Am Fam Physician. 2020;102(1):10
Author disclosure: No relevant financial affiliations.
Buprenorphine prescribing in primary care is a key bottleneck in the access to medications for opioid use disorder (OUD). In a Medicare claims study including family medicine, internal medicine, general practice, and psychiatry, the largest share of buprenorphine prescribers were family physicians. Given that family physicians care for patients of all ages and in a broad variety of settings, including urban and rural areas, they have the potential to dramatically improve national access.
Nearly two decades after Congress approved the use of Drug Addiction Treatment Act of 2000 waivers for prescribing buprenorphine, patients continue to struggle with access to office-based buprenorphine prescriptions—with nearly half a million deaths attributable to OUD over the past two decades.1 Health outcomes for patients with this chronic disease improve with continuous access to buprenorphine,2 often requiring close to weekly follow-up while patients stabilize.
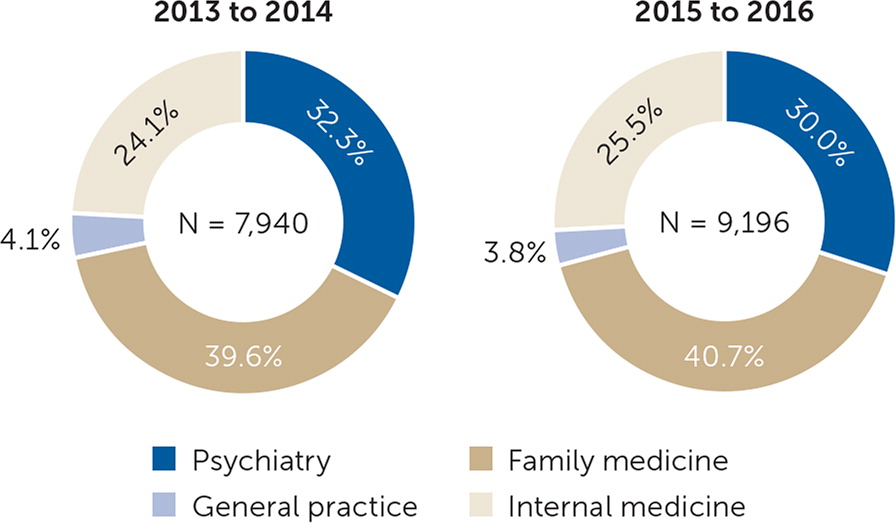
A 2020 Medicare claims study revealed that only about one in 50 primary care physicians participating in Medicare Part D prescribed buprenorphine between 2013 and 2016.3 This analysis examined primary care physicians (i.e., from family medicine, internal medicine, and general practice) and psychiatrists to identify characteristics of buprenorphine prescribers vs. nonprescribers.
In the study, psychiatry had the highest proportion of buprenorphine prescribers among the specialties studied at 10.8%, although broader access to medications for OUD among Medicare patients hinged on the 70% majority of nonpsychiatrist primary care prescribers.3 Family medicine had the highest volume of buprenorphine prescribers (Figure 1) but also had the most room for growth; 97.6% of family physicians were not buprenorphine prescribers.3
Primary care physicians who were less likely to prescribe buprenorphine had more recently completed residency training, were women, practiced outside the Northeast region of the United States, graduated from international medical schools, had more Medicare patients, and had more nonwhite patients per panel.3
Results of this study highlight the need for medical education reform. Training to effectively provide medications for OUD cannot be left to chance—graduate and continuing medical education leaders must consider this as a core competency for residents and practicing physicians alike to meet the population's needs, particularly patients in rural and urban communities with health professional shortages.4
The information and opinions contained in research from the Graham Center do not necessarily reflect the views or the policy of the AAFP.
A collection of Graham Center Policy One-Pagers published in AFP is available at https://www.aafp.org/afp/graham. One-Pagers are available from the Graham Center at https://www.graham-center.org.