Am Fam Physician. 2020;101(8):499-501
Author disclosure: No relevant financial affiliations.
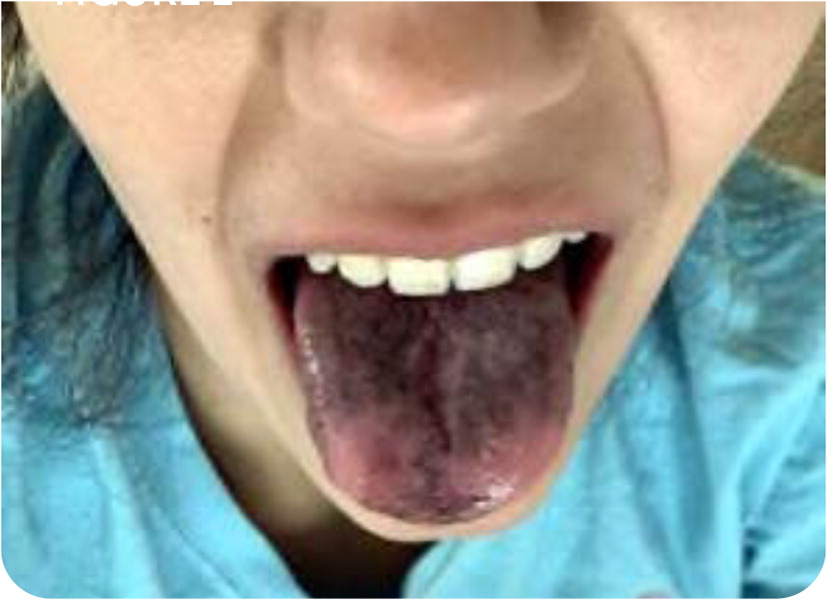
A 25-year-old woman presented with a one-month history of rapid heartbeat, lightheadedness, feeling faint with standing, and nausea. She had lost 13 lb (6 kg). She also reported darkening of her skin, tongue, and lips over the previous two weeks. The patient had a history of Hashimoto thyroiditis, which was diagnosed at 12 years of age. The patient was not taking any medications.
On physical examination, her systolic blood pressure was 100 mm Hg, and she was mildly tachycardic. There were multiple small, dark macules on her tongue and hyperpigmentation on her lip mucosa and the dorsal surfaces of the distal and proximal interphalangeal joints on both hands (Figure 1 and Figure 2).

Question
Discussion
The answer is E: primary adrenal insufficiency (Addison disease). Hyperpigmentation is present in almost all patients with primary adrenal insufficiency. The patchy hyperpigmentation is generalized but most often notable in areas exposed to light, chronic friction, or pressure.1 In this patient, a history of an autoimmune endocrine condition and the fatigue, hyperpigmentation, and vital signs prompted concern for adrenal insufficiency. An early morning (4 to 8 a.m.) serum cortisol measurement was 0.6 mcg per dL (16 nmol per L), which is significantly lower than the normal range of less than 10 to 20 mcg per dL (276 to 552 nmol per L). An adrenocorticotropic hormone stimulation test was performed, confirming the diagnosis of Addison disease.
Cortisol deficiency causes an increased production of pro-opiomelanocortin, a prohormone that is cleaved into active adrenocorticotropic hormone and melanocyte-stimulating hormone. The increase in melanocyte-stimulating hormone leads to increased melanin synthesis, which causes the hyperpigmentation in patients with Addison disease.2 The skin changes occur mostly on the inner surface of the lips and buccal mucosa, tongue, and gingival border. The bronze diffuse hyperpigmentation and darkening of skin may occur over areas exposed to light, chronic friction, or pressure. The skin lesions themselves do not cause symptoms. Hyperpigmentation typically fades within a few months of adequate glucocorticoid therapy, but the mucosal and tongue changes may take longer to resolve. Patients with one autoimmune endocrine disorder are at risk of others, which should be considered.
Some medications can cause generalized patchy hyperpigmentation of the tongue and oral mucosa. Drug-induced hyperpigmentation has several mechanisms depending on the medication ingested. Drugs containing heavy metals such as iron or gold cause deposition of metals into the skin. Other drugs form complexes with melanin or directly stimulate hypermelanosis. Medications that may cause hyperpigmentation include bismuth subsalicylate (Pepto-Bismol), antibiotics (tetracycline, linezolid [Zyvox]), proton pump inhibitors, interferon, antipsychotics (chlorpromazine and related phenothiazines), anticonvulsants (phenytoin [Dilantin]), anti-malarials (chloroquine, hydroxychloroquine [Plaquenil]), cytotoxic drugs (cyclophosphamide, bleomycin, doxorubicin [Adriamycin]), and some antidepressants.3
Lingua villosa nigra (black hairy tongue) presents as elongated filiform papillae and yellow to brown discoloration of the tongue surface. The condition is associated with poor oral hygiene, smoking, Candida albicans infection, and some antibiotics (e.g., minocycline [Minocin], linezolid).4 The hyperpigmentation is due to bacteria trapped in the filiform papillae that produce porphyrins.
Peutz-Jeghers syndrome, an inherited polyposis syndrome, typically presents during the first one to two years of life and is associated with hyperpigmented mucocutaneous macules. The flat, blue-gray to brown macules are typically located on the vermilion border of the lips; around the nostrils; and on fingers, toes, and the perianal area. Patients with Peutz-Jeghers syndrome have a much higher risk of developing intestinal cancers. The hyperpigmented lesions increase in number and size and fade after puberty, with the exception of those on the buccal mucosa, which may persist throughout adulthood.5 The hyperpigmentation is due to pigment-laden macrophages in the dermis.
Pigmented fungiform papillae of the tongue is a benign oral pigmentation variant that occurs most often in individuals with darker skin tones. The hyperpigmentation may be pink, red, or dark and typically occurs on the anterior and lateral aspects of the tongue. The hyperpigmented spots are due to the melanin deposition in the tips of the fungiform papillae and appear around 20 to 30 years of age.4,6
| Condition | Characteristics |
|---|---|
| Drug-induced hyperpigmentation | Generalized patchy hyperpigmentation of tongue and oral mucosa |
| Lingua villosa nigra (black hairy tongue) | Elongated filiform papillae and yellow to brown discoloration of tongue surface |
| Peutz-Jeghers syndrome | Hyperpigmented mucocutaneous macules that are flat and blue-gray to brown; typically on the vermilion border of the lips; around the nostrils; and on fingers, toes, and the perianal area |
| Pigmented fungiform papillae of the tongue | Pink, red, or dark hyperpigmented spots, typically on the anterior and lateral aspects of the tongue |
| Primary adrenal insufficiency (Addison disease) | Generalized, patchy hyperpigmentation of the inner surface of lips and buccal mucosa, tongue, and gingival border; bronze diffuse hyperpigmentation and darkening of skin may occur over areas exposed to light, chronic friction, or pressure |