
Am Fam Physician. 2020;102(7):389-391
This is one in a series of pro/con editorials discussing controversial issues in family medicine. Related editorial: Would Medicare for All Be the Most Beneficial Health Care System for Family Physicians and Patients? No: Medicare for All Would Cause Chaos and Fail to Control Health Care Costs
Published online August 20, 2020.
The coronavirus disease 2019 (COVID-19) pandemic has exposed several shortcomings in the U.S. health care system. The illusion of reliable employer-based health insurance is crumbling; our safety nets have wide geographic variations; high-deductible insurance plans result in delayed care for people with chronic conditions; and underlying racial and geographic disparities in care are worsening.1–5 The United States spends far more on health care than any other nation, but our life expectancy has fallen behind.6
We must use the lessons of this crisis to better prepare for the next one and address the shortcomings in our health care system. We would have been better positioned to manage acute and chronic health problems during the pandemic if the country had already adopted Improved Medicare for All.
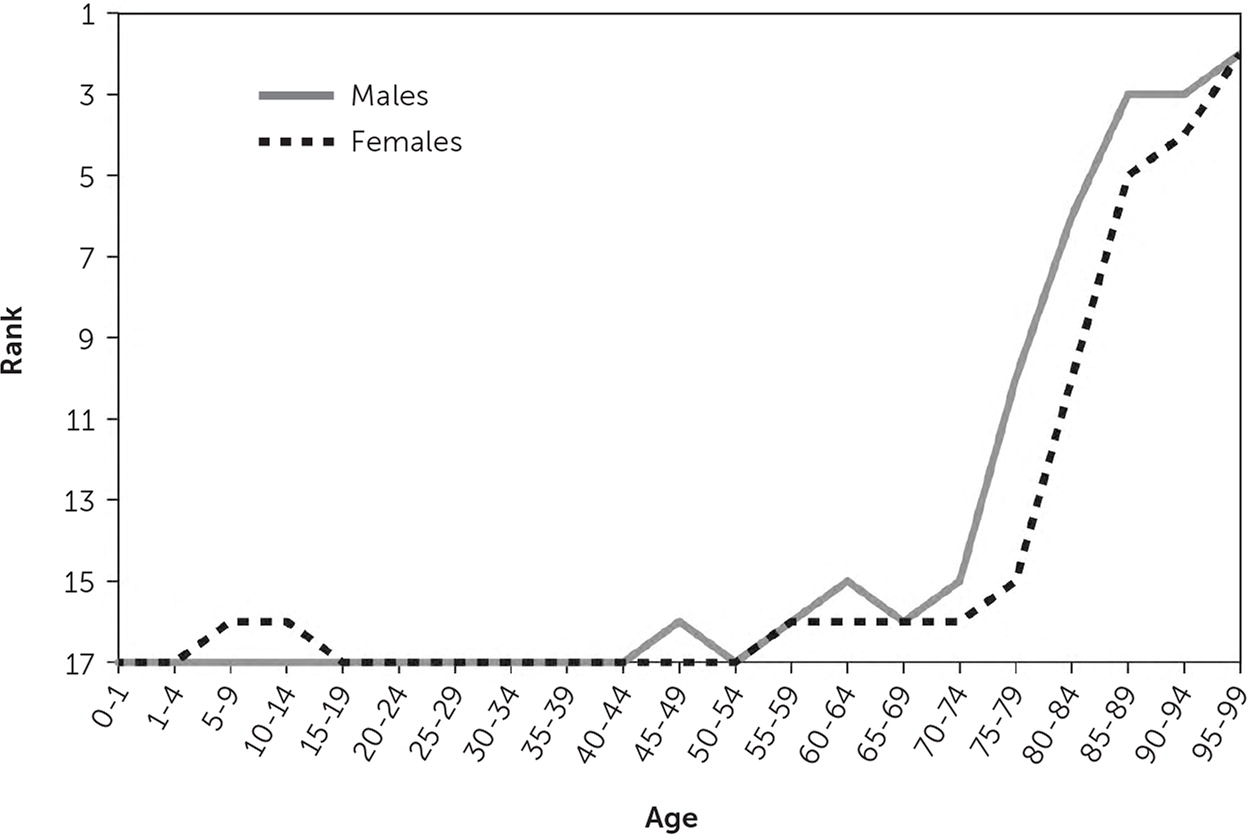
Medicare has benefits uncommon with other health insurance plans. Patients can choose from a network that includes 93% of U.S. primary care physicians.7 Once adults are eligible for coverage, their age-specific mortality increases from the worst among 17 peer nations to one of the best (Figure 1).8 The multiyear gap in life expectancy between Black and White patients who require dialysis disappears when both groups are covered by Medicare.9 Medicare also does a much better job of controlling costs compared with private health insurance: during the past decade, Medicare's cumulative increase in per-enrollee spending was 21.5%, far less than the 52.6% average increase among private insurers.10
However, Medicare is far from perfect. The reimbursement model for physicians is bewilderingly complex11; high levels of patient cost-sharing can bankrupt older adults; and the benefit design has significant gaps (dentistry, pharmacy, optometry, and audiology, among others).
The Improved Medicare for All approach addresses each of these problems through a simple concept: fix the flaws in the current program, then provide it to all Americans.12
Improved Medicare for All would provide universal access to all medically necessary care. It would obviate the need to develop emergent funding strategies to cover screening, treatment, and prevention of a single viral infection, such as COVID-19, in uninsured and underinsured patients.
How can we afford this plan? Administrative savings. Medicare operates with less than 2% overhead, whereas private health insurers often operate with more than 12%.13,14 The complexity of billing multiple payers adds tens of thousands of dollars to medical office overhead, and it diverts time from patient care to administrative tasks. Hundreds of economists declared that the United States would come out ahead economically under Improved Medicare for All.15,16
Compared with our peers in nine other countries, U.S. primary care physicians are far less satisfied with medical practice.17 A key driver of dissatisfaction is the moral indignity of knowing how to help a patient but facing insurmountable economic barriers.18 It breaks our hearts when a patient tells us, “I'll pray and wait until I turn 65 and have Medicare.” Medical bankruptcy would be scandalous in any comparable nation.19
Improved Medicare for All could help resolve the issue of excessive documentation. Electronic health records are one example of the unique administrative burdens of medical practice in the United States. A study of more than 10 million ambulatory progress notes in one record system determined that those written by clinicians in Canada, the United Kingdom, Australia, Netherlands, Singapore, and the United Arab Emirates averaged 1,000 characters; the average number of characters in notes written by U.S. clinicians was four times higher.20 Adopting a single-payer system would not automatically shorten these to global norms. However, it would mitigate two drivers of excessive documentation: complex requirements for maximal reimbursement and legal risk protection. If reimbursement requirements were more akin to global norms, physicians could document based on clinical—not economic—needs. If coverage of future medical care were guaranteed by law, patients would have fewer reasons to sue physicians.
Simplifying administrative burdens would allow more time for patient care. A 2016 study found that in some U.S. medical practices, physicians spend as little as 26% of their time with patients.21 In contrast, family physicians in Canada spend 79% of their time on patient care,22 which could be one reason that more of them report being satisfied with their practices.17
In 2018, John Cullen, MD, then-president of the American Academy of Family Physicians, described U.S. medical practice as “an incredible bureaucratic mess to get anything done for patients.”23 At the same time, Trina Larsen Soles, MD, then-president of Doctors of British Columbia, said of the Canadian system, “It's not a big hassle. I can focus on patient issues, not administrative issues.”23
Although the political obstacles are formidable, family physicians owe it to our patients and our profession to join the fight for Improved Medicare for All.
