Am Fam Physician. 2020;102(1):19-28
Related letter: Low Specificity Limits Use of Test for Spondylolysis in Children and Adolescents
Author disclosure: No relevant financial affiliations.
Back pain is a relatively common presenting symptom in children and adolescents. Typical causes include muscle strain or spasm, spinal deformities (e.g., Scheuermann kyphosis, adolescent idiopathic scoliosis), spondylolysis, bulging or herniated intervertebral disks, apophysitis of the iliac crest, and functional pain syndromes such as fibromyalgia. Spondyloarthropathies such as ankylosing spondylitis may present with low back pain and stiffness, which are often worse in the morning. Less common but more serious causes include malignancy and infections. The physical examination should include postural inspection, evaluation for tenderness, range of motion, strength testing, and testing for fractures and nerve impingement. Treatment for patients with muscle strain include relative rest, home-based exercises, physical therapy, and limited use of nonsteroidal anti-inflammatory drugs. If findings from the history and physical examination suggest underlying pathology, radiography and laboratory studies are indicated initially; magnetic resonance imaging, computed tomography, or a bone scan may be needed for further evaluation. It is generally accepted that the following factors warrant immediate evaluation: patient age younger than five years, symptoms persisting beyond four weeks, systemic symptoms, nighttime pain, bowel incontinence/urinary retention, or other neurologic symptoms.
Back pain is a relatively common condition in children. A 2011 Danish study found a prevalence of 28% to 48% in school-aged children, with increasing incidence in older adolescents.1 Care was sought in less than one-third of cases.1 One large cohort study found associations between back pain and age greater than 12 years, a family history of back pain, spending more than two hours per day studying or watching television, an uncomfortable school desk, widespread pain, and sleep problems.2 Evidence is mixed on the effect of heavy backpacks.3 Back pain in children should be assessed carefully because it can limit participation in sports, activities, and school. An estimated 10% to 15% of affected children will develop chronic low back pain later in life.4
History
An accurate history is essential in differentiating etiologies of back pain. Timing, onset, severity, location, frequency, and characteristics of the pain (e.g., whether it radiates) should be addressed. School-aged children should be asked about recent illness, trauma, and nonaccidental injuries. Symptoms that warrant urgent evaluation for rare conditions are listed in Table 1. Patients with spondyloarthropathy may have back stiffness in the morning or a family history of rheumatologic disorders.5 Table 2 and Table 3 present suggested approaches for the evaluation and management of common causes of acute and chronic back pain.
| Diagnosis | Symptoms | Special considerations | Evaluation | Management |
|---|---|---|---|---|
| Diskitis or vertebral osteomyelitis | Gradual onset of irritability and back pain without systemic toxicity; limping; refusal to crawl, walk, or bend forward | More common in children younger than 5 years | Radiographic findings may be normal initially, but within 2 to 3 weeks will show narrowing of intervertebral space MRI is best imaging modality to show disk and adjacent vertebral end plates and can help differentiate between diskitis and vertebral osteomyelitis | Antibiotics with activity against Staphylococcus aureus and Kingella kingae |
| Epidural abscess | Fever, neurologic deficits, spinal pain | Extremely rare in immunocompetent patients | Urgent MRI | Urgent referral to neurosurgery |
| Neoplasm | Unremitting nighttime pain, weight loss, myelopathic symptoms (e.g., gait instability, weakness) | History of previous malignancy | MRI Complete blood count, C-reactive protein level, erythrocyte sedimentation rate | Urgent referral to neurosurgery |
| Septic sacroiliitis | Fever, limping, pain over sacroiliac joint | Bimodal distribution: children 6 to 48 months of age and adolescents | MRI Laboratory test results consistent with infection | Antibiotics with activity against S. aureus and K. kingae; aspiration and culture in patients who do not respond to antibiotics |
| Syringomyelia | Pain and stiffness in back and shoulders; symptoms worsen with postural changes or Valsalva maneuver | Cervical syringomyelia can be associated with Arnold-Chiari malformation | Contrast-enhanced MRI shows fluid-filled, gliosis-lined cavity within the spinal cord at C2-T1, and possibly congenital anomalies | Urgent referral to neurosurgery for patients with functional decline |
| Tethered cord syndrome | Back pain exacerbated by exercise, bladder dysfunction, calf muscle atrophy, diminished or absent deep tendon reflexes, dermatomal sensory loss, leg weakness | Progressive scoliosis | MRI Physical examination may reveal weak ankle dorsiflexion in older children (usually the earliest sign of motor dysfunction) | Urgent referral to neurosurgery |
| Transverse myelitis | Back pain, bowel or urinary dysfunction, sensorimotor deficits | Signs and symptoms may not correlate to a specific vertebral level | Urgent evaluation indicated: contrast-enhanced MRI, cerebrospinal fluid analysis | Urgent evaluation in emergency department |
| Diagnosis | Presentation | Associated findings | Evaluation | Management |
|---|---|---|---|---|
| Herniated disk | Acute injury, low back pain radiating to leg | Radicular pain, positive straight leg raise test, decreased lumbar flexion | Radiography; MRI if no response to at least 6 weeks of conservative treatment | Relative rest, physical therapy; surgery for refractory cases |
| Muscle strain | Paraspinal pain | Muscle tenderness without radiation | No imaging required | Relative rest; physical therapy if persistent |
| Tumor or infection | Nighttime pain with fever or other generalized symptoms | Weight loss | Urgent radiography and MRI | Urgent evaluation in emergency department or by specialist |
| Vertebral fracture | Acute injury, focal midline pain | Other injuries, radicular pain, weakness | Urgent radiography and MRI | Urgent evaluation in emergency department |
| Diagnosis | Presentation | Associated findings | Evaluation | Management |
|---|---|---|---|---|
| Fibromyalgia and chronic widespread pain | Generalized widespread pain lasting at least 3 months with fatigue, nonrestorative sleep, and/or cognitive symptoms; tenderness to touch and sensitivity to sounds, lights, and smells | Most common in adolescents; functional illness is rare in children younger than 9 years; symptoms not limited to back | 2010 American College of Rheumatology criteria* may replace older criteria | Multidisciplinary approach: education, exercise, cognitive behavior therapy, and optional pharmacotherapy, including tricyclic antidepressants |
| Idiopathic scoliosis | Progressive constant pain with associated spinal deformity | Older age | Full spine radiography; consider other causes of back pain, including spondylolysis | Referral for all children younger than 12 years and for those with progressive scoliosis, significant pain, structural defects (hemivertebra), or Cobb angle > 20 degrees (especially > 40 degrees) |
| Iliac crest apophysitis | Tender area along iliac crest; pain (usually gradually worsening) with activity, especially running, jumping, kicking, or twisting | Skeletally immature 12- to 17-year-old patient; higher risk in those with tight hip or thigh muscles | Point-of-care ultrasonography showing tenderness with sonopalpation (i.e., palpation with the ultrasound probe) | Relative rest, icing or nonsteroidal anti-inflammatory drugs as needed; exercises, stretching, and possibly physical therapy |
| Inflammatory spondyloarthropathy | History of uveitis, polyarthritis, or stiffness | Morning stiffness, sacroiliac joint tenderness | Radiography, human leukocyte antigen B27 and rheumatoid factor testing, erythrocyte sedimentation rate, C-reactive protein level | Referral to pediatric rheumatologist |
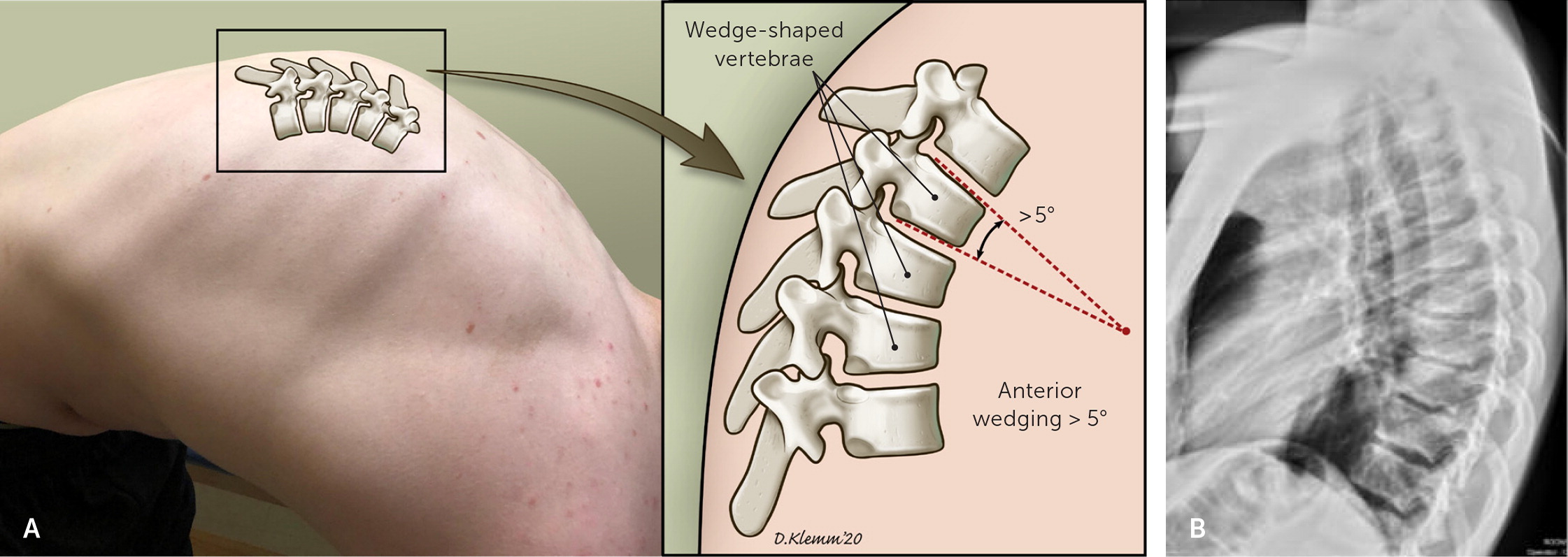
| Scheuermann kyphosis | Stooped posture, upper back pain | Rigid kyphosis | Radiography and MRI for severe symptoms refractory to physical therapy | Reassurance, physical therapy; surgical referral for limitations in breathing or refractory pain |
| Spondylolysis | Pain with lumbar extension that may radiate down the leg | Hamstring tightness, positive stork test, reduced range of motion with lumbar extension | Radiography; MRI if negative or concern for active stress fracture | Relative rest, physical therapy; bracing for constant pain |
Physical Examination
Examination of children and adolescents with back pain begins with a visual inspection of the back and standing posture. Gait testing should include heel and toe walking; children with diskitis may refuse to walk. Spasticity, ataxia, muscle atrophy, and instability suggest spinal cord impingement or muscular dystrophy. Signs of midline defects, such as dimples, hemangiomas, or hair patches, suggest underlying congenital spinal lesions. Curvature or accentuated kyphosis may signal scoliosis, Scheuermann kyphosis, or moderate limb length discrepancy. Leg length discrepancies of less than 2 cm are normal and usually not symptomatic.6,7 Palpation of the spinous processes may elicit tenderness in children with spondylolysis, malignancy, or infection. Pain at the iliac crest may occur with apophysitis.8 Range of motion should be assessed (Figure 1) to determine whether the back pain worsens with lumbar extension (spondylolysis) or flexion (discogenic conditions).

Strength testing of the hips, knees, and ankles can evaluate for weakness related to pain or neuropathy. Dermatomal numbness and paresthesias suggest a nerve root lesion. Patellar and Achilles reflexes should be assessed, and a Babinski test may be performed to evaluate for upper motor neuron injury. The slump test (Figure 2) and straight leg raise test evaluate for sciatica; pain radiating to the gluteal area or down the leg indicates a positive test. In the Patrick (FABER) test, the examiner flexes, abducts, and externally rotates the patient's hip to stress the sacroiliac joint (eFigure A). Ipsilateral pain elicited by this maneuver indicates sacroiliitis, which in turn suggests ankylosing spondylitis. The Thomas test can be performed to determine hip flexor tightness. With the patient in the supine position, the examiner uses both hands to bring one knee to the chest. The test is positive if the contralateral leg lifts off the table. In the stork test, the patient stands on one leg and hyperextends the lumbar spine (Figure 3); ipsilateral pain suggests spondylolysis, although the sensitivity (50% to 73%) and specificity (17% to 32%) are low.9 Lastly, quadriceps and hamstring tightness should be assessed; inflexibility is associated with spondylolysis and typically worsens as children progress to adolescence.9,10



Imaging
Guidelines from the American College of Radiology state that imaging in children and adolescents can be delayed unless the patient has abnormal neurologic findings or pain that occurs at night, radiates, or persists beyond four weeks.11 Plain radiography should be performed in patients with any of these findings.12 Anteroposterior and lateral views are often sufficient, even when evaluating for spondylolysis.13 Oblique views double the radiation exposure and do not significantly improve sensitivity; therefore, they are no longer recommended in the evaluation of spondylolysis.14
Magnetic resonance imaging (MRI) should be considered for patients with localized pain who have normal radiographic findings. MRI can detect tumors, infections, and disk herniation, and it can assess for edema in the pars interarticularis region, which is consistent with acute spondylolysis.12,14 A bone scan may be indicated if MRI findings are inconclusive or in children with diffuse back pain. However, bone scans do not detect soft tissue tumors or infections that do not stimulate bone metabolism, and therefore may miss a critical condition. Computed tomography (CT) shows bony architecture and soft tissues but does not show marrow elements. CT can be performed quickly and generally does not require sedation, but it may expose children to significant ionizing radiation.
Laboratory Testing
A complete blood count with differential, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level should be obtained if there is concern for malignancy or inflammatory conditions (e.g., spondyloarthropathies, juvenile rheumatoid arthritis, infections). Although an elevated ESR (more than 20 mm per hour) and/or CRP level (more than 1 to 2 mg per dL [10 to 20 mg per L]) is nearly 95% sensitive for osteomyelitis, the specificity is low (60%).15 The presence of human leukocyte antigen B27 is strongly associated with seronegative spondyloarthropathy (ankylosing spondylitis, reactive arthritis, and spondylitis associated with psoriasis and inflammatory bowel disease), but because of high false-positive rates, testing should be reserved for patients with high clinical suspicion, such as those with morning stiffness, night pain that improves with exercise, or sacroiliac pain. Other tests (e.g., rheumatoid factor, antinuclear antibodies, antistreptolysin O, Lyme disease testing) could be considered in the presence of associated findings, but they generally are not useful.16 Axial spondyloarthropathy should be considered if clinical symptoms occur and MRI findings are negative; this condition is associated with elevated ESR and/or CRP levels in approximately 40% of cases.17 If there is concern for axial spondyloarthropathy, consultation with a pediatric rheumatologist may be warranted.
Treatment
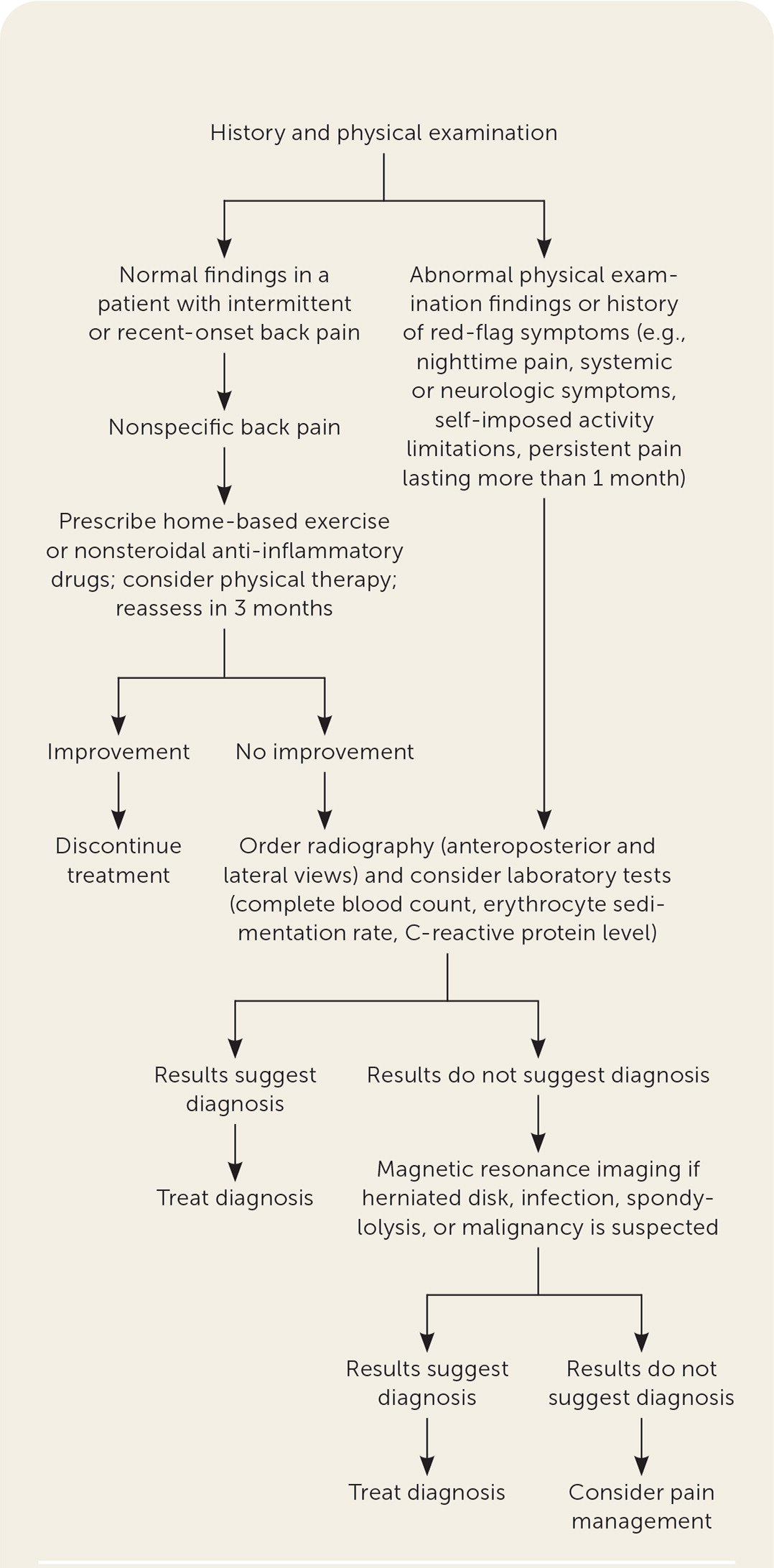
The approach to treating back pain in children and adolescents depends on the etiology and clinical course. For benign causes, relative rest, limited use of nonsteroidal anti-inflammatory drugs, and close follow-up without imaging is warranted. Physical therapy can be helpful for core strengthening and lower extremity flexibility, and Pilates is potentially useful based on its positive effects on quality of life in patients with juvenile idiopathic arthritis18 (Figure 4). Treatments for specific conditions are addressed below. An algorithm for the evaluation and treatment of back pain in children and adolescents is presented in Figure 5.19 Continued monitoring and close follow-up within four weeks can potentially diagnose serious conditions early.

Common Causes
LUMBAR MUSCLE STRAIN OR SPASM
Although published incidence studies are limited, many cases of low back pain in children who present to a primary care setting are attributed to a lumbar muscle strain or spasm.20 Muscle spasm may be related to growth, resulting in tight hamstrings and quadriceps that cause a posterior pelvic tilt. An association between heavy backpacks and back pain is controversial. However, the American Academy of Pediatrics recommends that backpacks not exceed 10% to 20% of the child's weight.3,21 Most cases of lumbar strain or nonspecific back pain respond to conservative management, including activities as tolerated, postural exercises, and lower extremity stretching.20 Pain usually resolves within a few weeks.20
SPONDYLOLYSIS AND SPONDYLOLISTHESIS
Spondylolysis is a stress injury to the pars interarticularis. Spondylolisthesis occurs when there is a bilateral pars injury with translation of one vertebral body over another (Figure 6). Spondylolysis affects up to 6% of all children, but the incidence among athletes is unclear.4,22 The primary sites include L5 (71% to 95%) and L4 (5% to 23%), but it can occur at any level.22 Although spondylolysis is common among athletes whose sports require repetitive lumbar extension (e.g., gymnasts, football linemen, divers, baseball players), it can occur in any athlete.11 Pain tends to be focal, may be associated with tenderness to palpation of the spinous process, and worsens with extension. A positive stork test is concerning for spondylolysis; other associated findings include tight quadriceps and hamstrings.23 Anteroposterior and lateral radiographs may show a fracture of the pars inter-articularis.22 If radiographic findings are negative, patients can be treated conservatively for six weeks.22 If pain persists, MRI sequenced to detect bone marrow edema in the pedicle and pars region is the preferred next step; single-photon emission CT is indicated if MRI is not available.11,22

More than 90% of patients with spondylolysis respond to conservative treatment, such as relative rest, flexibility exercises for the quadriceps and hamstrings, and core strengthening with a guided exercise program.23,24 Although bracing has not been conclusively proven to accelerate healing, it can be helpful for pain control if other conservative measures are ineffective.24 If bracing is indicated, a low thoracolumbar orthosis (Figure 7) is as effective as a high thoracolumbar orthosis.25 The duration of bracing depends on symptom response: It should be tapered when the patient is pain free, regardless of radiographic healing.26 Research has not shown that limited used of nonsteroidal anti-inflammatory drugs delays bone healing in children, as has been postulated in adults.27 Case studies have shown that acute fractures that do not improve with six weeks of conservative management may respond to transcutaneous electrical nerve stimulation26 (Figure 8). Return to activity should be gradual over approximately five months.28 Surgical management is limited to children who progress to grade 3 spondylolisthesis (50% to 75% vertebral translation), whose pain persists longer than six months, or who develop additional symptoms that are refractory to conservative management.22


SCHEUERMANN KYPHOSIS
Scheuermann kyphosis is osteochondrosis that presents as an abnormality of the vertebral epiphyseal growth plates. Criteria include three or more adjacent vertebrae wedged more than 5 degrees and disk space that narrows in the thoracic region29,30 (Figure 9). Because there is no diagnostic standard for Scheuermann kyphosis, prevalence rates vary widely.29,30 It can be noted in children as young as eight to 12 years who present with a postural deformity that does not resolve with extension or by lying down. Symptoms include gradual onset of pain without trauma over the deformity. Pain can worsen at the end of the day and is relieved with rest.29 Treatment is generally conservative without bracing or orthopedic interventions. Indications for orthopedic intervention include pain that does not respond to nonoperative treatment, neural impairment, and severe deformity (more than 80 degrees) that restricts pulmonary function.30,31 Pain tends to improve with skeletal maturity.32
SCOLIOSIS
Adolescent idiopathic scoliosis is a lateral curvature of the spine of more than 10 degrees. It occurs in 2% to 3% of adolescents.33 Back pain associated with this condition is linked to increasing age, injuries, and severity of curvature.34 Another underlying condition is present in 10% to 35% of children with scoliosis and back pain, such as spondylolysis, spondylolisthesis, Scheuermann kyphosis, or disk herniation35,36; therefore, a careful history and physical examination with appropriate imaging should be performed to evaluate for these and other etiologies. A previous article in American Family Physician addressed the evaluation and treatment of patients with isolated adolescent idiopathic scoliosis.37 Referral to a scoliosis center is indicated if symptoms do not respond to a conservative exercise program.
LUMBAR DISK HERNIATION
Although disk abnormalities on MRI can be common, symptomatic lumbar disk herniations with nerve root impingement are rare.38 Most adolescents with disk herniation (60%) report that an acute event precipitated the pain.38 Although the straight leg raise and slump tests were developed for adults, these tests have been positively correlated with disk herniation in pediatric populations.39 The slump test is more sensitive than the straight leg raise test in patients with lumbar disk herniation (84% vs. 52%, respectively).39 Initial imaging in patients with suspected disk herniation should include lumbar radiographs (anteroposterior and lateral).38 However, MRI is the preferred diagnostic modality and can help evaluate for soft tissue tumors, syringomyelia, or other spinal abnormalities.39 Timing of imaging depends on the concern for other causes of pain, as well as the severity and duration of symptoms. Treatment includes relative rest and physical therapy with lower extremity and core strengthening. Only refractory cases require surgery. If the patient does not improve as expected with conservative treatment, CT should be considered to assess for an occult apophyseal ring fracture, which occurs in the immature lumbar spine when fibers of the intervertebral disk attach to an incompletely fused posterior vertebral body.40 These fractures may require surgery.
This article updates a previous article on this topic by Bernstein and Cozen.41
Data Sources: We searched PubMed, the Cochrane database, the Cochrane Central Register of Controlled Trials, and the National Guideline Clearinghouse using the key words pediatric back pain, Scheuermann's disease, iliac apophysitis, pediatric spondylolysis, spondylolisthesis, pediatric disc herniation, and pediatric lumbar pain. The search included meta-analyses, systematic reviews, randomized controlled trials, clinical trials, guidelines, and diagnostic studies. Search dates: March 2019 to April 2020.
The authors thank Haley Nau and Bri Blonigan for their help with the photos.