas persons with diabetes are at increased risk of gram-negative infection, and wound culture may be helpful in management.32 Burn patients with diabetes who develop complications, such as cellulitis, should be referred to a burn center for further treatment.38
Long-Term Prognosis
Patients with burns expected to take longer than 14 days to heal should be referred to a burn specialist because of the risk of hypertrophic scarring.15 Permanent hyperpigmentation may occur in newly epithelialized skin exposed to direct sunlight; therefore, sunscreen with a sun protection factor of at least 50 should be used, and direct sunlight should be avoided for up to two years.27
Pruritus is common following reepithelialization and can be treated with moisturizers to keep the skin hydrated, cool cloths, massage, and oatmeal preparations.13 For moderate to severe pruritus, oral antihistamines are recommended as first-line therapy with cetirizine (Zyrtec) demonstrating superiority over diphenhydramine (Benadryl).32 Gabapentin (Neurontin) has also been shown to be beneficial.13,32
Neuropathic pain is more common with full-thickness burns and warrants referral to a burn center for specialized testing and possible surgical decompression.40
A significant proportion of childhood burn injuries are the result of child abuse or neglect. A study from the National Burn Repository indicated that 5.8% of childhood burn admissions are the result of abuse.41 Although anatomic location of the burn may be an unreliable indicator of abuse, burns to feet, buttocks, and posterior legs and hands are more likely to be nonaccidental.8,24 Additionally, a history that is incongruent with the injury and the presence of other unrelated injuries are indications for an inpatient abuse evaluation.1
Prevention
Identification of high-risk populations and common mechanisms of injury is key to developing an effective burn prevention strategy.10 Two populations especially vulnerable to burns are children and older adults. From 2011 to 2015, almost one-fourth of all burns occurred in children younger than 15 years.42 In 2015, unintentional fire and burn injuries were the third leading cause of injury-related deaths among U.S. children three to nine years of age and the eighth leading cause of all deaths among adults 65 years and older.2,10,42 Sunburns are the most common and preventable type of burns in children, affecting up to 50% of children before 11 years of age.3 Table 4 lists common sunburn prevention strategies.43,44 Scalds are the most common type of burns in children five years or younger and are often a result of spilling hot liquids during cooking.10 Bathing-related scalds are most common with sink bathing when a child may inadvertently turn on the hot water or the temperature of running water may fluctuate.45 Table 5 lists childhood burn prevention strategies.46,47
| Avoid outdoor activities during peak sun intensity (10 a.m. to 4 p.m.), even on cloudy days |
| Wear protective clothing (e.g., long sleeves, long pants, wide-brim hats) during the day |
| For patients at increased risk, consider clothing with a high UV protection factor (> 30) |
| Use sunglasses that provide 100% UVA and UVB protection |
| Use a broad-spectrum sunscreen with an SPF of at least 15 |
| Use a sunscreen that is water-resistant (40 to 80 minutes of protection in the water) |
| Apply sunscreen to dry skin 15 to 30 minutes before exposure to the sun |
| Reapply sunscreen every two hours or earlier when sweating, swimming, or towel-drying |
| Discard any sunscreen older than three years |
| Avoid using tablecloths and place mats because a child could pull them, causing spills |
| Block access to high-risk areas, such as kitchens and bathrooms, with gates or child locks |
| Consider using antiscalding devices or thermometers |
| Do not hang dish towels on the oven door |
| Do not heat formula in a bottle, and never microwave a bottle |
| Do not hold a child and a hot beverage at the same time |
| Do not run water while a child is being bathed, do not bathe a child in a sink; children's baths should be supervised |
| Keep all chairs away from counters and the stove |
| Keep all chemicals, matches, and lighters locked up or out of reach of children |
| Set water heater to 120°F (48.9°C) or lower; for small children, keep water temperature below 101°F (38.3°C) |
| Test all foods and liquids that are microwaved before giving to children |
| Use oven locks |
Older adults are at increased risk of burn injuries because of thinning skin, cognitive decline, decreased sensation, and comorbid medical conditions.48 Frailty in older patients predicts morbidity and mortality from burns.49 Although they are among the fastest growing population in the United States, adults 60 years and older are the least likely to be targeted for burn prevention.50 Table 6 lists key strategies for burn prevention for older adults.51
| Kitchen safety Consider devices that turn off the stove automatically when the pot is removed Ensure easy access to the fire extinguisher Turn pot handles inward to reduce accidental splattering Wear tight-fitting clothes and avoid long sleeves around the stove |
| Bathroom safety Check the water temperature before washing Install antiscalding devices that stop water flow when too hot Install railings and easy-access tubs and showers to prevent falls Obtain assistance with bathing if needed Set water heater to 120°F (48.9°C) or less |
| Home safety Avoid using space heaters and candles Ensure electrical cords, appliances, and outlets are in working condition Ensure heating pipes are covered Ensure smoke and carbon monoxide detectors are installed and working properly on every level of the home and in all bedrooms |
This article updates previous articles on this topic by Morgan, et al.,7 and Lloyd, et al.8
Data Sources: PubMed, Essential Evidence Plus, the Cochrane database, and Ovid were searched using the key terms burn management, burn prevention, burn prevalence, outpatient burns, topical burn treatment, sunburn, sunburn management, partial thickness burns, diabetics burns, burn dressings, and water burn treatment. The Agency for Healthcare Research and Quality, the Centers for Disease Control and Prevention, American Burn Association, American Association of Retired Persons, and SafeKids.org websites were also searched. Search dates: April 2, 2019; June 1, 2019; September 3, 2019; and December 28, 2019.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army Medical Department or the U.S. Army at large.